The use of high energy pulse application to the skin has been used in dermatology for some years. More recently, application has been found in optometry, in particular the management of meibomian gland disease (MGD) that contributes to dry eye (see Optician 17.03.2017).
The persistent nature of the condition and the need for good compliance with the currently accepted treatment options makes MGD a stubborn condition to address. Any treatment that might be applied by a practitioner and offer a longer-term solution should be viewed with interest. Intense pulsed light (IPL) therapy has been used for some years in the cosmetics industry for removal of skin lesions such as telangiectasia, port-wine stains and haemangiomas.
The technique has also been used in the management of severe facial erythema in patients with acne rosacea. In these patients, it was noticed that there also appeared to be some improvement in their MGD and it is from this serendipitous finding that an IPL treatment tailored for MGD was developed.
Background
IPL has been used for many years in dermatology,1-4 and was FDA approved in the US for the treatment of telangiectasia in 1995.4 These are the abnormal blood vessels found in, for example, rosacea which leak inflammatory mediators that can lead to skin damage. IPL has also found use in the more general treatment for acne as it is also believed to eradicate causative bacteria.1,2
More recently, IPL treatment has been cited in the TFOS DEWSII recommended staged management plan for dry eye disease, and is considered a second stage management option (table 1).8
--------------------------------------------------------------------------------------------
Table 1: TFOS DEWSII recommended staged management and treatment of dry eye disease.10,11
The steps outlined below show the most evidence-based staged management of DED depending on severity. The exact nature of an individual’s DED will dictate the range and number of management options selected from one or more steps. Options within a category are not ranked according to importance and may be equally valid.
Step 1:
- Education regarding the condition, its management, treatment and prognosis
- Modification of local environment
- Education regarding potential dietary modifications (including oral essential fatty acid supplementation)
- Identification and potential modification/elimination of offending systemic and topical medications
- Ocular lubricants of various types (if MGD is present, then consider lipid containing supplements)
- Lid hygiene and warm compresses of various type
Step 2: If above options are inadequate consider:
- Non-preserved ocular lubricants to minimize preservative-induced toxicity
- Tea tree oil treatment for Demodex
- Tear conservation
- Punctal occlusion
- Moisture chamber spectacles/goggles
- Overnight treatments (such as ointment or moisture chamber devices)
- In-office, physical heating and expression of the meibomian glands (including device-assisted therapies)
- In-office intense pulsed light therapy for MGD
- Prescription drugs to manage DED
- Topical antibiotic or antibiotic/steroid combination applied to the lid margins for anterior blepharitis (if present)
- Topical corticosteroid (limited-duration)
- Topical secretagogues
- Topical non-glucocorticoid immunomodulatory drugs (such as cyclosporine)
- Topical LFA-1 antagonist drugs (such as lifitegrast)
- Oral macrolide or tetracycline antibiotics
Step 3: If above options are inadequate consider:
- Oral secretagogues
- Autologous/allogeneic serum eye drops
- Therapeutic contact lens options
- Soft bandage lenses
- Rigid scleral lenses
Step 4: If above options are inadequate consider:
- Topical corticosteroid for longer duration
- Amniotic membrane grafts
- Surgical punctal occlusion
- Other surgical approaches (eg tarsorrhaphy, salivary gland transplantation)
--------------------------------------------------------------------------------------------
Devices launched in the UK for eye care practitioners are becoming increasingly accessible and affordable. The two main players in the UK are the Eye-Light system (Topcon, see figure 1) and the E-Eye IRPL (Grafton Optical, figure 2).

Figure 2: The E-Eye IRPL unit from Grafton Optical
How does IPL work?
