For the last in my series of articles, I thought it might be of interest to discuss a case involving anterior eye management, rather than my more typical focus upon posterior pathology. I decided to take a subject close to my heart; myopia and its progression. I am a -13.00DS myope married to a -8.00 myope who has a young son currently plano.
Myopia therapy
I have been following the debate on myopia and myopia management closely over the years and felt that the time was now right to dip my toe in the water. The prevalence of myopia is increasing with some studies expecting that about 50% of the global population will be myopic, currently some 1.9 billion people are already myopic.1
There are numerous studies which show the risk of AMD, cataract and glaucoma, alongside the more widely known association with retinal detachment, is significantly higher in myopia.
Currently, the research points to the need for more time spent outside and consideration of the implications of prolonged screen use and near work. This is all well and good but not very practical for your average child, especially a teenager. This leaves us with the more clinically applicable option, such as the use of a centre distance multifocal contact lens like the CooperVision Biofinity multifocal lens.
The annulus for reading creates a hyperopic defocus which has been shown in some studies to reduce the rate of progression of myopia. This approach is ‘off licence’ and does not seem to offer the most dramatic of benefits. As yet, the CooperVision MiSight lens for myopia control has not been released to the wider profession and so is not currently an option for me. Readers might be interested in seeing the extent of impact of a multifocal contact lens as compared with other interventions by using the Brien Holden Vision Institute Myopia Calculator (at https://calculator.brienholdenvision.org).
Another option is the use of low dose atropine (see Optician 05.10.18). Again, in my practice this is not practical as the drug is not currently commercially available in the UK and has not been licenced for this purpose to date.
This leaves orthokeratology, by no means a new approach. This subject has been covered in previous articles within Optician and has the benefit of a robust and comprehensive longitudinal dataset which has shown in numerous studies efficacy at myopia control.2
Orthokeratology was first commercially offered in the 1960s, though its results were not overly predictable. Dr Richard Wlodyga and Nick Stoyan, in particular, are generally credited with developing the first reverse zone lens design in the 1990s. Since then, many contact lens companies have developed their own lenses and systems. Typically, about 6µm of flattening is required to change the prescription by 1 dioptre.
Orthokeratology lenses typically have three distinct zones:
- A flat central zone, which is made as large as possible to reduce haloes that would be induced if the treatment area is smaller than the pupil size. There is a correlation between the degree of myopia and the size of the treatment zone. We fit the central area on alignment.
- The mid zone is the reverse curve, which provides the negative pressure to steepen the mid-peripheral cornea. The curve dynamics are calculated to ensure there is no change in overall sag of the lens.
- The outer zone is the peripheral aspheric zone, which is designed to give an alignment fit to the peripheral cornea. This may be either spherical or toric.
The total diameter of an orthokeratology lens is larger than a standard RGP, and is typically about 5cm smaller than the corneal diameter.3
The process of undertaking a fitting is fairly straightforward when using the No7 EyeDream system. Following refraction, you take baseline topography of the cornea and accurate measurements of corneal diameter. The topography is taken from the Medmont E300 into an Eyedream program which requires you to add all the necessary variables (figure 1). From this, No7 can calculate the required first lens for the treatment.
Typically, the lenses take about one week to be produced and returned to the practice where they may be fitted to the patient. A standard RGP insertion and removal teaching session is undertaken. If fitting correctly, you will see the three zones described above clearly defined with an area of apical alignment, the reverse curve showing extensive pooling of fluorescein and the peripheral alignment curve with a clear amount of edge lift.

Figure 2: Typical three zone fluorescein pattern of an orthokeratology lens
Patient 1
My first case concerns a 14-year-old female who has experienced -1.00DS of myopic progression in less than one year. There were no underlying pathological processes known of and she comes from a family whose members express moderate myopia. In this case, the parents were looking for any way that the degree of myopic progression might be managed while giving their child freedom from glasses and the ability to follow proper compliance – in particular, not swimming in their lenses. The child was a talented and very keen surfer – a sport that has excellent breaks in beautiful West Wales (figure 3).

Figure 3: The incentive for orthokeratology
Patient CH details:
Refraction
- RE -3.25/-0.25x115 (6/5)
- LE -3.00DS(6/5)
Ocular examination
- Unremarkable
Pre-treatment topography (figure 4) based on four scans summated into a single composite eye.
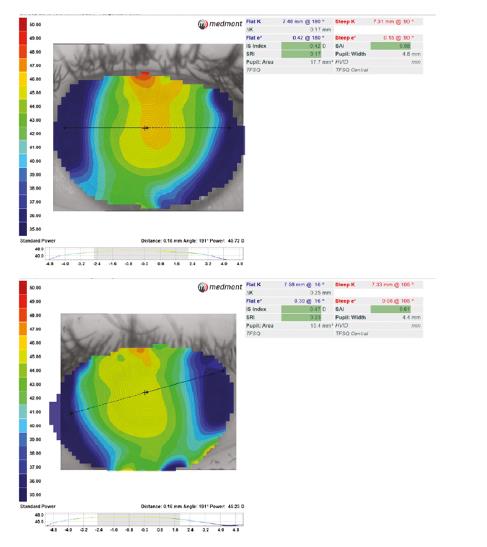
Figure 4: RE initial assessment for the right eye (a) and the left eye (b). Each map is a composite of four scans
The patient quickly overcame the initial discomfort of the lens and was adept at insertion and removal after only a relatively short time. Figure 5 shows one of the lenses on the eye at collection.

