Typical vision-related or asthenopic complaints, such as headaches, tired and burning eyes or blurred vision can be expected in more than 50% of patients even in the younger age group between 18 and 38 years.1 Where this is found to be due to fixation disparity (FD), prescribing prisms may help relieve the symptoms. A new method has been developed which allows an aligning prism to be determined based on the direct measurement of FD.
There are many things which interfere with good binocular vision in today’s digital environment, such as the increased amount of work carried out at short distances and the need to constantly switch between multiple digital devices. These challenges spurred us on to look for a new method for assessing FD.
The result was EyeGenius, a new method for measuring and correcting FD based on direct conversion of the measured FD value (in minutes of arc) into a prescribed prism value (in prism dioptres or Δ). This new interactive measurement technique minimises error from the influence of the person carrying out the examination. EyeGenius was developed by Hoya in co-operation with the University of Applied Sciences and Arts Northwestern Switzerland throughout six years of clinical research, development and testing.
Fundamentals of heterophoria and FD
Binocular deviations were studied by scientists as long as 120 years ago. Maddox examined how the vergence system reacted to prisms2 while Duane introduced a classification system for convergence insufficiency and convergence excess which has been used ever since.3 These approaches have been and continue to be used to measure dissociated heterophorias, which are defined as deviations from the straight-ahead binocular (orthovergence) position without fusion.
The term ‘fixation disparity’ (FD) was introduced by Ogle in 1949. In the years since then, dissociated and associated phorias have increasingly been differentiated. FD assessment and its clinical relevance has attracted a lot of interest from practitioners. FD is defined as a residual misalignment of the foveas within Panum’s Area that persists after the vergence system compensates for neuromuscular bias when fusion is allowed.4 Therefore, FD assessment gives a realistic view of the binocular vision under normal viewing conditions.5
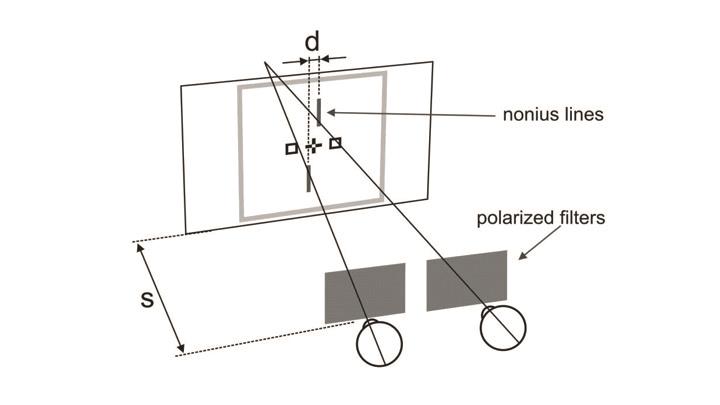
Figure 1: Test to measure FD. The nonius lines are adjustable and the observer has to align them to the central cross. However, on the monitor they are moved around distance (d). The observation distance is marked by (s). The extent of the displacement and the test distance then allow subjective FD to be calculated in minutes of arc
FD is better correlated to asthenopia than dissociated heterophoria4 and represents a good indicator of the visual system’s stress. FD is measured in minutes of arc, and the aligning prism in prism dioptres (Δ). FD is counteracted by aligning prisms so that the latter nullify it. Two parameters are required to measure subjective FD (figure 1):
1 The perceived displacement (d) of both nonius lines.
2 The distance between the test plane and the eye of the tested person(s).
The formula used to determine FD in minutes of arc is
tan α = d/s.
Binocular correction methods using FD test figures were developed by HJ Haase6 and RFJ Mallett7 more than 50 years ago, and they remain in use throughout Europe today. Forty years ago in the USA, Sheedy developed test figures based on Ogles’ ideas to determine FD curves.8
Both, MCH (after Haase) and Mallett tests, have been widely used to assess FD. Prismatic corrections have been successfully used in German-speaking countries to treat patients with asthenopic complaints9-12. Promising results regarding the improvement of reading speed and visual acuity have also been reported in the UK.13,14
The existing methods described above have advantages as well as limitations. The MCH and Mallett methods use conventional procedures to define aligning prisms through the process of measuring associated phorias.