A Xenon flash lamp will emit wavelengths from between 400 and 1200nm.1,3,4 When this light passes through a filter cut-off at around 500nm, it causes the blood within telangiectatic blood vessels exposed to the incident light to coagulate, so causing them to close.1,2,4 Toyos et al noted that acne rosacea patients treated with IPL reported a decrease in their dry eye symptoms (80% of people with facial skin rosacea have MGD).1,2
The exact nature of the mechanism is not fully understood. Simply put, it is believed that IPL leads to:
- A decrease in the number of inflammatory markers found at the lid margin
- Improved nerve function around the meibomian glands
- Flash heating of the meibum, so increasing expressibility2 (see figure 3)
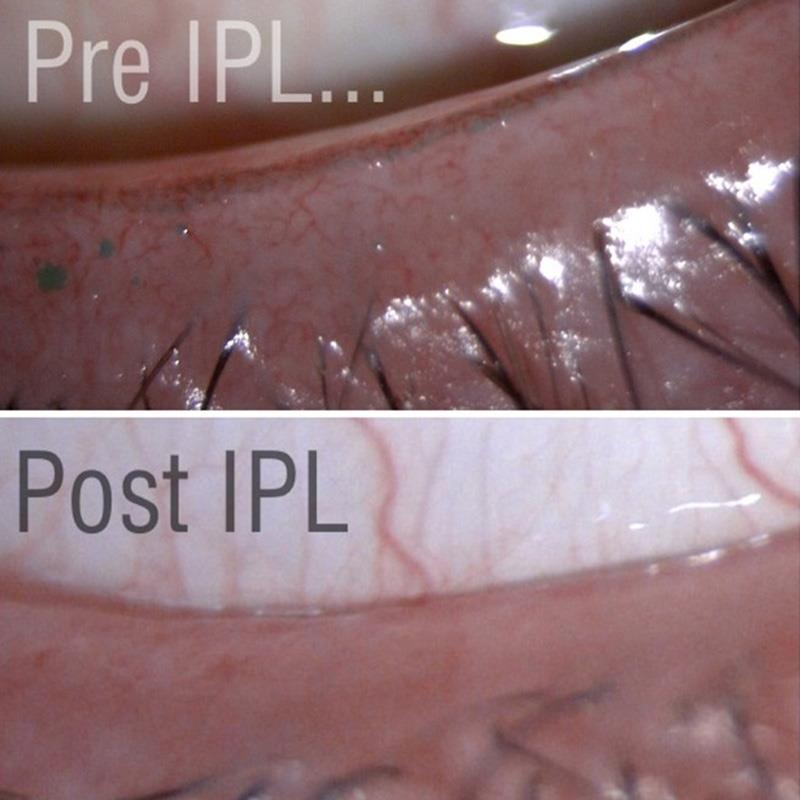
Figure 3: Lid margins before and after IPL treatment
It has been speculated that the flash of both visible and infra-red light leads to intracellular changes within the DNA which alter protein levels (a process described as photobiomodulation). Dell excellently summarised the mechanisms in his review paper,2 and they are thought to include:
- An increase in mitochondrial function2,5
- Increased calcium channel flow2,5
- Increased collagen synthesis2
- Modulation of the secretion of anti-inflammatory molecules2
- Suppression of matrix metalloproteinases (or MMPs) which are proteolytic enzymes that degrade the extracellular matrix and so influence cellular migration2
- Demodex necrosis and death (a chromophore in the exoskeleton of the mite absorbs IPL energy)2
The overall effect of these actions is to help restore the homeostasis of the tear film.
In practice
In my practice (TK&S), we have been using the Eye-Light system (distributed by Topcon in the UK) since the beginning of the 2018. It is a two-step system, with an IPL step followed by use of the Low Level Light Therapy mask (figure 1) for the phase that induces photobiomodulation.
Manufacturer recommendations are to give the patient three treatments, separated by seven to 14 days, followed by a ‘top up’ treatment to be implemented annually.
Table 2: Results
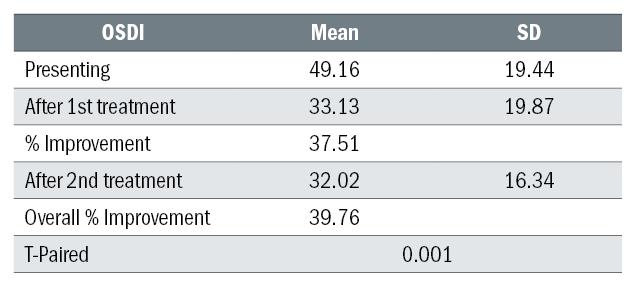
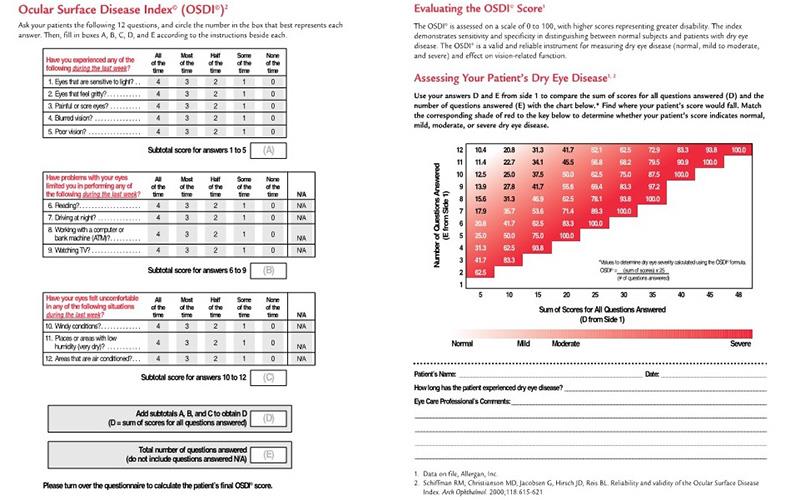
Figure 4: OSDI questionnaires
As the results show, with our patient base, IPL can lead to an improvement in OSDI score, in some cases it can be life changing.
