There is increasing interest in myopia management within the eye care professional (ECP) community. This positive step is largely due to advances in clinical research and the evidence-base supporting why myopia management should become the standard of care for childhood myopia, in addition to more optical interventions becoming available to the public. As the science and education in this field is rapidly evolving, it is understandable that certain theories may be replaced or superseded by new evidence in a relatively short time. This is also an emerging field of practise for many eye care professionals (ECPs), with many clinicians in the process of building up their knowledge and expertise to help serve these young patients in optical practice.
This article will identify common questions, or myths, surrounding myopia management to help support ECPs with their clinical confidence and competence in this subject matter.
MYTH 1: SLOWING MYOPIA BY ONE DIOPTRE WON’T MAKE ANY DIFFERENCE
There are multiple benefits to having lower levels of myopia, including better uncorrected visual acuity, better corrected visual acuity and less dependence on one’s correction (figure 1).

Figure 1: Types of contact lens related complications
Furthermore, lower myopes are better refractive surgery candidates by virtue of the need to remove less corneal tissue and the expectation of less residual post-surgical refractive error (figure 2).2
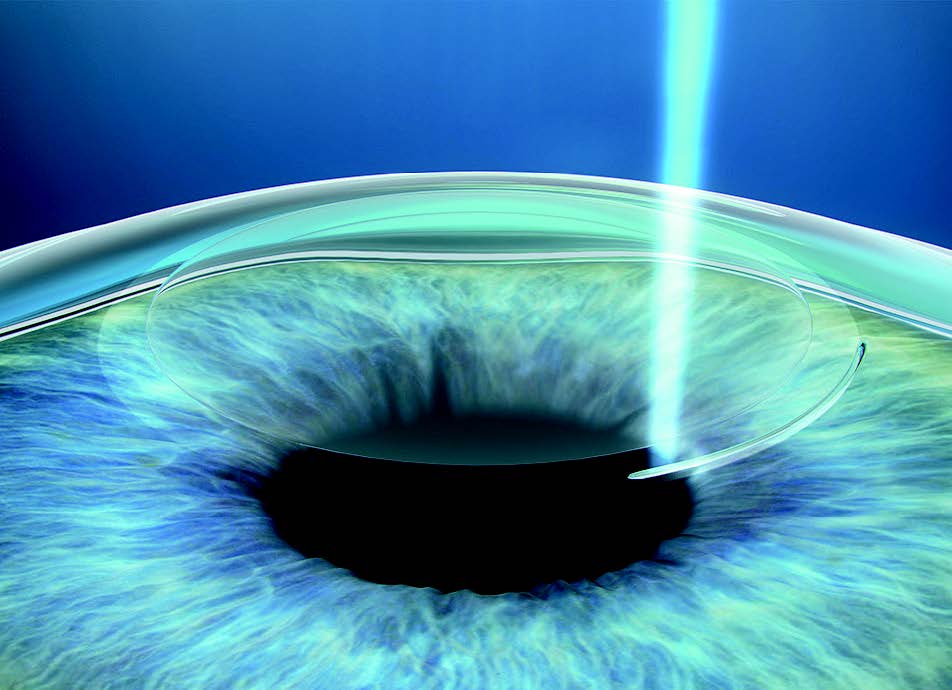
Figure 2: Lower myopes are better refractive surgery candidates
The greatest virtue of less myopia, however, is the reduced risk of eye disease and visual impairment.3 At university we learned that myopia was a risk factor for retinal detachment, open-angle glaucoma and some forms of cataract (figure 3).
