Initial presentation
EB, a 32-year-old female Caucasian presented to our practice as an emergency appointment. The patient’s chief complaint was photosensitivity in the right eye which was also uncomfortable.
She reported she had suffered a sudden onset of pain on the lower part of her eye two days ago, and since then the pain had been getting less (slowly). The photosensitivity had presented at the same time as the pain, and had persisted with no improvement since.
Examination results at this first presentation are summarised in table 1.
Initial diagnosis and management
An initial tentative diagnosis was made of traumatic anterior iritis though the possibility of herpes keratitis was considered.
Management was undertaken as follows:
- Cyclopentolate 1% topical drops (tds – three times a day) for right eye to be reviewed after 24 hours (a private prescription was issued).
- Clinitas Hydrate gel (nocte)
- Theoloz Duo (every one to two hours)
One day follow up and management
EB reported a marked improvement in photosensitivity, but had awoken this morning with the eye feeling sore. Examination now showed minimal corneal staining (figure 3), with resolution of anterior chamber reaction (dark and quiet).
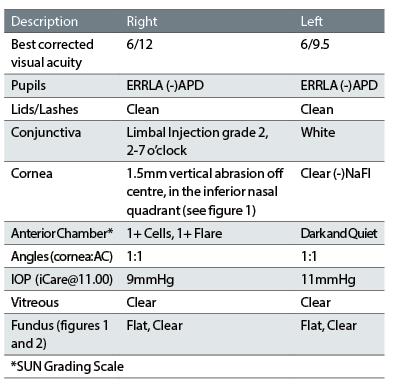
Table 1: Clinical findings at first presentation
A diagnosis of traumatic iritis was now confirmed and the management plan was as follows:
- Continue with cyclopentolate (tds) for another day (Saturday and Sunday) then stop
- Use Clinitas Hydrate Dry Eye (every one to two hours)
- Any worsening of signs to seek advice.
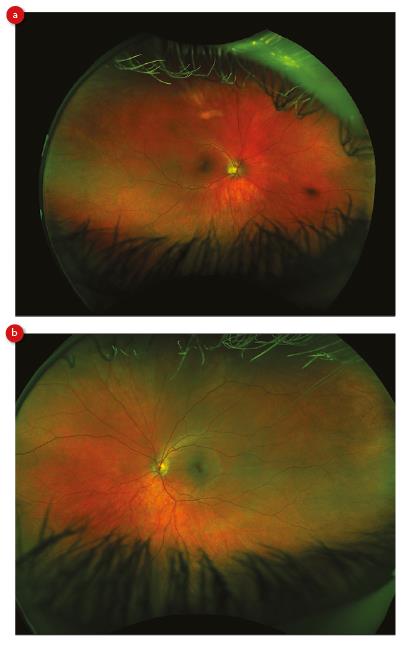
Figure 1: Clinical findings at first presentation
Uveitis is inflammation of the uveal tract and can be sub-divided into the following categories depending on location:
- Anterior – inflammation predominantly affecting the iris (iritis) or the iris and anterior ciliary body or pars plicata (iridocyclitis).
- Intermediate – involves posterior ciliary body (pars plana), anterior choroid.
- Posterior – involves the choroid posterior to the vitreous base and retina. This form is almost always chronic.
- Pan-uveitis – generalised involvement of uveal tract. This form is always chronic.
Anterior uveitis is the most common form (12 per 100,00)1,3-5 and first presents typically in young and middle aged people. Anterior uveitis accounts for anything from 50 to 90% of uveitis cases.3-5
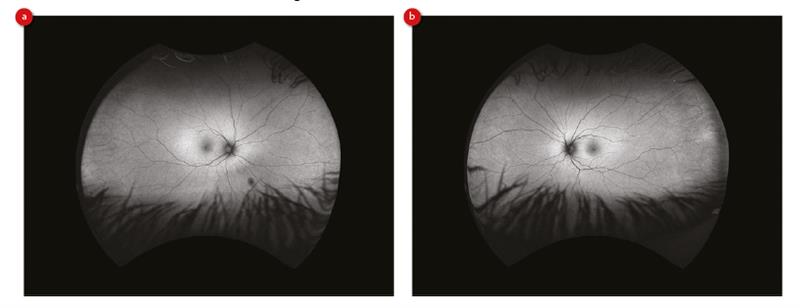
Figure 2: Infra-red wide-field view of retina, (a) right and (b) left
Most cases of iritis are idiopathic, of no identifiable direct cause, with 20% due to trauma.3,5
Traumatic uveitis tends to be more prevalent in younger patients, and more common in males than females.5
Table 2 lists the known signs and symptoms associated with traumatic uveitis.
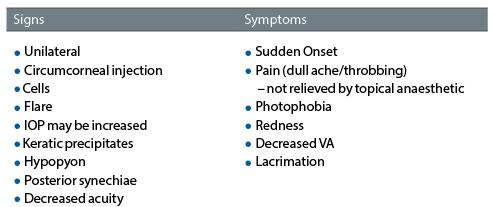
Table 2: Signs and symptoms of traumatic uveitis1,5
Differential diagnosis for acute anterior uveitis would include consideration of the following:
- Acute angle closure glaucoma
- Traumatic hyphaema
- Traumatic corneal abrasion
- Traumatic retinal detachment
- Phacogenic uveitis
- Herpetic uveitis
With epithelial damage in the right eye of EB, it was important for us to rule out any possible herpetic origin.