EyeGenius
The EyeGenius method is based on the direct detection of FD and its precise recalculation into an aligning prism by means of a unique algorithm. This allows values to be defined in increments of 0.01 Δ, which is impossible with existing methods. Additionally, modern, electronic visual testing devices are used, which facilitates patient interaction and minimises the influence of the practitioner on the outcome of the test.
EyeGenius research studies
The advantages and disadvantages of prismatic corrections have been debated among experts. As long as the fusion control circuit is active and works under normal viewing conditions, the wearing of prisms affects the position of rest, the fusional reserves and FD.15 The prism can therefore be adapted to by the wearer over a wide range of values. As soon as the fusion is broken, the eyes slowly return to their original vergence position. If the vergence system has a high adaptation ability under normal fusion conditions, small prisms can become ineffective after a long period of wear (this phenomenon is variously known as the ‘eating up’ of prisms or ‘prism adaptation’).
The development of EyeGenius started with a study of the effects of wearing prismatic correction using a high-resolution eye tracking device. This research phase was led by Dr W Jaschinski from the IfADo Leibniz Research Centre for Working Environment and Human Factors in Dortmund, Germany, and the research group Individual Visual Performance, who had experience with research on FD. Significant effects on subjective and objective FD after several weeks of continuous prism wearing could be demonstrated for the first time.16 Even small prism values were effective and the outcomes of this study gave evidence that the vergence system does not fully adapt to prisms.
Another important research area was on the correlation between fixation disparity and aligning prism. A preliminary study measuring FD in minutes of arc was carried out on 40 subjects. Prisms were gradually introduced to neutralise any FD. The amount of prism was increased until FD reached zero or changes its direction. All measurements were carried out with a far and a near vision testing device, and both vertical and horizontal FD were measured. This made it possible to calculate an aligning prism from FD with an accuracy of 0.01 Δ. A high correlation was found between the initial FD and the calculated final aligning prism (r=0.79 horizontally and r=0.89 vertically). The researchers were able to determine conversion factors which made it possible to immediately convert the FD value into an aligning prism. This is the main innovation and foundation of the new EyeGenius method, which allows both rapid and accurate measurements.
The EyeGenius system
EyeGenius is made up of an iPad running the remote control Hoya App, a Far Vision Device and a Near Vision Device. These three interconnected devices use Wi-Fi to communicate with each other (figure 2).

Figure 2: Hoya EyeGenius System
The Far Vision Device (FVD) uses polarisation technology on a 24-inch LCD screen. It is capable of running a wide range of polarised tests without requiring the addition of a supplementary polarised screen to the basic monitor. The tests are carried out with the appropriate polarised glasses. The system provides high-quality polarisation on an even background which eliminates ghost images and makes use of the entire surface of LCD screen.
The Near Vision Device (NVD) is 3D and 10.1 inches in size and is used for near vision examination. Again, it provides high-quality and makes use of the entire surface of LCD screen (3D technology) without the use of polarised filters. The so-called ‘barrier technology’ uses two displays, one in front of the other.
The NVD combines two functions:
1 It is a visual testing device, which displays the test figures necessary for near refraction in 2D and 3D.
2 It can be used by the customer as an interactive tablet computer.
The Remote Control Device is an iPad application named Hoya EyeGenius available from the Apple Store. The Far Vision Device and the Near Vision Device are controlled directly through the Hoya EyeGenius software control panel, running on an iPad.

Figure 3: EyeGenius FD examination
Each step in the test is accompanied by instructions for the examiner, including a script for what to say to the patient.
The EyeGenius concept integrates the most important criteria for measurements, making them reliable, easy and fast.
Pre-tests recognise abnormal binocular vision cases which cannot be assessed by EyeGenius.
In case of unreliable measurement, the system generates a message referring the patient for an extended binocular examination. These might include:
- Unreliable FD measurements, either horizontal or vertical, far or near.
- Difference between far and near FD measurements.
- Detected FD outside of defined ranges.
The near tablet serves as a remote control and is used by the patient to align the nonius lines without influence from the examiner. The FD measurement takes less than 10 minutes for both far and near distance measurements.