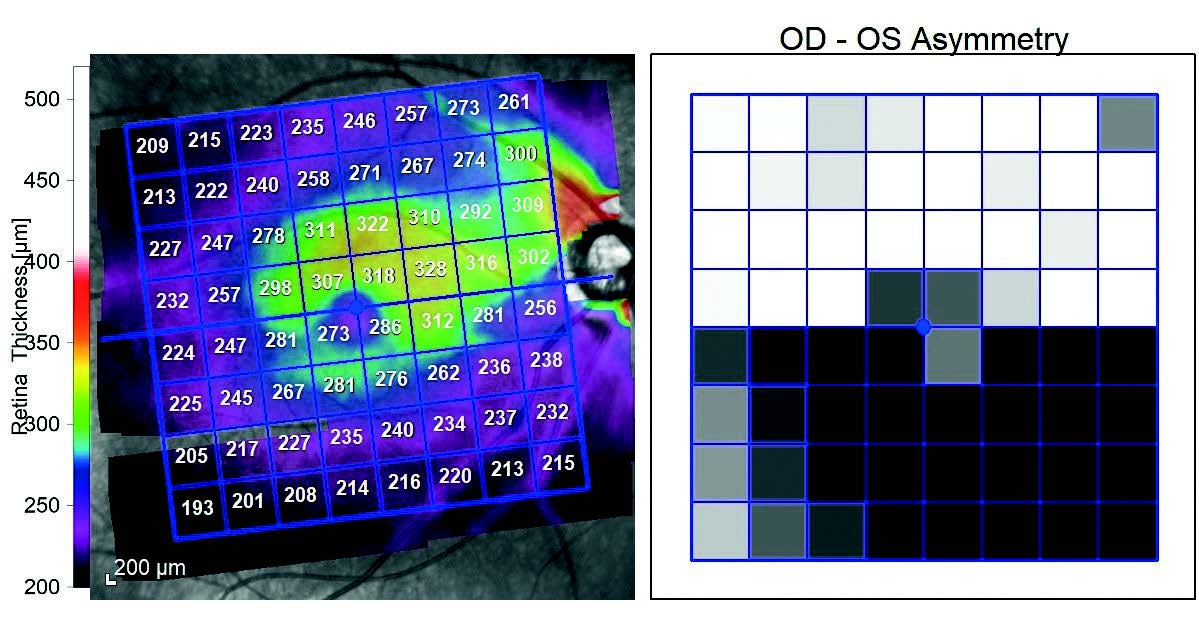

Figure 3: Myopia has long been associated with several causes of sight loss, including (a) primary open angle glaucoma (top), (b) cataract (middle) and (c) rhegmatogenous retinal detachment (bottom)
We also learned about myopic degeneration, since renamed as myopic maculopathy (figure 4).4 With the increasing prevalence of myopia and its severity, myopic maculopathy is climbing up the league table of causes of untreatable visual impairment and will be the single greatest threat to vision by the middle of this century.5-7 Currently, there is no treatment.
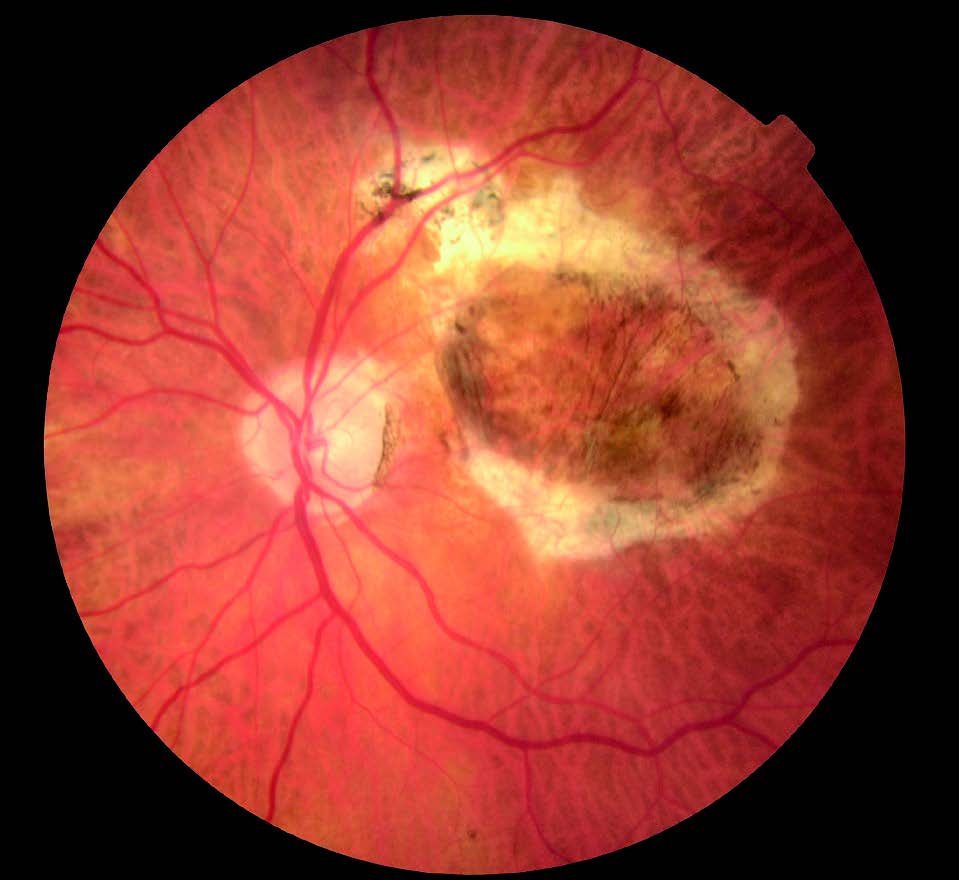
Figure 4: Myopic maculopathy is climbing up the league table of causes of untreatable visual impairment
The relation of each dioptre of myopia and the risk of myopic maculopathy was recently quantified using data from over 20,000 patients from five studies across three continents.1 Each additional dioptre of myopia increases the risk of myopic maculopathy by an astonishing 67%.1 Likewise, each dioptre less lowers the risk by 40%.1 Furthermore, myopic maculopathy is not a disease of high myopia, it is a disease of myopia as half of the cases occur in myopes below -5.00DS, because there are many more of us around.8,9 As Professor Ian Flitcroft says: ‘There is no safe level of myopia.’ Myopic maculopathy develops much earlier than other age-related macular disease, so patients have to live with the disease for longer.10
There has recently been shown to be a similar relationship between all causes of visual impairment and dioptres of myopia based on data from 15,000 Dutch patients.11 Whether you are 55 or 75 years old, each additional dioptre of myopia increases the risk of visual impairment by 25%.3 Likewise, each dioptre less lowers the risk by 20%.3
In summary, we should care about long-term visual health of every myopic child and not just address their current visual needs. With the range of myopia management options available to us, we have the potential to slow myopia progression by at least a dioptre and make a huge public health impact.
