Contact lenses provide our patients with significant lifestyle and optical benefits for sport and vocational activities, and for myopia control. Contact lens related complications only occur in the minority of contact lens wearers and reassuringly these are mostly mild in nature, resolving on removal of the lenses.1 As eye care practitioners (ECPs), understanding research in this area allows us to minimise the risks of potential complications, both by the products we prescribe and the advice we give.
The purpose of this report is to examine and summarise the recent BCLA CLEAR publication on contact lens complications and link them to everyday practice.
What is a contact lens related complication?
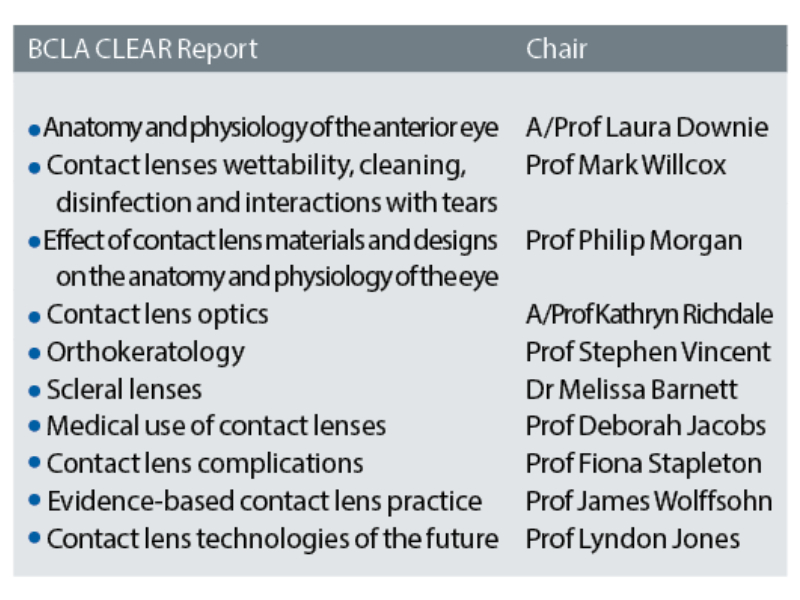
Various adverse events can occur directly due to contact lens wear, this excludes incidences that occur concurrently. These are usually symptomatic and requires some form of intervention, which can range from simply a temporary discontinuation of contact lens wear to pharmacological or medical involvement 1. For further clarity, the BCLA CLEAR classifies them as seen in table 1 and figure 1.
Corneal infections
Corneal infections or microbial keratitis (MK) are rare but potentially serious complications of contact lens wear. They account for between 35-65% of the total number of cases seen within hospitals and in working aged adults, two thirds of the total number of cases seen are contact lens or trauma related.1
While the last reported estimate of the incidence of contact lens related MK was made over 10 years ago so may not align entirely with the current numbers, these numbers have been robust for the past 30 years. Unsurprisingly, the risk of corneal infection varies with modality, and the highest risk of 20 cases per 10,000 was linked to overnight wear of soft lenses.1 The lowest risk was the daily use of soft lenses and daily rigid corneal lens use.1
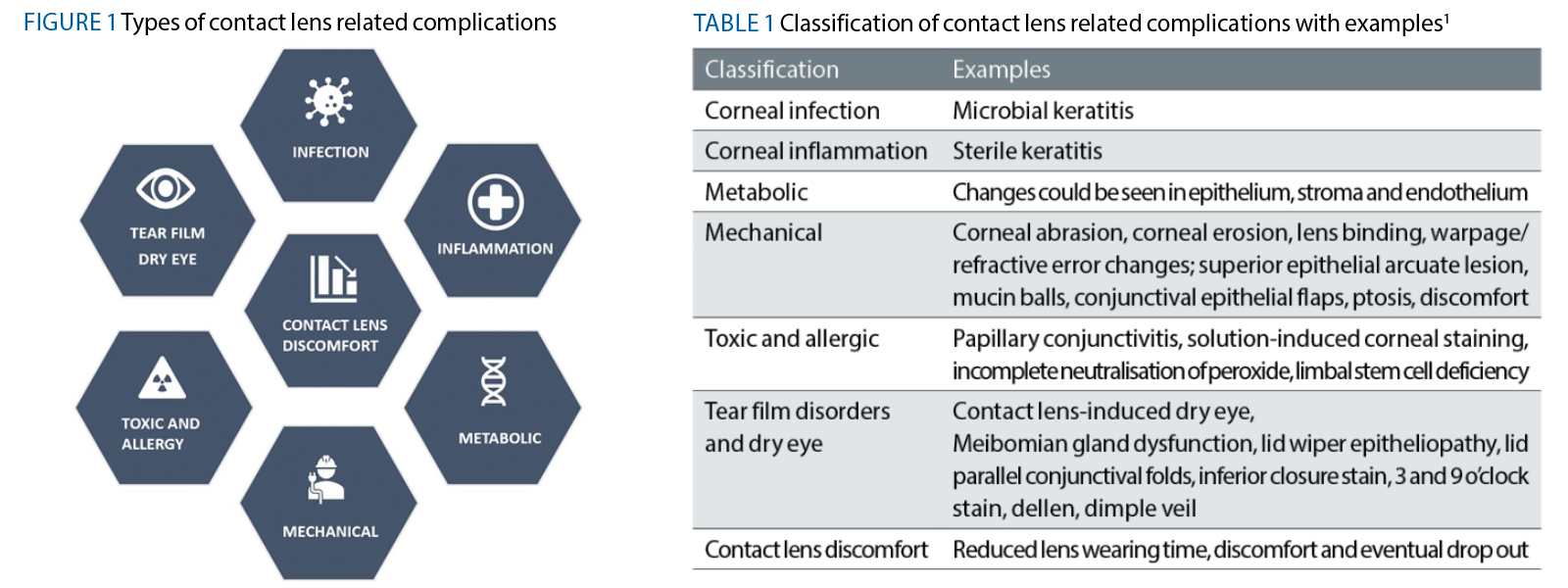
Most contact lens related infections are caused by bacteria, the most common being Pseudomonas aeruginosa, but there are regional variations. The remaining 5 to 15% are caused by free-living protozoa such as Acanthamoeba spp and fungi such as Fusarium spp1 (figure 2).
Figure 2: Microbial keratitis due to Fusarium spp (left) and Acanthamoeba spp (right)
Some risk factors for MK are not modifiable such as age and gender, but the good news for the contact lens practitioner is that their role in minimising these risks are relatively simple and very effective. The practitioner should provide the patient with the appropriate information when they fit the lenses and reiterate at all aftercare appointments.
