Radiofrequency radiation is energy transmitted with a wavelength between 100 microns and 100 kilometres. This places it beyond the visible and infrared parts of the electromagnetic spectrum (figure 1). It is used for broadcasting radio and television signals, connection of internet with WiFi, communication of digital devices with Bluetooth, and the cooking of food in microwave ovens.
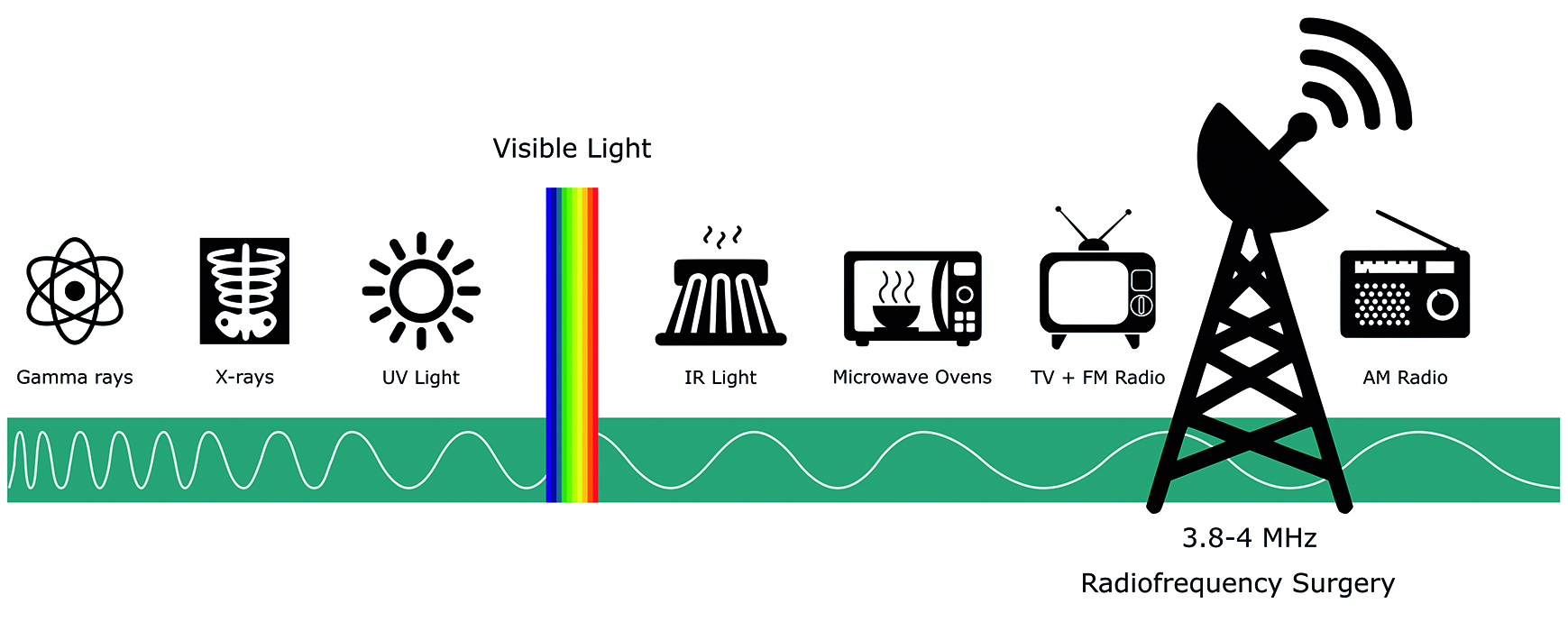 Figure 1: Radiofrequency radiation on the electromagnetic spectrum
Figure 1: Radiofrequency radiation on the electromagnetic spectrum
Radiofrequency is commonly used in dermatology, and this introduction covers its use in the removal of benign skin lesions. In this area of application, the technique is ideally suited to an in-practice procedure, owing to the rarity of serious complications, rapidity of treatment and relatively low cost. Other uses of the technique include the biopsy of suspected cancer, as an incisional tool in oculoplastic eyelid surgery, and aesthetic applications on the eyelids and adjacent skin.