TAKE HOME MESSAGE
Each dioptre saved has the potential to significantly reduce the risk of sight-threatening pathologies later in life.
MYTH 2: 0.50DS PER YEAR IS NORMAL MYOPIC PROGRESSION
The rate of myopia progression is too varied to assign a single value (figure 5). The two most important factors contributing to this variability are age and race, with the number of myopic parents also playing a role. With respect to age, in the Correction of Myopia Evaluation Trial (COMET), a three-year clinical trial of progressive addition lenses (PALs) for myopia progression, children in the single vision lens group who were six or seven years old at baseline progressed twice as fast as the 11-year-olds: -2.19DS vs -1.04DS over three years.12 Donovan et al published a review of the myopia progression rates.13 The estimated progression rates were dependent on baseline age, with decreasing progression with age. Brennan et al reported corresponding data for axial elongation.14 In myopic children of European descent the rates at eight and 11 years are around 0.3 and 0.2mm/year, respectively.14
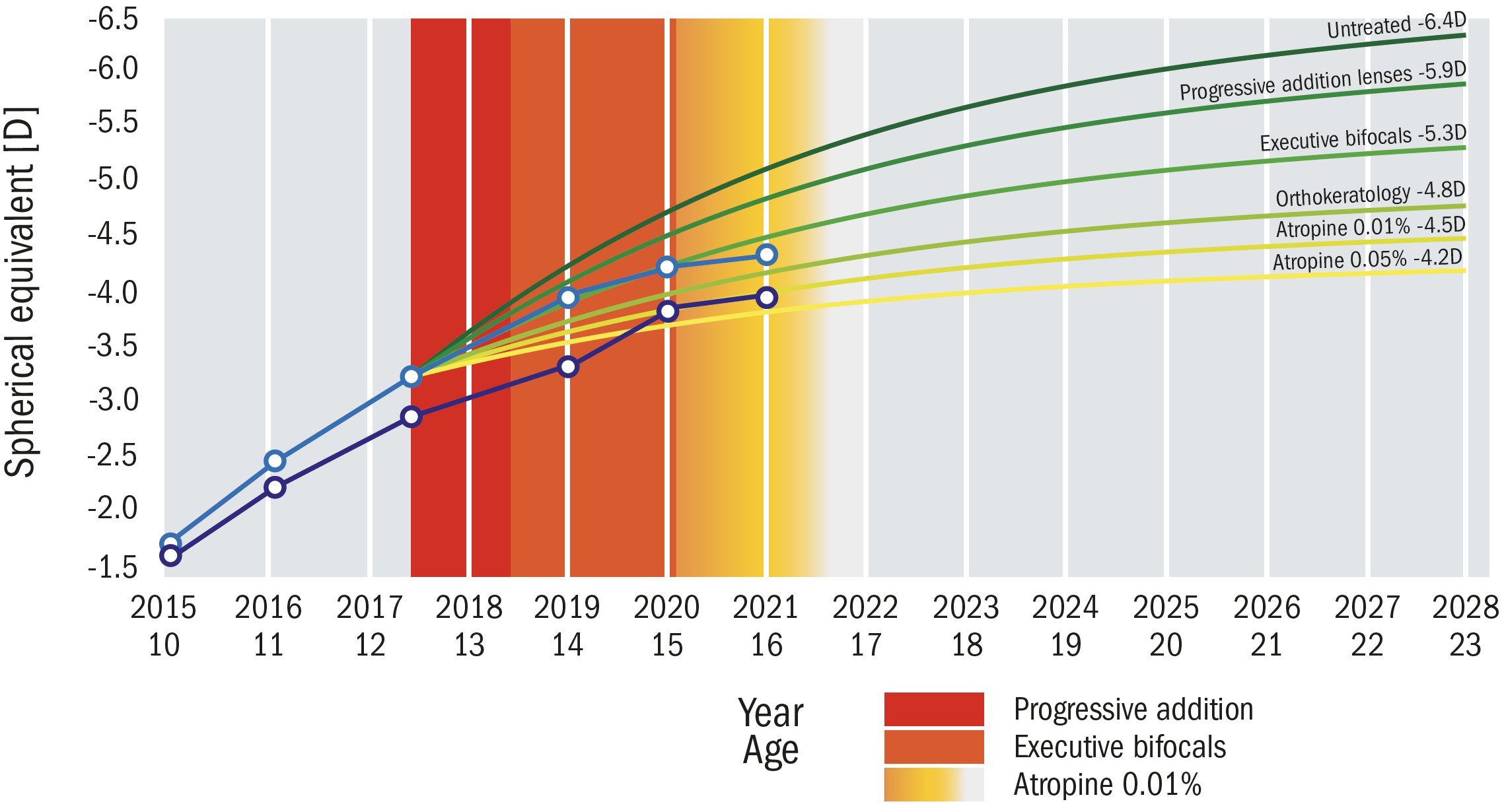
Figure 5 :The myopia curves for the right (blue line) and left (purple line) eyes for three successive interventions. 1. Progressive power lens. 2. Executive bifocal. 3. Atropine 0.01%
Ethnicity is another significant factor, with myopic children in Asian countries progressing faster than those in western countries. Donovan et al estimated annual myopia progression in nine-year-olds to be -0.55 DS for populations of predominantly European extraction and -0.82 DS for East Asians.13 In other words, the East Asian children progress 50% faster. This same ratio holds for axial elongation.14 Regardless of the variations in progression rate, there is no evidence that treatment effect varies with ethnicity.15,16 Many studies report that parental history of myopia increases the incidence and prevalence of myopia in children,17,18 but there are fewer studies of the effect of parental history of myopia on the progression of myopia.19 Among Singaporean myopic children aged six to 12 years,20 the mean progression rate for those with at least one myopic parent was -0.63 DS per year compared to -0.42 DS per year for those whose parents were not myopic. In a subset of children in the COMET Study, children with two myopic parents progressed faster over five years than those with zero or one myopic parents by -0.78DS and -0.55DS, respectively.19
In summary, we should avoid talking about normal or average progression of myopia. It varies too much with age, race and family history. In fact, even when we account for these factors, progression rates vary. This makes care of the individual patient challenging as we will never know what would have happened, had we not intervened.
TAKE HOME MESSAGE