The steps to minimising contact lens related infections:
- Avoidance of overnight wear
- Avoidance of water exposure
- Attention to hand, lens and case hygiene
- Attention to other risk factors – male sex, young age, smoking
- Fit with daily disposable lenses where possible
- Ensure that patients understand that they should seek help early. Early presentation to an eye care practitioner reduces the risk of more severe disease2
Daily disposable modality is linked to less severe microbial keratitis and fewer cases of corneal infiltrative events (CIEs). If daily disposable wear is not possible, then only fitting scheduled replacement lenses is the next best thing, and using hydrogen peroxide solution as opposed to multipurpose solution also reduces the risk of sterile keratitis (also known as CIEs).
For reusable lenses careful consideration should be given to the lens storage case, given there are often lower levels of best practice compliance reported and the potential for biofilm build up. The introduction of simple mechanical cleaning intervention steps such as rubbing the case followed by rinsing, tissue wipe and leaving to air dry have been found to remove nearly 90% of the bacterial load. A reminder of regular replacement of cases and solutions is also important.
Practitioners also need to be confident in their ability being to distinguish between the sight threatening MK and a CIE in order to ensure the appropriate treatment is accessed as quickly as possible.
Corneal infiltrative events (CIEs)
CIEs are often asymptomatic making them easier to distinguish from the more symptomatic presentations associated with MK.1 They can also sometimes however be accompanied by mild to moderate pain and a red, watery eye, which is then more challenging to correctly identify.
Differential diagnosis
An important characteristic is that with a temporary break from lens wear, symptoms will reduce in a CIE, but will increase in MK.1 Their size and location are key also as a CLPU will typically be <1mm in diameter and located in the periphery or mid periphery.
- An important characteristic is that with a temporary break from lens wear, symptoms will reduce in a CIE, but will increase in MK.1
- Their size and location are key also as a CLPU will typically be <1mm in diameter and located in the periphery or mid periphery.