How it works
With the appropriate selection of frequency and waveform, radiofrequency has a strong affinity for water. The vibration of water molecules in targeted tissues cause the frictional build-up of heat. Depending on the duration and peak value of tissue temperature the effects may be desiccation, coagulation or vaporisation.
- Desiccation refers to the loss of water from cells that leads to them becoming shrunken and shrivelled with preservation of cellular detail.
- Coagulation is the denaturation of proteins to form a coagulum, with loss of cellular definition, as all tissue structures agglutinate into a formless, homogenous mass. The term is often used in specific reference to the denaturation of the normally water-soluble blood protein albumin, where the irreversible uncoiling and the matting together of groups of these damaged molecules form an insoluble mass that plugs a blood vessel and limits bleeding.
- Vaporisation is the phase transition of water from a liquid to steam. Within the membranous confines of a cell, a rapid gaseous expansion causes it to burst. The process of vaporisation in contiguous cells results in the tissue splitting apart as though it had been cut with a razor-sharp knife. A waveform that temporally blends vaporisation with coagulation allows for simultaneous cutting and haemostasis, a bloodless dissection.
A defining feature of radiofrequency is that the probe itself is never hot. This is in contradistinction to electrocauterisation, which is analogous to a soldering iron, where heat is transferred from a scalding tip by conduction. If the probe of a radiofrequency unit were touched to a plastic bag, there would be no melting because plastic does not contain water. Radiofrequency only generates heat in the cells touched by the probe. Its probe would not directly burn fingers if pinched, rather it would cause thermal trauma from the inside out due to the reaction it generates within their moisture containing skin cells.
The clinical utility of this mode of action is that it offers the capability for extremely precise dissection with negligible lateral heat spread and, thus, surrounding tissue preservation. Consequently, there is minimal post-procedural pain, bruising, oedema or scarring.
History of thermal procedures
Battlefield medicine has used boiling oil to arrest the bleeding of wounds for thousands of years. In the practice of barber surgeons, along with blacksmiths, farriers and shoemakers, or anyone who had tools that could be repurposed, the oil was replaced by heated cauterising irons when amputating limbs, pulling teeth or for other bloody wounds. The use of high-frequency alternating electrical currents to generate heat is the basis of electrocautery that allows some refinement in control, but the rudeness of a deliberate third degree burn and its attendant sequelae persists.
Irving Ellman, a dentist and electronics engineer, began to use electrosurgery devices in the late 1960s. Their unwanted and unsightly burning and charring of thin, conterminous gingival tissue soon led to a ban in dentistry. This prompted him to experiment and discover that a frequency of approximately 4MHz in the electromagnetic spectrum of the AM radio allowed desirable tissue effects with minimal collateral damage. The Ellman radiofrequency unit was commercialised in the 1970s, and its progeny remain the most popular units (figure 2).
 Figure 2: An Ellman radiofrequency unit
Figure 2: An Ellman radiofrequency unit
Indications
Radiofrequency units are now commonly used in dermatology, surgery and gynaecology. In dermatological applications, it is especially helpful when good cosmetic results are essential and, owing to its effective control of bleeding, with highly vascularised lesions, such as capillary haemangiomas (figure 3).
 Figure 3: A capillary haemangioma. Radiofrequency is helpful in treating such highly vascularised lesions
Figure 3: A capillary haemangioma. Radiofrequency is helpful in treating such highly vascularised lesions
On the eyelid, the technique is most commonly used to remove benign lesions that are cosmetically or functionally bothersome. When this removal is undertaken through successive layers, the surgical process is termed surface ablation. When removal is achieved through a cutting process, it is termed excision. Other applications include epilation and punctal occlusion. The radiofrequency unit has also been used to create incisions (cuts) in blepharoplasty surgery.
A list of common uses and lesions treated with radiofrequency are listed in table 1.