Treatment for anterior uveitis is usually:
- Cycloplegia – to minimise ciliary sphincter spasm (and therefore reduce pain) and prevent synaechial formation.
- Steroid – varying dosage is used depending on the severity of the inflammation.
With a corneal abrasion, and potential herpetic (or indeed any infective) involvement, a steroid at this stage would suppress the immune system and allow the virus to proliferate. It was therefore decided to start solely with the cycloplegia, and use heavy lubrication and review after 12 hours.
The College of Optometrists Clinical Management Guidelines,1 (and the Moorfields Manual4) recommend the use of cyclopentolate 1% three times per day, having first excluded the possibility of angle closure.
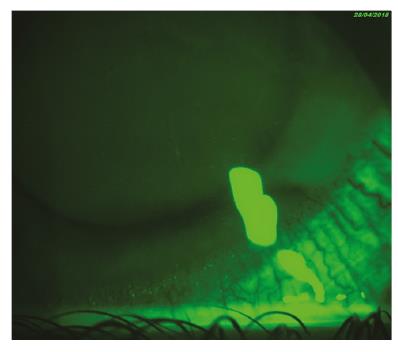
Figure 3: Anterior right eye showing inferior nasal lesion
Aggravation of the ciliary nerves and the subsequent ciliary muscle spasm are believed to lead to eye pain, with the ciliary spasm also irritating the trigeminal nerve causing photophobia.3 There is also increased permeability of blood vessels leading to cells and flare in the anterior chamber.3,5
Cyclopentolate hydrochloride is a cholinergic antagonist (anti-muscarinic) and acts upon the pupil leading to mydriasis and paralysis of the ciliary body (cycloplegia).2 The stabilisation of the ciliary body leads to pain relief and reduces photosensitivity (despite dilation) and also helps to stabilise the blood/aqueous barrier, so reducing the leakage of white blood cells and other inflammatory mediators into the anterior chamber.5 Cyclopentolate is a prescription only medicine (POM) that can be used and supplied by all optometrists, both entry level and independent prescriber (IP) optometrists.6
At follow up review, the corneal abrasion had improved and the anterior chamber had quietened, with no cells or flare apparent. With resolving corneal abrasion and quieting of the anterior chamber, it was felt that a steroid was not necessary but could have been prescribed (by an IP optometrist) or via referral to an ophthalmologist, to further reduce inflammation if necessary.
Conclusion
A simple traumatic iritis, as presented here, is manageable within optometric practice by any optometrist, if they feel comfortable doing so. Assessing the anterior segment, grading any anterior chamber reaction, measuring IOP and undertaking dilated fundus examination are all within core competencies.
The College of Optometrists Guidelines1 grade the first episode as a B2 (Alleviation and palliation: normally no referral to Ophthalmologist), raising to an A3 (Urgent – within one week) if no improvement after one week of pharmacological treatment (see table 3).
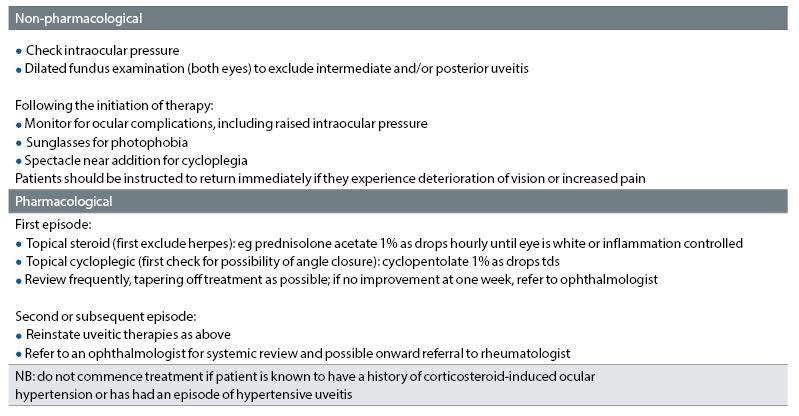
Table 3: College of Optometrists Clinical Management Guidelines for Uveitis
With suitable follow up, EB was treated and managed in practice without the need for a visit (and long wait) to the eye casualty department.
Dr Keyur Patel is a therapeutic optometrist based in Northampton.
References
1 College of Optometrists Clinical Management Guidelines for uveitis (anterior, acute and recurrent). https://www.college-optometrists.org/guidance/clin... (accessed 8 May 2018).
2 Engelhard SB, Patrie J, Prenshaw J, et al. Traumatic uveitis in the mid-Atlantic United States. Clin Ophthalmol 2015;9:1869–74. doi:10.2147/OPTH.S90153
3 Traumatic iritis - EyeWiki. http://eyewiki.aao.org/Traumatic_iritis (accessed 4 May 2018).
4 Jackson TL, editor. Moorfields Manual of Ophthalmology. 2nd ed. JP
5 Kim J, Edens MA. Iritis. In: StatPearls. Treasure Island (FL): : StatPearls Publishing 2018. http://www.ncbi.nlm.nih.gov/books/NBK430909/ (accessed 4 May 2018).
6 College of Optometrists Clinical Management Guidelines - cyclopentolate. https://www.college-optometrists.org/guidance/opto... (accessed 8 May 2018).
7 Bartlett J, Jaanus S. Clinical Ocular Pharmacology. 2nd ed.