Risk is lowest with daily disposables and highest in overnight wear of reusable soft lenses. Although these lesions are not infectious, the appropriate treatment is generally considered to be a combination of topical prophylactic antibiotics and steroids.1
Metabolic complications
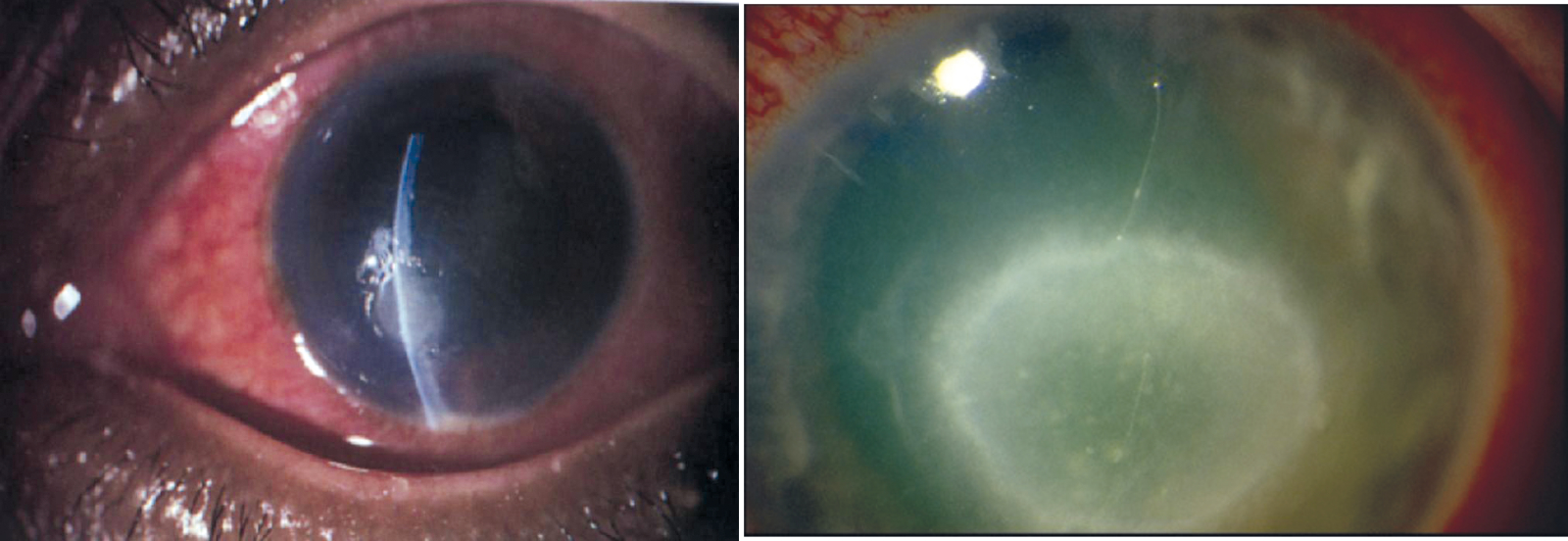
Metabolic stress of the cornea is influenced by both the oxygen transmissibility of the contact lens and the tear exchange. The evolution of lens materials has reduced the frequency that this complication is observed in contact lens practice, but as these high Dk materials are not universally prescribed, it does still feature to some degree.1 Signs of hypoxia are quite distinctive at each stage depending on the level of hypoxia being induced, and can potentially alter the appearance and function of all the corneal layers1 (table 2 and figure 3).
Table 2: Hypoxic complications4
Figure 3: Hypoxic complications. (a) epithelial microcyst. (b) stromal oedema showing as striae. (c) neovascularisation. (d) Endothelial changes
Mechanical contact lens induced complications
Corneal abrasions and erosions
Contact lens related corneal and conjunctival abrasions or erosions can result from a deposited or damaged contact lens or debris trapped between the lens and the cornea. They are typically superficial and can be managed with lubricants once the initial cause has been identified and removed.1
Lens binding
Lens binding is generally described in relation to rigid corneal lens wear, in particular ortho-k, but it has been reported across a wide range of materials and modalities. If a corneal erosion accompanies lens binding, caution should be observed due to the link with microbial keratitis.3 Lens binding is usually resolved with re-fitting the lenses and increasing the frequency of replacement.1
Corneal warpage
Corneal warpage can be induced by hypoxia, but has also been known to be induced by the resting place of a contact lens, causing temporary changes that can be detected by topography. It usually self resolves on cessation of lens wear.1
Superior epithelial arcuate lesions (SEALS)
SEALs (figure 4) are largely associated with high modulus soft lenses such as some of the first generation silicone hydrogel (SiHy) lenses. Incidence has reduced as the practice of fitting lower modulus SiHy lenses has increased. It typically resolves on temporary discontinuation of lens wear.1