There have been three key lessons that our experience has taught us:
1 IPL is not the ‘magic pill’ as exemplified by the following patient. Our first patient, a 65 WF, had a history of dry eye secondary to refractive surgery. EF had used heat MGD eye masks, artificial tears, had tried the LipiFlow system and we had just put her onto Ikervis (topical ciclosporin) and her OSDI at this stage was still 41.66. After her first IPL treatment,
EF returned with a score of 12.5. We were amazed. So, we asked EF to stop all additional treatment and return for her second treatment. At this visit, EF reported a significant decrease in comfort (OSDI of 70). We restarted all treatments and, before her third treatment, her OSDI was down to 50. Three months later, EF had an OSDI of 15 which had become 25 by the time of her last visit (six months post last IPL treatment). IPL can help further improve patient comfort, but in our experience, the patient will still need to continue with stage one elements of dry eye management. At TK&S, we make sure that the patient is appropriately educated about the importance of continued management (homework) after treatment.
2 A single treatment will tell you if it is going to work:
- Four patients out of 18, had no improvement in OSDI score. Unfortunately, these patients reported no improvement at all (confirmed by OSDI), after 1st, 2nd or 3rd treatments.
- The biggest reported improvement appears to happen after the 1st treatment, and if that stage there is not significant change, from our data it does not appear as if the patient will get any further benefit from additional treatments.
3 Use a questionnaire:
- Patient 19, an 80-year-old female, was recommended IPL treatment before having cataract extraction. The presenting OSDI was 18.15, and after treatment she recorded a score of 8. When questioned, she told us she felt that it had made no difference at all.
- Independent questionnaires are a good way to record results, and also to show patients the improvement (if any has been achieved).
Conclusion
Optometry is ideally placed to offer IPL treatments for dry eye disease sufferers. The techniques involved in treatment are easily delegated to support staff (with appropriate training and support), and the units do not take up much space.
IPL treatment for patients who have been properly managed and educated can be life-changing, and will encourage patient loyalty and new referrals.
Dr Keyur Patel is a therapeutic optometrist working in Northampton.
Disclosures – The author has no financial interest in Topcon.
Acknowledgment
I would like to thank Andrew Yorke, Fergal Byron and Richard Balls at Topcon for allowing TK&S Optometrists early access to the Eye-Light technology, training and on-going support.
References
1 Toyos R, McGill W, Briscoe D. Intense pulsed light treatment for dry eye disease due to meibomian gland dysfunction; a 3-year retrospective study. Photomed Laser Surg 2015;33:41–6. doi:10.1089/pho.2014.3819
2 Dell SJ. Intense pulsed light for evaporative dry eye disease. Clin Ophthalmol 2017;11:1167–73. doi:10.2147/OPTH.S139894
3 Rennick S, Adcock L. Intense Pulsed Light Therapy for Meibomian Gland Dysfunction: A Review of Clinical Effectiveness and Guidelines. Ottawa (ON): : Canadian Agency for Drugs and Technologies in Health 2018. http://www.ncbi.nlm.nih.gov/books/NBK531789/ (accessed 20 Nov 2018)
4 Arita R, Fukuoka S, Morishige N. Therapeutic efficacy of intense pulsed light in patients with refractory meibomian gland dysfunction. Ocul Surf Published Online First: 13 November 2018. doi:10.1016/j.jtos.2018.11.004
5 Low-level laser therapy. Wikipedia. 2018.https://en.wikipedia.org/w/index.php?title=Low-lev... (accessed 20 Nov 2018).
6 de Freitas LF, Hamblin MR. Proposed Mechanisms of Photobiomodulation or Low-Level Light Therapy. IEEE J Sel Top Quantum Electron 2016;22. doi:10.1109/JSTQE.2016.2561201
7 Intense pulsed light. Wikipedia. 2018.https://en.wikipedia.org/w/index.php?title=Intense... (accessed 20 Nov 2018).
8 Vora GK, Gupta PK. Intense pulsed light therapy for the treatment of evaporative dry eye disease. Current Opinion in Ophthalmology 2015;26:314–8. doi:10.1097/ICU.0000000000000166
9 Nelson JD, Craig JP, Jones L, et al. What is it, why does it occur and how can it be diagnosed and treated?;:4. Nelson et al. — What is it, why does it occur and how can it be di.pdf. https://www.tearfilm.org/ckfinder/userfiles/files/... (accessed 23 Nov 2018).
10 Jones L, Downie L, Korb D, et al. TFOS DEWS II management and therapy report. The Ocular Surface Published Online First: 1 July 2017. doi:10.1016/j.jtos.2017.05.006
11 Farrant S. TFOS DEWS II – part 3; Management. Optician, 17.03.17.