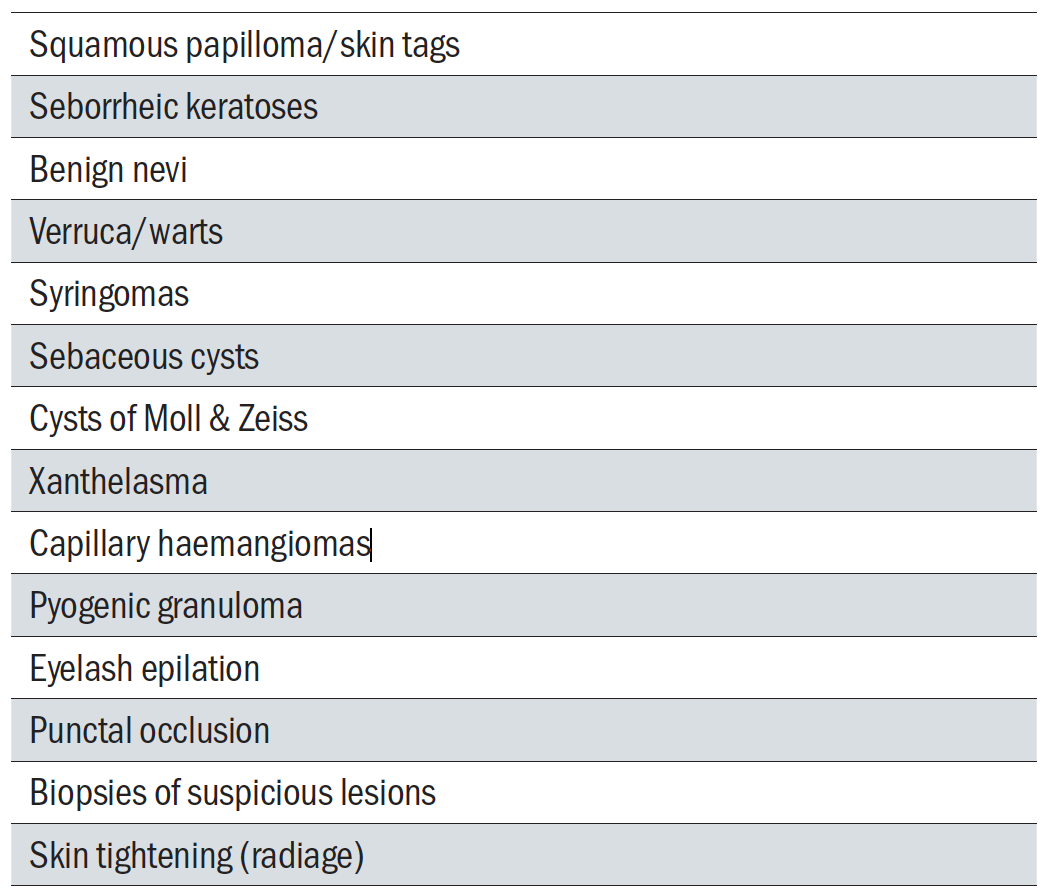 Table 1: Common uses and lesions treated with radiofrequency
Table 1: Common uses and lesions treated with radiofrequency
Contraindications
Malignant and pre-malignant lesions should not be removed by radiotherapy. This is to avoid the potential for seeding cancerous cells in healthy tissue. It is for this reason that a pigmented lesion should not be treated unless there is confidence that it is not melanoma. Such cases should always be referred to dermatology or oculoplastics for evaluation. Further management may include monitoring, excisional biopsy, wide excision or topical chemotherapy. Caution should also be applied when considering the treatment of lesions within 2mm of the eyelid margins, where any collateral damage has more functional relevance.
All use of radiofrequency around the body comes with a general warning for patients who have a cardiac pacemaker due to the theoretical risk of mediating tachycardia or even asystole. However, this is mainly when working near the heart, which is well outside even the most generous definition of ocular adnexa, and so not relevant to optometrists. Pacemakers fitted in the past few decades are also shielded to protect against externally generated currents. Notwithstanding this small risk, it is well advised to use another form of treatment if it is an option.