Mucin balls
Mucin balls (figure 5) can be seen in hydrogel lens wearers, but are more common in wearers of high modulus SiHy lenses. It also appears to be linked to patients with steeper corneal geometry, which suggests a link to the way the contact lens fits. It is still unclear whether there is any clinical significance attached to the presence of mucin balls.1
Figure 4: (left) A superior epithelial arcuate lesion (SEAL); Figure 5: (right) Mucin balls
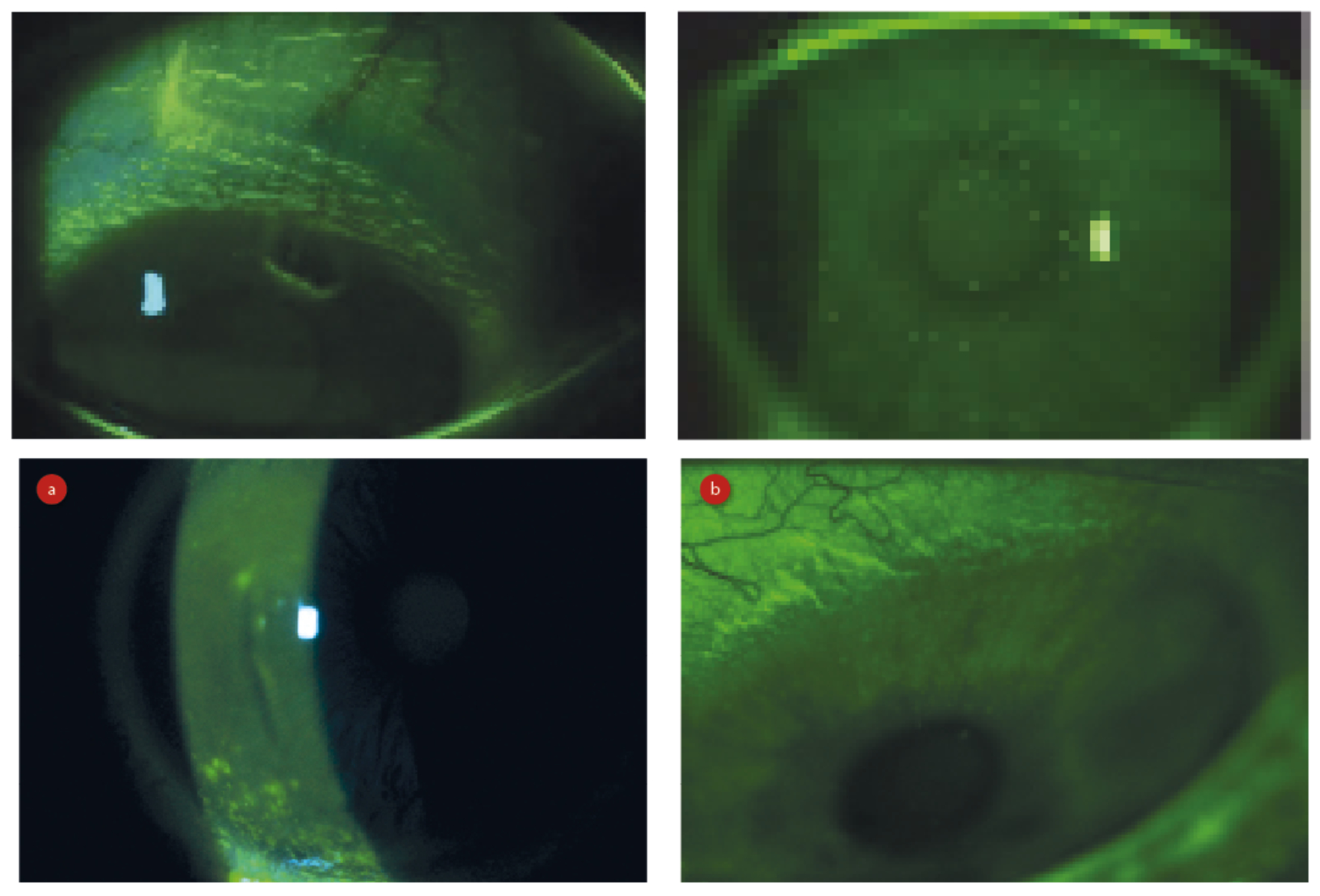
Figure 6: (a) CLIDE, (b) CLADE
Contact lens induced dry eye
Contact lens induced dry eye (CLIDE) affects 15 to 55% of contact lens wearers and refers to patients experiencing symptoms of dryness that resolve on lens removal. Influential factors include population, lens material and assessment criteria.1 If symptoms of dryness are present with or without contact lenses, it is known as contact lens associated dry eye (CLADE). According to the TFOS DEWS II reports, global prevalence of dry eye disease (DED) ranges between 5 and 50%, and is more common among contact lens wearers than non-wearers4 (figure 6). This leads to the consideration that contact lens wear is a modifiable risk factor for dry eye disease.1
Both CLIDE and CLADE are multifactorial in nature,1 contributing factors include material, water content, lens design, modality, replacement schedule, duration of lens wear and environmental factors. Patient factors such as gender and ethnicity also play a part.1
Modifiable risk factors are important to understand here too as soft contact lens wearers have a higher incidence of CLIDE than rigid corneal lens wearers.1 Furthermore, CLIDE occurs more frequently in hydrogel wearers compared with wearers of SiHy contact lenses. High water content contact lenses have also been proposed as a potential risk factor for CLIDE, which is likely to be a consequence of contact lens dehydration and local thinning of the tear film (figure 7). Additionally, poor wettability has also been strongly associated with dry eye symptoms and unsurprisingly, symptoms increase with longer wearing times. Environmental factors have also been suggested to increase the risk of CLIDE, including raised temperature and reduced humidity as well as screen use. Patients with 3 and 9 o’clock staining or incomplete blinking are also more likely to report symptoms of CLIDE.