Regardless of age of onset, ethnicity, parental history or lifestyle, we should assume a young myope is going to progress, rather than waiting for it to happen.
MYTH 3: MYOPIA STABILISES AT AGE 15
First, it must be acknowledged that around a third of cases of myopia do not even appear until after the age of 15 years. For example, in a US study of 396 myopic adults between 25 and 35 years of age, 37% developed myopia at the age of 15 years or thereafter based on self-report.21 In a UK study of 1,224 twins between 18 and 86 years of age of whom 347 were myopic, 28% of the myopes reported having their first spectacle or contact lens correction at the age of 18 years or older, nearly all between the ages of 18 to 30 years.22
Studies of juvenile-onset myopes do show that the average age of stabilisation is around 15 years,23,24 but as we know, not all children are average, although most believe that their own are above average. The most comprehensive report was an extension of the Correction of Myopia Evaluation Trial (COMET). The researchers were able to estimate the age and amount of myopia at stabilisation in 426 of their original cohort – a large ethnically diverse group of 469 myopic children.24 The mean age at myopia stabilisation was 15.6±4.2 years (note the huge standard deviation), and the mean amount of myopia at stabilisation was -4.87±2.01 DS. Participants with two myopic parents were around 1.00DS more myopic at stabilisation than those with no myopic parents, but did not differ in age at stabilisation. The mean age at stabilisation is similar to a previous estimate, but contrary to Goss and Winkler,23 there was no significant difference between the sexes.
In a subsequent paper, the group reported on the stabilisation of axial elongation in the same cohort with similar conclusions.25 Age at stabilisation was 16.3±2.4 years. Age at stabilisation was not associated with ethnicity, sex or number of myopic parents, but axial length at stabilisation was associated with sex and number of myopic parents, but not ethnicity. The COMET authors24 noted a large variation in age of stabilisation of refractive error:
- 48% of the cohort had stable myopia by age 15 years
- 77% of the cohort had stable myopia by age 18 years
- 90% of the cohort had stable myopia by age 21 years
- 96% of the cohort had stable myopia by age 24 years
In other words, around half of juvenile onset myopes are still progressing at 15 years and a quarter continue progress into adulthood.
These data are important when setting reasonable expectations for the duration of myopia management with each patient. As discussed above, the rate of myopia progression decreases with age and some amount of progression may be acceptable, particularly after several years of myopia management, but that is for discussion among practitioner, patient and parent.