Ellman radiofrequency unit
The Ellman radiofrequency unit generates an electric current through the body rate at either 3.8MHz or 4MHz. Attached to the machine by a flexible cable is a handheld probe with an insulated handle and an exposed metal end. This end tip serves as an electrode to contact the skin and complete an electric circuit. The electrode may have various forms; either as a wire (straight or looped), a needle or a ball depending on the application (figure 4).
 Figure 4: A selection of electrodes for use with the Ellman radiofrequency unit, with a variety of end tips that include straight wires, wires as loops, needles and balls
Figure 4: A selection of electrodes for use with the Ellman radiofrequency unit, with a variety of end tips that include straight wires, wires as loops, needles and balls
Energy is passed as alternating current to the body at the point of contact between the electrode and the skin. It is the polarity of the current that is alternating at a radiofrequency. At this frequency, the transmitted energy is absorbed so completely by water within the touched cells that there is very little remaining to pass to the surrounding area, which gives the technique its precision. After its cellular action, the current (with much diminished energy) passes to a passive electrode plate that acts as an antenna. This grounding plate is usually placed underneath the patient, nearby to the site of surgery.
Ellman radiofrequency units are able to produce a variety of electrical waveforms. As waveforms change, so will the corresponding tissue effects. The key variable is the rate at which heat is produced, and that depends on the amount of ‘on-time’, which is termed the duty cycle (figure 5).
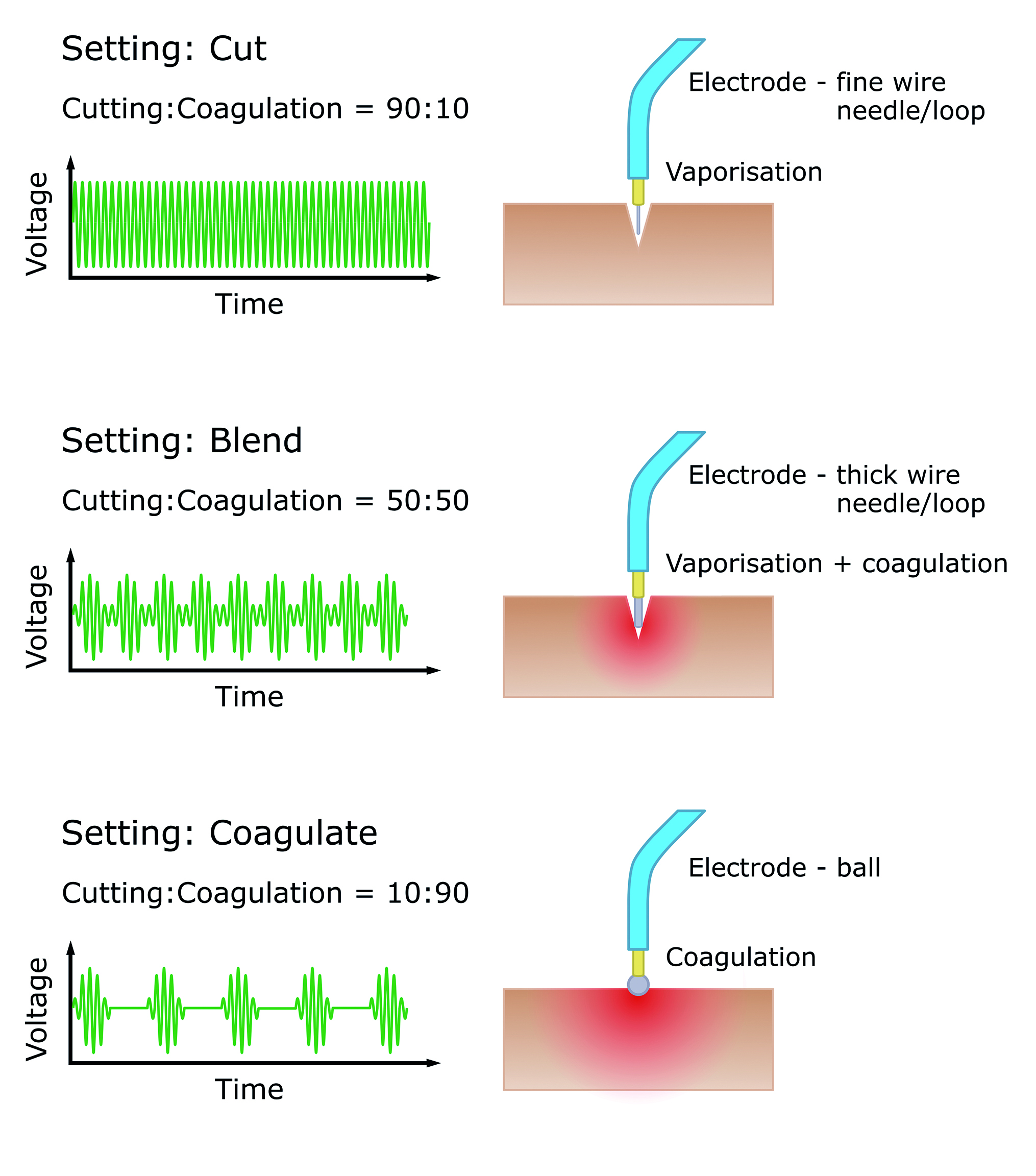 Figure 5: The various modes of action of the radiofrequency unit
Figure 5: The various modes of action of the radiofrequency unit
If electromagnetic energy is applied continuously, there is a violent increase in heat that results in vaporisation and pure cutting. With a lower duty cycle, the energy is pulsed on-off and the heating can be kept below the 100°C threshold for vaporisation, and instead the cell is cooked without exploding. This results in the coagulation of blood and melting of soft tissues. This is analogous to an egg in a microwave oven.