The measurement is carried out without trial prisms. Examiners receive the resulting prisms on their remote control right away. The prisms are prescribed after the subjective trial and acceptance by patient.
Available tests
There are more than 60 optometric tests in the EyeGenius system for far and near vision examination divided into four groups:
- The refraction group – contains a variety of different optotypes and tests for astigmatism or binocular balance. There are many different functions, such as choice of a single optotype or rows of optotypes, changes of contrast, red-and-green background or switch to inverse presentation. Users can also choose among a range of randomly generated optotypes.
- The visual function tests contain other functions, like contrast measurements, twilight or glare tests, night myopia tests, fixation figures, and so on.
- The binocular vision tests include the new Mallett test and the whole MCH sequence in line with the directives of the International Association for Binocular Vision (IVBS). The binocular vision tests are available on both far and near vision devices.
- Hoya EyeGenius FD procedure.
EyeGenius method for measuring FD
EyeGenius pre-tests
The goal of the pre-tests is to include patients with asthenopic complaints and exclude all cases with abnormal binocular vision. The EyeGenius pre-tests consist of the asthenopic symptoms questionnaire, a test for checking monocular visual acuity under binocular conditions, and the random dot stereo vision test at near distance.
Patients wear a trial frame during all pre-tests, with far correction for non-presbyopes and near correction for presbyopes. Once all pre-tests have been administered, the examiner is taken directly to the EyeGenius FD measurement.
EyeGenius test figures
The test figures (figure 4) have the following properties:
- A strong central fusional lock (cross and squares), seen by both eyes, to stimulate central fusion;
- A strong peripheral fusional lock (letters), seen by both eyes, to stimulate peripheral fusion
- Presented on the left and on the right in order to create natural binocular viewing conditions and for measurements to be taken under dynamic conditions.
The EyeGenius FD measurements must be carried out without any prism, even if the patient has been wearing prismatic prescription. The method is not designed to allow a summation of prism values.

Figure 4: FD measurement order. 1 and 2: horizontally and vertically at far point. 3 and 4: horizontally and vertically at near point
A sophisticated algorithm using the standard deviation of the test results runs in the background. It analyses far and near FD measurements to ensure they have been taken in a reliable manner. When the far and near measurements are comparable, it calculates the prismatic prescription. When the results are not reliable, the algorithm advises of this and recommends more extensive and specific binocular assessments.
EyeGenius considers prismatic values below 5.0 Δ horizontally and below 3.0 Δ vertically. Values greater than these are excluded, with the advice to carry out a more specific vision examination.
Results of the EyeGenius method
There are three possible outcomes to the EyeGenius sequence:
1 All the measurements are found to be within the defined tolerance values. In this case, an aligning prism prescription is produced, and the examiner demonstrates the effect of the prescription on visual acuity and subjective comfort. The prism is prescribed in addition to the refraction values.
2 The measured values are smaller than 1.0 Δ horizontally and/or 0.5 Δ vertically. The prismatic prescription value is set to zero. If a zero prism is advised, refraction values will be prescribed.
3 One of the following occurs:
- There is a large difference between FD far and near.
- There are large absolute values outside of the range: aligning vertical prism is greater than 3 Δ, and/or aligning horizontal prism greater than 5 Δ).
- The measurements and results are unreliable.
In these cases, there is need for a more extensive binocular examination. EyeGenius will recommend referral to a specialist, as it is likely that special care is required (eg vision therapy, different prisms for near/far or higher prism values).
Conclusion
Prismatic corrections are not the only method in the optician’s toolbox, but they are an important addition to other instruments linked to issues such as refraction, accommodation and other visual functions. It can play an important role in helping patients achieve better vision and visual comfort.
Asthenopic complaints are astonishingly common: a study among opticians in Spain showed that, out of 1,679 patients examined, 56.2% suffered from asthenopia.1 Given the number of people who predominantly work with computers, the total proportion of people with visual discomfort is estimated in the literature to be between 64% and 90%.17 Many of these people are not aware that their issues can be traced back to their eyes, however.18 Asthenopia may thus not be considered as a serious problem by eye care professionals, despite the expected high potential in this field.