Figure 5: Left lens in situ on collection
The protocol was then for the patient to be sent away and for them to be seen first thing in the morning after the first overnight wear. Typically, 60 to 70% of the final optimum correction with the initial lens is achieved after only one overnight wear.
Day 1
The patient arrived at the practice for 8:30am having successfully slept in the lens overnight with no issues or concerns. They had removed the lens and felt the vision much improved, though not perfect.
Vision Over refraction
R (6/10) -1.00 D
L (7/7.5) -0.50 D
The cornea was examined and there was no significant staining nor any evidence of lens binding. I took scans for the record but, as already mentioned, the first night of wear does not usually generate the full potential correction of that lens. The protocol then calls for the patient to be recalled after four to seven nights of overnight wear.
Day 7
The patient returned for their one week follow-up having slept in the lenses nightly for the last week. They reported their vision had improved further and, while they were aware of a little glare in the evening (possibly a sign of regress over the course of the day), the acuity achieved was adequate. More importantly, they had been able to surf safely with no visual correction.
Again, the cornea was checked and found to be normal.
Vision Over Refraction
R (6/7.5) -0.75 D
L (6/6-1) -0.50 D
Almost all of the desired effect had been achieved but, due to the residual myopia, it was likely that by the evening there was more significant myopia present. You would ideally leave a young myope slightly hypermetropic to allow for this over the day.
Day 14
The patient returned for the next scheduled check in the morning after the two weeks of overnight wear. They had noticed a reduction in symptoms of glare, probably as a result of the stabilisation of the treatment plus a degree of adaption. Figure 6 shows the change analyses for the patient.
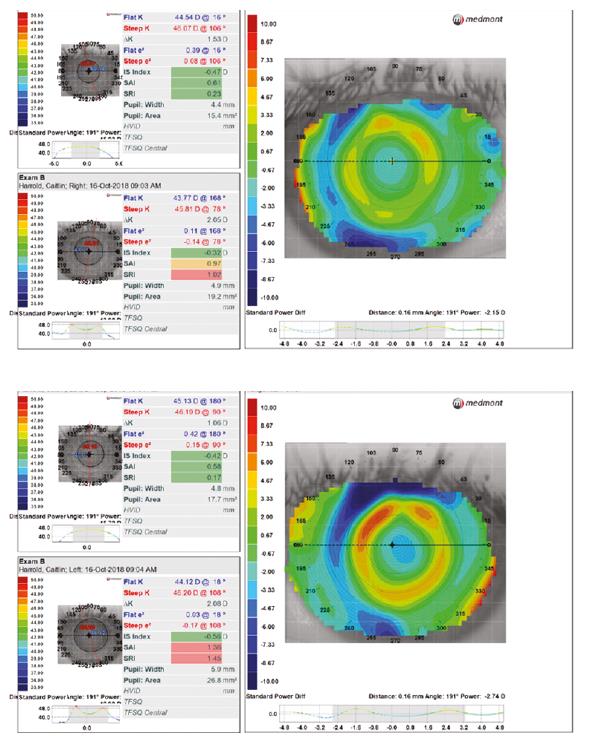
Figure 6: Change analyses showing the change in corneal surface profile for the right eye (a) and the left (b)
Vision Over Refraction
R (6/6-2) -0.50 D
L (6/6) -0.25 D
As can be seen in both these plots, there is now an area of relatively flattened cornea surrounded by an annulus of steeper cornea before the change drops away into the corneal periphery. The mark of success is the doughnut-shaped ring of red on the plot.
Having analysed the most recent plots we have decided that a new lens is required with the goal of correcting the last residual myopia which should reduce the blur and glare, especially that experienced at the end of the day.
Discussion
It is interesting to be presenting a case from the perspective of a novice rather than an expert, and I cannot pretend to have all the answers. I do, however, feel strongly that as practitioners, we need more to be having a discussion with the parents of young myopic children about the risk of progressing to higher orders of correction and, while they are still young enough, to have this progression slowed by a meaningful degree. This will take a degree of maturity from the profession, and I wonder in years to come whether the lack of discussion about myopia management could be seen as a clinical omission in the same vein as the more recent cases where cross-linking in keratoconus was not mentioned.
Not every practitioner will be in a position to offer all solutions and, of course, solutions offered should be backed up by good evidence. There are also cost implications for the patient with up-front fees typically around £150 and monthly fees of approximately £35 thereon, though obviously fees will vary.
The safety profile of the lenses is comparable to that of simple soft contact lens modalities and I have found the drive to discuss them comes from a genuine feeling that you are providing a measurable treatment rather than simply passively correcting a progressing defect.
Andy Britton is an optometrist and co-director of Specsavers Haverfordwest in South Wales.
Useful resources
- A useful resource for practitioners and patients which provides evidence-based estimates of the likely efficacy of interventions can be found at http://www.Brienholdenvision.org.
- The College of Optometrists also published a special edition of Ophthalmic and Physiological Optics in May of 2018 which provided a complete breakdown of the state of the nation in myopia research and management, edited by Dr Nicola Logan.
References
1 Holden B et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology, Volume 123, Issue 5, May 2016, Pages 1036-1042.
2 Huang J et al. Efficacy comparison of 16 interventions for myopia control in children: a network meta-analysis. Ophthalmology. 2016 Apr;123(4):697-708.
3 Crouch L. Introduction to Orthokeratology – lens collection and aftercare. Optician, 15.12.2015.