Management of CLIDE centres around managing any pre-existing tear film issues and refitting the patient with SiHy lenses,1 daily disposable SiHy or rigid corneal lenses.
Figure 7: Localised thinning of the tear film
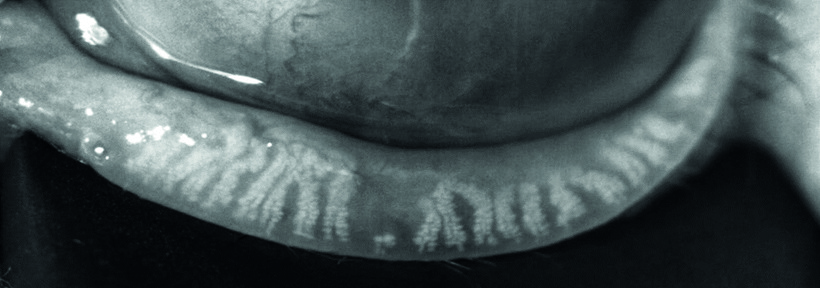
Meibomian gland dysfunction in contact lens wear
The 2011 TFOS International Workshop defined meibomian gland dysfunction as ‘a chronic, diffuse abnormality of the meibomian glands, commonly characterised by terminal duct obstruction and/or qualitative/quantitative changes in the glandular secretion. It may result in alteration of the tear film, symptoms of eye irritation, clinically apparent inflammation and ocular surface disease’.5 The condition leads to evaporative dry eye and has been linked to the primary cause of contact lens discomfort in at least 14% of cases.5 It is also a common observation in contact lens practice (figure 8).
Can soft contact lens wear affect meibomian glands?
- Can change the structure and function of the glands
- Can alter expressibility and quality of secreted meibum
- Can lead to gland losses
- Associated with increased lid margin vascularity, irregularity and plugging of gland orifices
Figure 8: Meibomian gland drop-out shown by meibography
Contact lens discomfort
Contact lens discomfort is an important area for the contact lens practitioner as it is the most common reason for contact lens dropout, with around 50% of wearers reporting discomfort during contact lens wear.1 There are many elements that contribute towards this including patient factors such as lid conditions and contact lens factors such as lens design and thickness. Higher levels of discomfort have been linked to high water content lenses and lenses with a higher modulus