Ellman radiofrequency units allow for alteration of the length and spacing of pulses, which creates different electrical waveforms in three pre-set modes to give either 90% cutting, 90% coagulation or a 50:50 blend of cutting and coagulation. There is also a separate outlet that produces a spark-gap fulgurating current, for non-delicate tissue destruction through cauterisation.
In fulguration mode, the electrode is held a short distance from the skin so that there is sparking to the surface, analogous to lightning. In fact, the term fulguration comes from the Latin term fulgur, which means ‘lightning’.
To overcome the high impedance of air, the voltage is significantly higher than when cutting. The sparks heat the tissue to over 200°C for very brief periods; too short to generate the sustained rise in intracellular pressure necessary for vaporisation. Instead, the fugacious bursts enkindle tissue carbonisation. The process acts over a relatively wide area, but only superficially because it forms charred eschar (cast-off dead tissue) that insulates against heat spread to deeper layers of skin.
Smoke evacuation
When delivering radiofrequency procedures, an assistant must hold a smoke evacuator close to the site of surgery. This draws out the malodour of burning flesh. The unit should also contain a filter to safeguard against bacteria and viruses liberated from an infected patient or a viral wart. The Ellman Surg-e-Vac uses four-stage filtration to trap particles down to 0.01µm, which is more than tenfold smaller than those trapped by the best surgical facemasks, and comparable to the size of smaller viruses. An additional high-efficiency air particulate (HEPA) filter with germicidal UVC light may also be considered for the treatment room as part of a ventilation system or portable air purifier.
Clinical work-up
Clinical diagnosis with eyelid lumps and bumps is often as much divination as it is diagnosis. However, the primary matter of point with any eyelid lesion in clinic is not discerning what it is exactly, but whether the possibility of cancer or a pre-malignant lesion meets a threshold of concern. Detecting malignancy is more important than the proper naming of benignity.
The key questions that should be asked are listed in table 2, and the most important of all relate to reported changes in appearance or size, which is the calling card of cancer. When examining an eyelid lesion, we should review the ‘ABCDE’ features, which were devised for melanomas but have general applicability, and look for the aberration or destruction of adjacent structures, such as the absence of nearby eyelashes (table 3).