TAKE HOME MESSAGE
If a teenager is happily wearing a myopia management soft lens, then why not have them continue until you are confident that refractive error is stable? Also, while we have limited data, managing myopia that develops in the late teens should be considered.
MYTH 4: LAST YEAR’S PROGRESSION ALLOWS ME TO MAKE INFORMED DECISIONS ABOUT MANAGEMENT OPTIONS
Many eye care professionals state they use a patient’s previous progression to decide whether or not to initiate myopia management. 26 As discussed above, there are several factors that influence rate of progression, so if this leads you to initiate myopia management in young patients, then that is not a bad thing. Nonetheless, if you use past progression as your criterion, you will be missing a lot of patients deserving of myopia management. Why? Because progression in consecutive years is poorly correlated. Data from clinical trials show a poor correlation between progression in the first and second year.27 Likewise, 916 myopes in the Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) study showed virtually no relation between progression in consecutive years.28 Furthermore, judging the success of your intervention based on the prior year is problematic. There can be an illusion of great treatment success due to a combination of natural reduction in progression with age, regression to the mean (someone who is above average in one year is likely to be closer to, or lower than, average the next year), and initial spike in real treatment efficacy.27
TAKE HOME MESSAGE
Consider treating all young myopic children, rather than basing your decision on previous progression.
MYTH 5: YOUNG CHILDREN CANNOT HANDLE CONTACT LENSES
The typical age at which optometrists introduce contact lenses is between 10 and 12 years of age.29,30 In the brave new world of myopia management, we need to recalibrate and there are good reasons to do so. Numerous studies have demonstrated that children as young as eight years can be successfully fit with soft contact lenses.16,31-35 The most comprehensive compared fitting and follow-up in eight to 12-year-old children and 13 to 17-year old teenagers.34 The authors enrolled 84 children and 85 teens and over 92% completed fitting and three months of wear in both groups. The mean total chair time for children was 111 minutes compared with 95 minutes for teenagers. Most of the difference was due to application and removal training: 42 minutes for children and 30 minutes for teenagers. The authors conclude that ECPs should consider routinely offering contact lenses as an option, especially for young myopic children from eight years old as these are the potential high myopes of the future. This has been borne out in studies of soft lens myopia management where children as young as seven or eight have been successfully fit.16,36 Start introducing the topic early, particularly when a family member, particularly a parent, is an established contact lens wearer. And if you are worried about additional chair time, it will not be much and it may be time to delegate application and removal to a staff member.

Figure 6: Numerous studies have demonstrated that children as young as eight years can be successfully fit with soft contact lenses
TAKE HOME MESSAGE
Do not consider age a contraindication when it comes to contact lens fitting, particularly for myopia management.
MYTH 6: VISION IS WORSE WITH MYOPIA MANAGEMENT OPTIONS
Some of us have had mixed experiences with different types of contact lenses and this may lead to similar expectations in children wearing lenses designed for myopia management. This is a flawed assumption for two reasons. First, children may be more visually tolerant than adults. For example, they do not drive at night and have clear media. Second, a number of studies have shown that visual acuity is unaffected by myopia management devices.16,37-39 Conventional visual acuity is unaffected by overnight orthokeratology or MiSight 1 day wear although more stringent measures (low contrast letters and dilated pupils) may reveal differences.37,39 In the three-year MiSight 1 day clinical trial, visual acuity was equivalent in the two groups and 80% or more of MiSight 1 day wearers reported seeing really well. The lens has a concentric dual-focus design, but when asked about ‘ghosting,’ less than half the wearers noticed them and few found it ‘annoying’.40 Adapted single vision soft lens wearers moving to myopia management designs may require a little adaptation.
TAKE HOME MESSAGE
Most children respond very well to myopia management options. Their delight at wearing a comfortable daily disposable soft lens will outweigh any minor visual symptoms.
MYTH 7: IT’S IMPOSSIBLE TO PRACTICE MYOPIA MANAGEMENT WITHOUT BEING ABLE TO MEASURE AXIAL LENGTH
In clinical trials of myopia progression and control, axial length is the metric of choice for assessing efficacy for a number of reasons. 27 Expert panels state that both cycloplegic auto-refraction and optical biometry are acceptable outcome measures, but show a preference for the latter.41-42 The advantage of measuring axial length with modern optical instruments is that no cycloplegia is required. Ultrasound requires topical anaesthesia, contact with the cornea, and is far less repeatable than optical biometry.