and the report states that there is no difference in comfort between hydrogel and SiHy lenses, but more dryness is reported with hydrogel lens wear.1 Other factors influencing contact lens discomfort can be related to the lens design, deposits or a higher level of post blink movement. The ideal fit is well centred without excessive movement and with an edge design that minimises interaction between the lens and the lids and bulbar conjunctiva.1
The role of the contact lens solution in contact lens comfort has been examined and some combinations of lens and lens care system provide greater levels of comfort. Peroxide was also compared with multipurpose solutions and while some differences between comfort on application and overall comfort, there was no significant difference overall, but avoiding PHMB based solutions can help to improve contact lens discomfort in some cases.
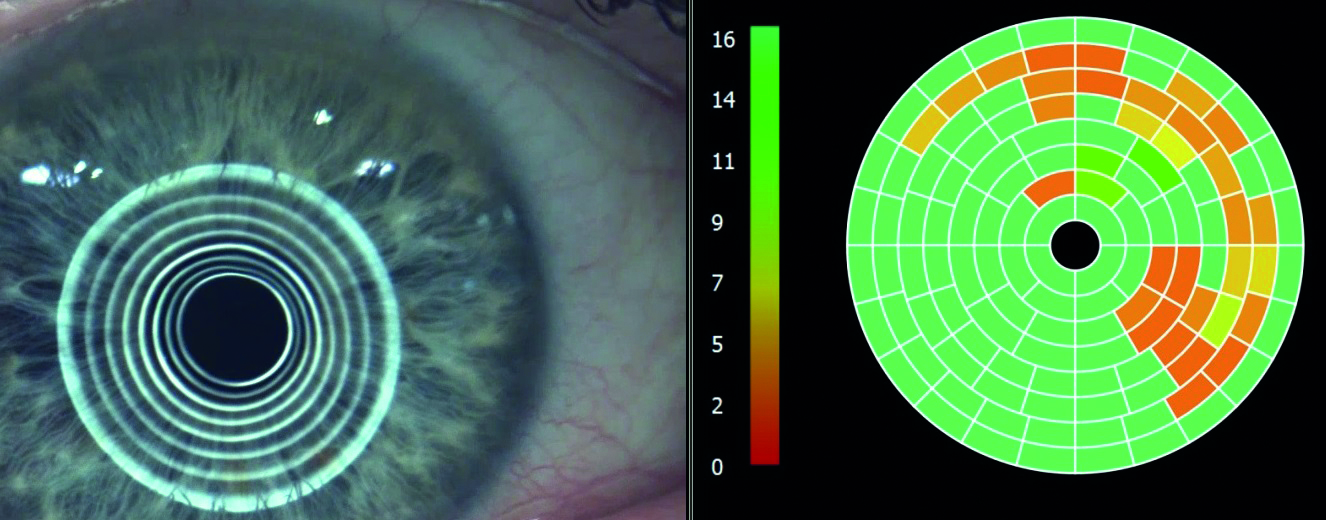
Orthokeratology
Orthokeratology is the process of fitting a rigid lens for overnight wear to mould the cornea (figure 9). It can be used to correct myopia, hyperopia, presbyopia and astigmatism. It has been used ‘off label’ for myopia control and there is now a CE marked product for this purpose also. The risk of MK varies across age ranges, but as a whole is around 7.7 per 10,000 eyes per year, which is similar to overnight use of soft lenses.1
Other complications linked to orthokeratology are similar to those observed with other types of contact lenses and were generally considered to be mild. Corneal neovascularisation occurred in less than 5% of patients and corneal erosions or abrasions were retrospectively counted as one in 21 wearers. Corneal staining was recorded in one study to be mild and minimal (less than grade 1) and occurred in eight out of 66 wearers.1 For a more comprehensive review of orthokeratology, read the BCLA CLEAR-Orthokeratology publication.6