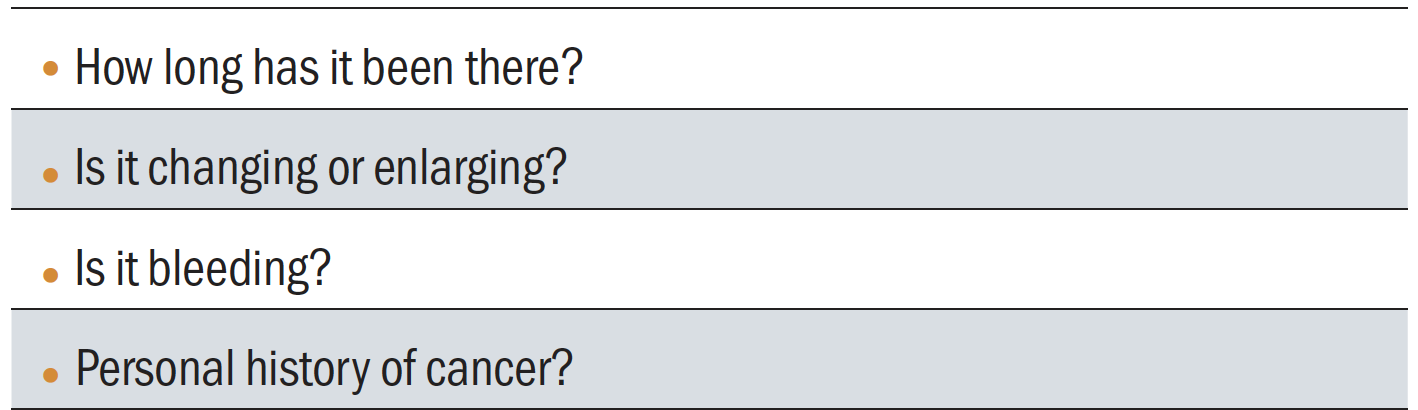 Table 2: Key questions to ask when a patient has an eyelid lesion
Table 2: Key questions to ask when a patient has an eyelid lesion
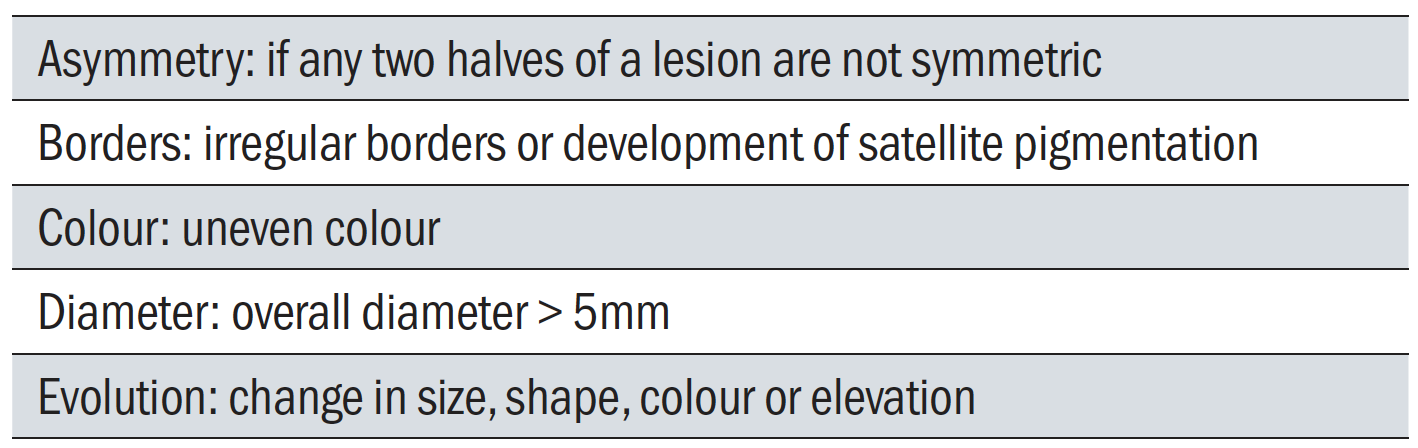 Table 3: ‘ABCDE’ signs concerning for malignant transformation of a nevus into melanoma
Table 3: ‘ABCDE’ signs concerning for malignant transformation of a nevus into melanoma
If you are uncertain, watch actively. Cancer changes. Malignancy moves. You just need to be there to catch it early before it gets organised. The fundamentals of navigating the grey zone of uncertainty with eyelid lesions are timing of follow-up, photo-documentation and humility. Sharing with a patient that there are signs of concern, along with the possible diagnosis, is also important so they appreciate that there is a justifiable reason for an early review that is not contingent on their vision.