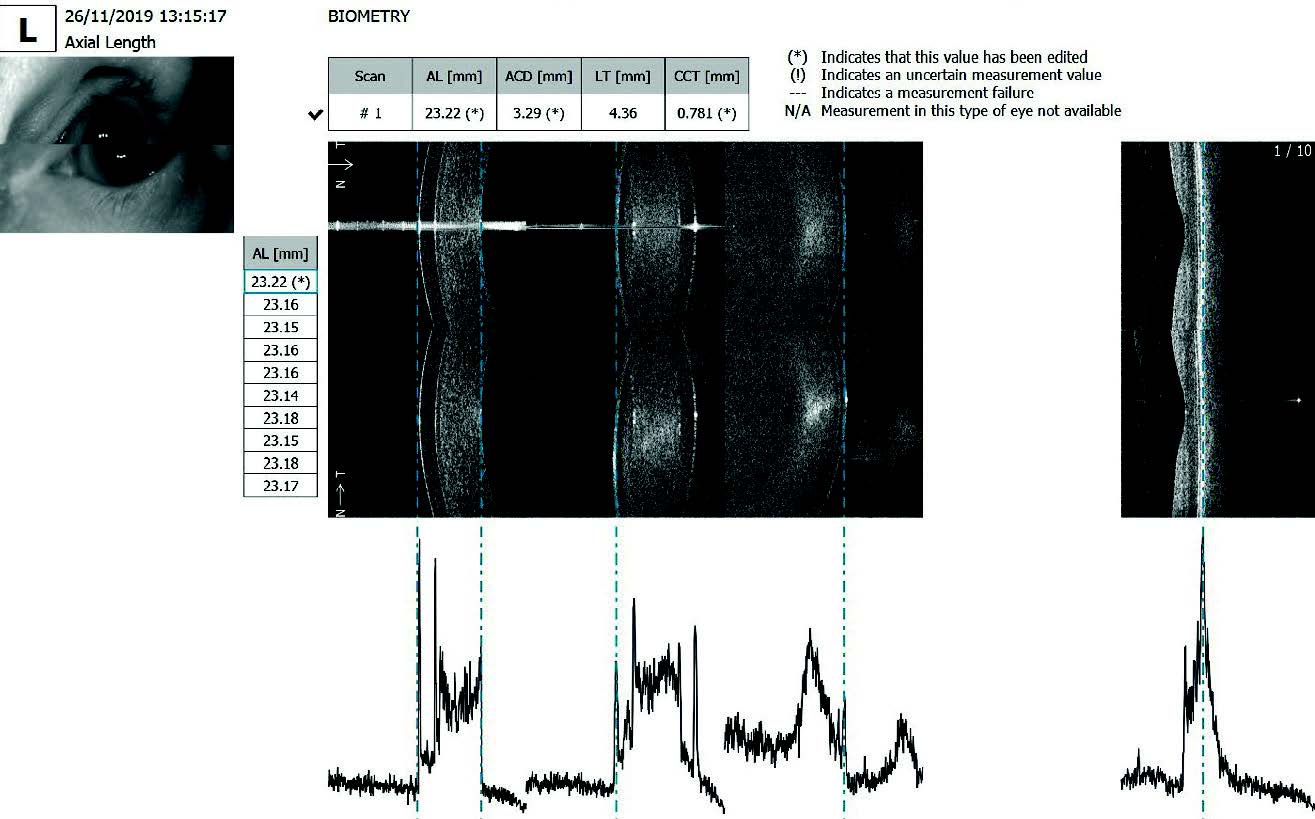
Figure 7: The advantage of measuring axial length with modern optical instruments is that no cycloplegia is required
Speaking of repeatable, the exquisite precision of instruments like the IOLMaster (Carl Zeiss Meditec) and Lenstar (Haag- Streit) makes axial length measurements more repeatable than refraction. Unfortunately, such instrumentation is not cheap. There may come a time when axial length measurement becomes the standard of care for myopia management, but that time is not now. When managing myopia using soft contact lens or spectacle modalities, refraction, preferably under cycloplegia and with an auto-refractor, is an acceptable way to monitor progression. In the three-year MiSight 1 day clinical trial, myopia progression and axial elongation were highly correlated.16
TAKE HOME MESSAGE
Axial length measurement is not mandatory for myopia management but there are caveats. Some myopia management interventions influence the optics of the eye independently of axial length, most notably overnight orthokeratology. The only accurate way to monitor myopia progression in overnight orthokeratology is with axial length measurement.
SUMMARY
In closing, young, myopic children can be offered a range of clinically useful myopia management options that have the potential to reduce the risk of visual impairment later in life, rather than solely correct their refractive error. Myopia should no longer be considered an inconvenience, but a manageable condition with a narrow window of opportunity to control its progression to have the biggest impact. With organisations like the World Council of Optometry introducing clinical guidance for ECPs, there is no question that myopia management should be the standard of care for childhood myopia.