Figure 9: An orthokeratology lens in situ
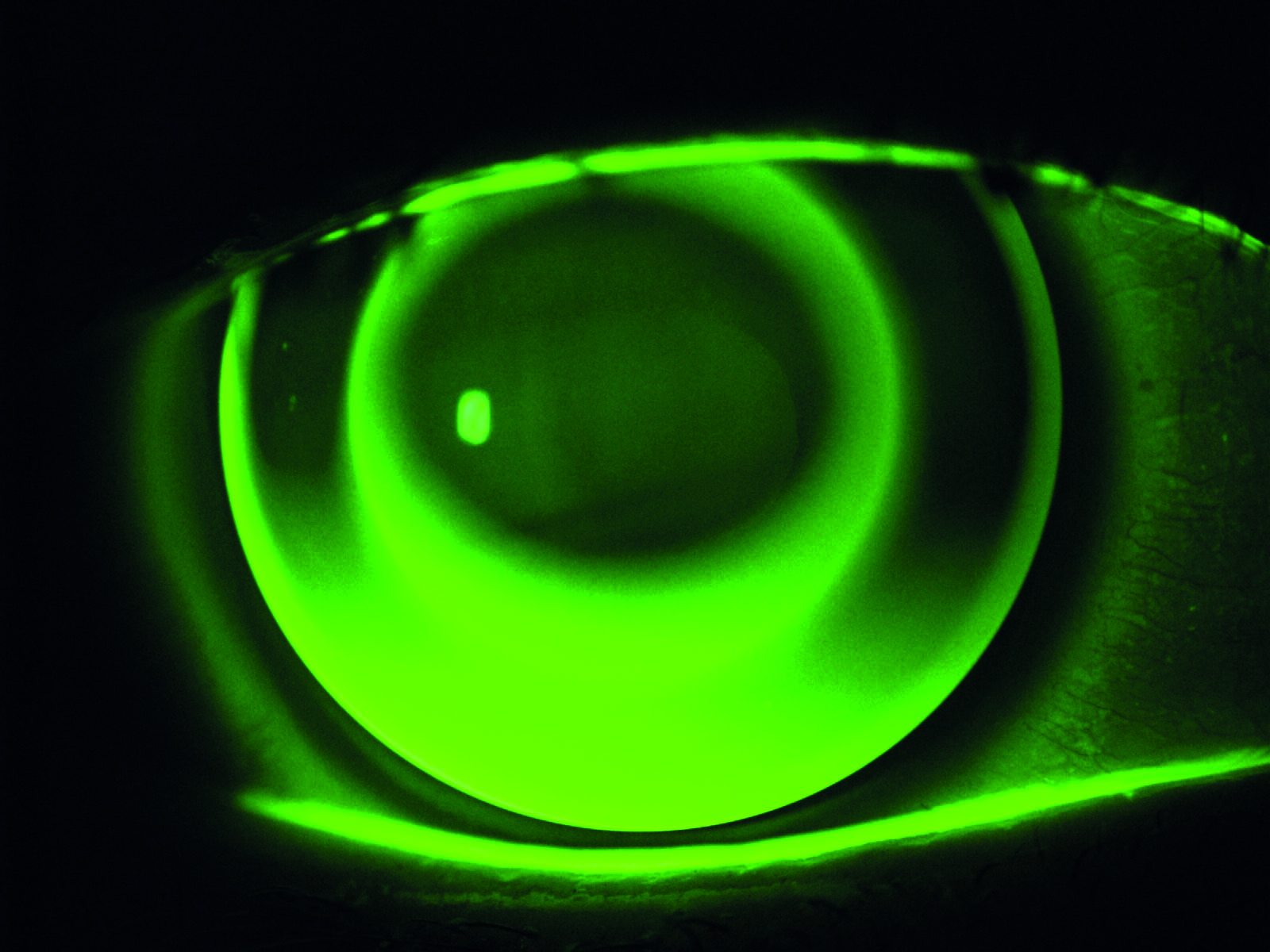
Scleral lenses
Mid-day fogging is the most common visual complication associated with scleral lens wear, noted between 16-85% of wearers. Similar to other lenses, scleral lens wear can be rarely associated with microbial keratitis and infiltrative keratitis. Other complications could be related to hypoxia such as endothelial bleb response, mechanical complications such as corneal bullae, corneal staining (figure 10), increased corneal sensitivity, conjunctival staining (figure 11) and redness. Much of the complications related to scleral lens wear was associated with hypoxia, which has significantly reduced due to the recent use of high DK lens materials. More detailed guidance on scleral lenses is provided in the BCLA CLEAR-Scleral lens publication.7
Figure 10: (left) Scleral lens in situ with inferior central bearing causing (right) corneal staining
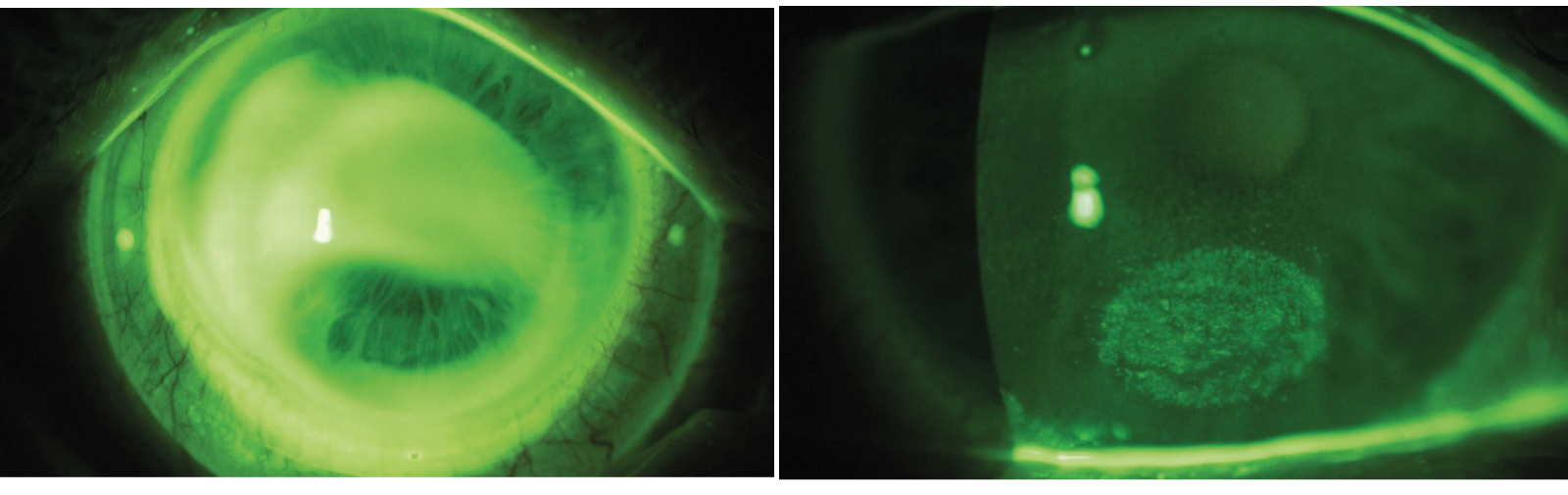
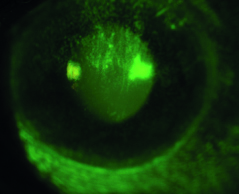
Figure 11: Conjunctival stain after scleral lens removal
CPD Exercise
The multiple choice questions for this CPD article can be found at opticianonline.net and concern the assessment and management of the following two cases.
Case study 1
A 34-year-old male patient presents for an unscheduled aftercare complaining of a sore right eye for the last few days. He has been unable to wear his lens but the eye still feels like it is getting worse without lens wear too. He is photophobic and has some noticeable oedema of the right eyelid. The left eye is asymptomatic.