Pre-operative procedure
Consent is particularly important with advanced clinical procedures that involve risk. The process starts at the initial consultation when the treatment plan is first discussed with the patient, but should be confirmed on the day. It must cover the
following:
- Diagnosis of condition for treatment
- Expected outcome of treatment procedure
- Outcome from alternative of non-treatment and doing nothing
- Duration of process
- Cost of treatment
- Details of follow-up required
There must also be full disclosure of common side-effects and any rare, but serious, possible complications.
In law, consenting is a process rather than a signed piece of paper but, without written records, there is no evidence of any process. It is also recommended for medicolegal purposes that photographs are taken before and after all procedures.
On the day of treatment, measurements should be taken of visual acuity, blood pressure and pulse. Medical history should be reviewed, and the patient must be asked specifically about known allergies to iodine, anaesthetics or antibiotics. The lesions to be treated should be verbally confirmed with the patient. It must also be confirmed that they are willing to proceed, and they should be told that treatment can stop at any time if they
request this.
Anaesthesia is required for most radiofrequency procedures, and this can be topical or infiltrative. All but the most superficial lesions are more comfortable if the area is anaesthetised with a subcutaneous injection of lidocaine 1% or 2%. The inclusion of epinephrine is standard, unless it is medically contraindicated, to reduce the likelihood of bleeding and to prolong the duration of anaesthesia. The eyelids are well suited for receiving local anaesthetic because of the potential space between the epidermis and dermis. The formed bolus is dissipated by massage. It will take five to 10 minutes to take effect.
The skin is cleansed with povidone-iodine 10% in an aqueous solution, or a similar surgical preparation formula. It should be allowed to dry for at least three minutes.
Some clinicians like to use a corneal shield to protect the cornea from accidental contact. Alternatively, the eyelid can just be pulled down and held in place with a thumb. A corneal shield is of more use when lesions are close to the eyelid margins, or when a high power is being used.
Surgical technique
During a radiofrequency procedure, the patient is usually lying on their back, or similarly reclined in a chair, with the optometrist behind them. After the Ellman radiofrequency unit is switched on, the appropriate electrode is fitted to the handle, and the waveform and power are selected. The antenna plate should be placed on the operating table, positioned near the operative site. This plate does not have to make skin contact, but should be under the patient.
During surgery, the power is adjusted based upon the tissue response. The aim is to keep the power to the minimum required to limit collateral heat damage. Any sparking indicates that the power is too high and should be reduced. If the electrode is dragging, then it is likely that the power should be increased, though this may also occur if the skin is too dry or if the electrode has collected tissue and needs to be wiped clean.
Making cuts
A straight or looped wire electrode is used to make incisions with the Ellman radiofrequency unit set to deliver 90% cutting. If there is bleeding, this can be switched to the blend setting. It is often helpful to lightly moisten the skin with a piece of wet gauze because this facilitates its cutting action. The probe is held near the perpendicular to the tissue site. Using the fingers to create a gentle tension on the skin can facilitate the incision. During the actual cutting, it is important to use a smooth uninterrupted motion with even and light pressure. The movement should not be too slow. If it is, the build-up of lateral heat in the tissue may cause charring, followed by necrosis and sloughing.
The biggest difference, and the most important thing to be learned, is that radiosurgery cuts without pressure, unlike scalpel blades, and so a light, smooth, continuous brush-like stroke should be developed. When incising the electrode should always be kept moving at between 5 to 8mm per second.