Professor Mark Bullimore writes about myopia and other topics, is an adjunct professor at the University of Houston, a consultant for Alcon Research, Allergan, CooperVision, Essilor, Eyenovia, Genentech, Johnson & Johnson Vision, Novartis, Presbia and Vykuma and owner of Ridgevue Publishing, Ridgevue Technologies and Ridgevue Vision. Dr April Jasper practices in West Palm Beach, Florida, USA. She is an American Academy of Optometry fellow and is chief optometric editor of Optometric Management.
This article was supported by an educational grant from CooperVision, Inc.
REFERENCES
- Bullimore MA, Brennan NA. Myopia Control: Why Each Diopter Matters. Optom Vis Sci 2019;96:463-5.
- Bailey MD, Olson MD, Bullimore MA, et al. The Effect of Lasik on Best-Corrected High-and Low-Contrast Visual Acuity. Optom Vis Sci 2004;81:362-8.
- Bullimore MA, Ritchey ER, Flitcroft DI, et al. The Risks and Benefits of Myopia Control. Ophthalmology 2021;128:1561-1579.
- Ohno-Matsui K, Kawasaki R, Jonas JB, et al. International Photographic Classification and Grading System for Myopic Maculopathy. Am J Ophthalmol 2015;159:877-83 e7.
- Hsu WM, Cheng CY, Liu JH, et al. Prevalence and Causes of Visual Impairment in an Elderly Chinese Population in Taiwan: The Shihpai Eye Study. Ophthalmology 2004;111:62-9.
- Iwase A, Araie M, Tomidokoro A, et al. Prevalence and Causes of Low Vision and Blindness in a Japanese Adult Population: The Tajimi Study. Ophthalmology 2006;113:1354-62.
- Liang YB, Friedman DS, Wong TY, et al. Prevalence and Causes of Low Vision and Blindness in a Rural Chinese Adult Population: The Handan Eye Study. Ophthalmology 2008;115:1965-72.
- Vongphanit J, Mitchell P, Wang JJ. Prevalence and Progression of Myopic Retinopathy in an Older Population. Ophthalmology 2002;109:704-11.
- Wong YL, Sabanayagam C, Ding Y, et al. Prevalence, Risk Factors, and Impact of Myopic Macular Degeneration on Visual Impairment and Functioning among Adults in Singapore. Invest Ophthalmol Vis Sci 2018;59:4603-13.
- Cohen SY, Laroche A, Leguen Y, et al. Etiology of Choroidal Neovascularization in Young Patients. Ophthalmology 1996;103:1241-4.
- Tideman JW, et al. Association of Axial Length with Risk of Uncorrectable Visual Impairment for Europeans with Myopia. JAMA ophthalmology 2016;134:1355-63.
- Hyman L, Gwiazda J, Hussein M, et al. Relationship of Age, Sex, and Ethnicity with Myopia Progression and Axial Elongation in the Correction of Myopia Evaluation Trial. Arch Ophthalmol 2005;123:977-87.
- Donovan L, Sankaridurg P, Ho A, et al. Myopia Progression Rates in Urban Children Wearing Single-Vision Spectacles. Optom Vis Sci 2012;89:27-32.
- Brennan NA, Cheng X, Toubouti Y, Bullimore MA. Influence of Age and Race on Axial Elongation in Myopic Children. Optom Vis Sci 2018;95:E-abstract 180072.
- Berntsen DA, Sinnott LT, Mutti DO, Zadnik K. A Randomized Trial Using Progressive Addition Lenses to Evaluate Theories of Myopia Progression in Children with a High Lag of Accommodation. Invest Ophthalmol Vis Sci 2012;53:640-9.
- Chamberlain P, Peixoto-de-Matos SC, Logan NS, et al. A 3-Year Randomized Clinical Trial of MiSight Lenses for Myopia Control. Optom Vis Sci 2019;96:556-67.
- Zadnik K, Satariano WA, Mutti DO, et al. The Effect of Parental History of Myopia on Children’s Eye Size. JAMA 1994;271:1323-7.
- Lim DH, Han J, Chung TY, et al. The High Prevalence of Myopia in Korean Children with Influence of Parental Refractive Errors: The 2008-2012 Korean National Health and Nutrition Examination Survey. PLoS One 2018;13:e0207690.
- Kurtz D, Hyman L, Gwiazda JE, et al. Role of Parental Myopia in the Progression of Myopia and Its Interaction with Treatment in COMET Children. Invest Ophthalmol Vis Sci 2007;48:562-70.
- Saw SM, Nieto FJ, Katz J, et al. Familial Clustering and Myopia Progression in Singapore School Children. Ophthalmic Epidemiol 2001;8:227-36.
- Bullimore MA, Reuter KS, Jones LA, et al. The Study of Progression of Adult Nearsightedness (SPAN): Design and Baseline Characteristics. Optom Vis Sci 2006;83:594-604.