We hope that the efficiency and simplicity of the EyeGenius method will increase interest in the field of binocular vision, and will be successfully implemented and used on a daily basis in optometric practices and optical stores. However, it is important to remember that successful binocular correction requires that subjective refraction is taken care of first.
Volkhard Schroth and Professor Roger Crelier are based at the University of Applied Sciences and Arts, Olten, Switzerland, Olga Prenat is education and faculty director EMEA Hoya Vision Care Europe and Dr Natalia Vlasak is based at Maribor University, Maribor, Slovenia.
References
1 R Montés-Micó, ‘Prevalence of general dysfunctions in binocular vision,’ Annals of ophthalmology, vol. 33, no. 3, pp. 205-208, 2001.
2 E Maddox, The Clinical use of Prisms; and the Decentering of Lenses, 2nd Edition ed. Bristol, England: John Wright & Sons, 1893.
3 A Duane, A new classification of the motor anomalies of the eye: based upon physiological principles, together with their symptoms, diagnosis, and treatment. New York: Vail, JH, 1896.
4 R London and RS Crelier, ‘Fixation disparity analysis: sensory and motor approaches,’ Optometry, vol. 77, no. 12, pp. 590-608, Dec 2006.
5 TC Jenkins, LD Pickwell and AA Yekta, ‘Criteria for decompensation in binocular vision,’ Ophthalmic Physiol Opt, vol. 9, no. 2, pp. 121-5, Apr 1989.
6 HJ Haase, ‘Binocular testing and distance correction with the Berlin Polatest (Transl W. Baldwin),’ Journal of the American Optometric Association; 34, 115-124, 1962.
7 RFJ Mallett, ‘The investigation of heterophoria at near and a new fixation disparity technique,’ The Optician, vol. 148 (3844/ 3845), pp. 547-551; 574-581, 1964.
8 JE Sheedy and JJ Saladin, ‘Association of symptoms with measures of oculomotor deficiencies,’ Am J Optom Physiol Opt, vol. 55, no. 10, pp. 670-6, Oct 1978.
9 K Günthert. (1980) Heterophorien im Spiegel der Statistik. Der Augenoptiker.
10 S Schmitz. (1998) Kundenbefragung zur Mess- und Korrektionsmethodik nach HJ Haase (MKH). Deutsche Optikerzeitung DOZ.
11 V Schroth. (1998) Erfolgsbeobachtung: Prismenkorrektion bei Kindern, die nicht freiwillig lesen. Neues Optikerjournal, NOJ.
12 D Methling and W Jaschinski, ‘Contrast sensitivity after wearing prisms to correct for heterophoria,’ Ophthalmic Physiol Opt, vol. 16, no. 3, pp. 211-5, May 1996.
13 CI O’Leary and BJ Evans, ‘Double-masked randomised placebo-controlled trial of the effect of prismatic corrections on rate of reading and the relationship with symptoms,’ Ophthalmic Physiol Opt, vol. 26, no. 6, pp. 555-65, Nov 2006.
14 TC Jenkins, F Abd-Manan, S Pardhan, and RN Murgatroyd, ‘Effect of fixation disparity on distance binocular visual acuity,’ Ophthalmic Physiol Opt, vol. 14, no. 2, pp. 129-31, Apr 1994.
15 J Cooper, ‘Clinical implications of vergence adaptation,’ Optom Vis Sci, vol. 69, no. 4, pp. 300-7, Apr 1992.
16 V Schroth, R Joos, and W Jaschinski, ‘Effects of Prism Eyeglasses on Objective and Subjective Fixation Disparity,’ PLoS One, vol. 10, no. 10, p. e0138871, 2015.
17 M Rosenfield, ‘Computer vision syndrome: a review of ocular causes and potential treatments,’ Ophthalmic and Physiological Optics, vol. 31, no. 5, pp. 502-515, 2011.
18 Z Yan, L Hu, H Chen and F Lu, ‘Computer Vision Syndrome: A widely spreading but largely unknown epidemic among computer users,’ Computers in Human Behaviour, vol. 24, pp. 2026-2042, 2007.