Removing lumps
Lesions on a stalk, like a pedunculated papilloma (figure 6), are easily removed by gently pulling upwards to create tension on the stalk, and then cutting with the looped electrode on a cut or blend setting. Care should be taken not to exert too much pull that will lead to a wound gaping on release of the upward tension. Better to be left with a stump that can be smoothed afterwards.
 Figure 6: Two presentations of pedunculated papilloma
Figure 6: Two presentations of pedunculated papilloma
When approaching larger, broad-based, elevated lesions, consideration should be given to initially debulking with a blade in a shaving fashion. The loop electrode can then be used in superficial passes, gradually moving downwards, until the lesion is smoothed out. This produces excellent cosmetic results, especially when the edges are feathered. Another advantage is that any tissue removed can be sent to pathology with no burn artifact.
Flat lesions
When the lesion is essentially flat, or has a stuck-on plaque morphology, such as some naevi or seborrheic keratosis, they can be ‘melted’ away using the 90% coagulation setting and an electrode with a ball tip. The electrode is used with a light tapping motion to remove the lesion that fades as if touching-up a picture in Photoshop.
Control of bleeding
Excessive bleeding is almost never a problem in radiosurgery when used for eyelid lesions because there is always some haemostasis with cutting and the blood vessels involved are small. However, if there is excess bleeding, then this should be stopped by some form of direct pressure. Then, most of the blood should be dabbed away before capillaries or larger vessels are sealed by the repeated use of a wider tip or ball electrode with a coagulation setting.
Cauterisation
The fulguration mode of the Ellman radiofrequency unit is used to destroy warts and the base of cysts. It is delivered using an electrode with a thick tip. It is quite different to the other modes that rely on direct contact with the target tissue. Instead, when fulgurating, the electrode is held a short distance above the surface. This gap allows for the creation of electrical arcs between the tip of the electrode and the skin. An electrical storm in miniature.
Hair follicle epilation
The Ellman radiofrequency unit can be used to permanently burn the germinal cells of eyelash follicles, which is a more permanent alternative to mechanical epilation. It targets single eyelashes, and so is most applicable when there are only a few aberrant lashes. It is thus more comparable to electrolysis, rather than cryotherapy. The advantage over electrolysis is that there is less collateral tissue damage, but a downside is that it is more demanding of accurate electrode positioning and so treatment may take longer.
The technique uses a special electrode that is very thin and insulated down its entire shaft to the very end. Anaesthetic is often not needed. The small gauge wire of the electrode is introduced alongside the lash and slid 2 to 3mm down to the follicle. On reaching the end a stop is felt, whereupon the radiofrequency signal is delivered on the 90% coagulation setting for about one second to destroy the hair follicle. The eyelash is then given a light tug and should come out. It often does not budge, which indicates that the follicle was missed. In this situation, the process is repeated until it does. A combination of a highly focused effect and blindness in aiming can be frustrating.
Post-procedure
Immediately following the procedure, the surgical site should be cleaned with an antiseptic and an antibiotic ointment is applied. Blood pressure and pulse are checked. The patient is educated with regard to moist healing for the next few days.
The clinical notes need to document what was done, any complications, and the instructions the patient was given on wound healing and follow-up.
Summary
Optometrists hold a significant role in diagnosing and managing their patients’ ocular health. There is a clinical need and a market demand for being able to provide full scope eye care in a local setting. For many patients there is at present no option of having lumps, bumps and marks that bother them removed. Being limited to offering reassurance that a lesion is just benign and is not bad enough to meet the NHS treatment criteria of functional disability or cosmetic disfigurement should not be accepted without challenge.
Radiofrequency is a versatile tool that is ideally suited to use in appropriate community settings. Optometrists who are willing to step-up to educate themselves and accept the responsibility are well placed to provide this service.
- Dr Michael Johnson is a specialist IP optometrist based in an independent community practice in South Gloucestershire with a current interest in developing advanced optometric skills, including laser treatment and anterior eye and adnexal therapies.