- Dirani M, Shekar SN, Baird PN. Adult-Onset Myopia: The Genes in Myopia (GEM) Twin Study. Invest Ophthalmol Vis Sci 2008;49:3324-7.
- Goss DA, Winkler RL. Progression of Myopia in Youth: Age of Cessation. Am J Optom Physiol Opt 1983;60:651-8.
- COMET Group. Myopia Stabilization and Associated Factors among Participants in the Correction of Myopia Evaluation Trial (Comet). Invest Ophthalmol Vis Sci 2013;54:7871-84.
- Hou W, Norton TT, Hyman L, et al. Axial Elongation in Myopic Children and Its Association with Myopia Progression in the Correction of Myopia Evaluation Trial. Eye Contact Lens
2018;44:248-59. - Leshno A, Farzavandi SK, Gomez-de-Liano R, et al. Practice Patterns to Decrease Myopia Progression Differ among Paediatric Ophthalmologists around the World. Br J
Ophthalmol 2019. - Brennan NA, Toubouti Y, Cheng X, Bullimore MA. Efficacy in Myopia Control. Prog Retin Eye Res 2020; https://doi.org/10.1016/j.preteyeres.2020.100923.
- Hernandez J, Sinnott LT, Brennan NA, et al. Analysis of CLEERE Data to Test the Feasibility of Identifying Future Fast Myopic Progressors. Invest Ophthalmol Vis Sci 2018;59:3388.
- Sindt CW, Riley CM. Practitioner Attitudes on Children and Contact Lenses. Optometry 2011;82:44-5.
- Wolffsohn JS, Calossi A, Cho P, et al. Global Trends in Myopia Management Attitudes and Strategies in Clinical Practice. Cont Lens Anterior Eye 2016;39:106-16.
- Li L, Moody K, Tan DT, et al. Contact Lenses in Pediatrics Study in Singapore. Eye Contact Lens 2009;35:188-95.
- Paquette L, Jones DA, Sears M, et al. Contact Lens Fitting and Training in a Child and Youth Population. Cont Lens Anterior Eye 2015;38:419-23.
- Plowright AJ, Maldonado-Codina C, Howarth GF, et al. Daily Disposable Contact Lenses Versus Spectacles in Teenagers. et al 2015;92:44-52.
- Walline JJ, Jones LA, Rah MJ, et al. Contact Lenses in Pediatrics (CLIP) Study: Chair Time and Ocular Health. Optom Vis Sci 2007;84:896-902.
- Walline JJ, Jones LA, Sinnott L, et al. A Randomized Trial of the Effect of Soft Contact Lenses on Myopia Progression in Children. Invest Ophthalmol Vis Sci 2008;49:4702-6.
- Walline JJ, Walker MK, Mutti DO, et al. Effect of High Add Power, Medium Add Power, or Single-Vision Contact Lenses on Myopia Progression in Children: The BLINK Randomized Clinical Trial. JAMA 2020;324:571-80.
- Kollbaum PS, Jansen ME, Tan J, et al. Vision Performance with a Contact Lens Designed to Slow Myopia Progression. Optom Vis Sci 2013;90:205-14.
- Lam CSY, Tang WC, Tse DY, et al. Defocus Incorporated Multiple Segments (Dims) Spectacle Lenses Slow Myopia Progression: A 2-Year Randomised Clinical Trial. Br J Ophthalmol 2020;104:363-8.
- Berntsen DA, Barr JT, Mitchell GL. The Effect of Overnight Contact Lens Corneal Reshaping on Higher-Order Aberrations and Best-Corrected Visual Acuity. Optom Vis Sci 2005;82:490-7.
- Sulley A, Young G, Hunt C, et al. Wearer Experience and Subjective Responses with Dual Focus Compared to Spherical, Single Vision Soft Contact Lenses in Children During a 3-Year Clinical Trial. Optom Vis Sci 2019;96: E-abstract 195252.
- Walline JJ, Robboy MW, Hilmantel G, et al. Food and Drug Administration, American Academy of Ophthalmology, American Academy of Optometry, American Association for Pediatric Ophthalmology and Strabismus, American Optometric Association, American Society of Cataract and Refractive Surgery, and Contact Lens Association of Ophthalmologists Co-Sponsored Workshop: Controlling the Progression of Myopia: Contact Lenses and Future Medical Devices. Eye Contact Lens 2018;44:205-11.
- Wildsoet CF, Chia A, Cho P, et al. IMI - Interventions Myopia Institute: Interventions for Controlling Myopia Onset and Progression Report. Invest Ophthalmol Vis Sci 2019;60:M106-M31.
- Sheng H, Bottjer CA, Bullimore MA. Ocular Component Measurement Using
eiss Iolmaster. Optom Vis Sci 2004;81:27-34.