Slit lamp examination reveals a 2mm circular lesion 3.5mm away from the limbus with fuzzy edges which stains with fluorescein. He also has grade 2 MGD.
His lenses are monthly replacement and he is unsure exactly how old they are or how old the case is. He admits he only sometimes rubs and rinses and thinks he may have slept for a few hours in them at the weekend.
Case study 2
A 25- year-old woman presents for a routine aftercare appointment on her monthly disposable SiHy lenses, reporting occasional grittiness over the last few weeks in the left eye. It has not stopped her wearing the lenses.
She is a smoker and has a long standing history of blepharitis, and generally adheres to contact lens related compliance well.
Slit lamp examination reveals a 1mm circular lesion. It is located 1mm in from the limbus between 4 and 5 o’clock with clearly defined edges and some fluorescein staining.
Conclusion
In summary, contact lenses provide patients with many optical and lifestyle benefits. Prescribing them brings patient loyalty and a regular, reliable contribution to the turnover of an optical practice and is interesting and rewarding for the eye care practitioner. The risks associated with contact lens wear are small, often mild in relation to the benefits and frequently resolve on removal of lenses. The risks can be minimised by being proactive with educating patients on lens care and hygiene practices and continuing to monitor their compliance during aftercare appointments.
Pauline Bradford is a contact lens optician with a wide range of experience, both in practice and in professional services. She currently divides her time between lecturing in optometry at the University of Plymouth and is the Academic Link Tutor between Canterbury Christ Church University and ABDO college. She is also an examiner for ABDO and occasionally works in practice.

- The full report and supplementary information can be accessed at https://doi.org/10.1016/j.clae.2021.02.010
- The BCLA CLEAR Summary report is a short bite-size evidenced based practical guide for clinicians, bringing together the key findings from the report. Accessed via CLEAR (bcla.org.uk)
The editors for this series are Neil Retallic and Dr Debarun Dutta.
Acknowledgements
Acknowledgement and recognition to Fiona Stapleton F, May Bakkar, Nicole Carnt, Robin Chalmers, Ajay Vijay, Sanjay Marasini, Alison Ng, Jacqueline Tan, Heidi Wagner, Craig Woods, James Wolffsohn who were the paper’s authors and the educational grants from Alcon and CooperVision.
The author would like to thank Professor Fiona Stapleton and Dr Nicole Carnt for kindly reviewing of this article.
Original paper: Stapleton F, Bakkar M, Carnt N, Chalmers R, Vijay A K, Marasini S, Ng A, Tan J, Wagner H, Woods C, Wolffsohn J S BCLA CLEAR-Contact Lens Complications Contact Lens and Anterior Eye 44 2021 330-367.
References
- Stapleton F, Bakkar M, Carnt N, Chalmers R, Vijay AK, Marasini S, et al. CLEAR - Contact lens complications. Cont Lens Anterior Eye_ 2021;44(2):330-67. https://doi.org/10.1016/j.clae.2021.02.010.
- Keay L, Edwards K, Naduvilath T, Taylor HR, Snibson GR, Forde K, et al. Microbial keratitis predisposing factors and morbidity. Ophthalmology 2006;113(1):109-16. https://doi.org/S0161-6420(05)01031-6.
- Willcox MD, Carnt N, Diec J, Naduvilath T, Evans V, Stapleton F, et al. Contact lens case contamination during daily wear of silicone hydrogels. Optom Vis Sci 2010;87(7):456-64. https://doi.org/10.1097/OPX.0b013e3181e19eda.
- Stapleton F, Alves M, Bunya VY, Jalbert I, Lekhanont K, Malet F, et al. TFOS DEWS II Epidemiology Report. The ocular surface 2017;15(3):334-65. https://doi.org/10.1016/j.jtos.2017.05.003.
- Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo CK, et al. TFOS DEWS II Definition and Classification Report. The ocular surface 2017;15(3):276-83. https://doi.org/10.1016/j.jtos.2017.05.008.
- Vincent, S.J.; Cho, P.; Chan, K.Y.; Fadel, D.; Ghorbani-Mojarrad, N.; González-Méijome, J.M.; Johnson, L.; Kang, P.; Michaud, L.; Simard, P.; et al. CLEAR - Orthokeratology. Contact lens & anterior eye : the journal of the British Contact Lens Association 2021, 44, 240-269, doi:10.1016/j.clae.2021.02.003.
- Barnett, M.; Courey, C.; Fadel, D.; Lee, K.; Michaud, L.; Montani, G.; van der Worp, E.; Vincent, S.J.; Walker, M.; Bilkhu, P.; et al. CLEAR - Scleral lenses. Contact lens & anterior eye : the journal of the British Contact Lens Association 2021, 44, 270-288, doi:10.1016/j.clae.2021.02.001.
