Jonathan Bourton continues our series of case studies from the Institute of Optometry. The patient presented for an examination to see if she met the visual standards to become an ambulance driver
A 27-year-old female Caucasian attended for an eye examination at her GP's request to see if she met the visual standards for a London ambulance driver.
She was asymptomatic but reported a long-standing reduction in vision in her left eye due to coloboma. It was noticed shortly after birth that the left globe appeared smaller than her right globe and at the age of six months the parents had noticed a left divergent heterotropia. Her general health was very good (mild asthmatic) and she did not report any headaches, diplopia or flashing lights.
She had received cosmetic squint surgery to her left eye to correct an exotropia at the age of 15 years and at that time a short trial period of occlusion of the right eye was carried out under the hospital eye service. However, there was no improvement in visual acuities and occlusion of the right eye was stopped.
The patient drove a motorbike and her current occupation was as a driving instructor. Cover test at distance revealed a left 20Æ exotropia (manifest divergent squint) with 5Æ left hypertropia. There was a normal pupil response in the right eye to direct and near. The left pupil showed a relative afferent pupillary defect (RAPD). Right and left motility was full, with no anomaly of the ocular movements. IOPs were within the normal range: Right eye 15mmHg; left eye 14mmHg respectively (non-contact, AO at 10:15am). On slit-lamp examination there was microphthalmos of the left eye. Photopic pupil sizes were asymmetrical with the right pupil measuring 2mm in diameter and the left pupil 1.5mm respectively. Bilateral anterior segments were quiet.
On slit-lamp examination there was microphthalmos of the left eye. Photopic pupil sizes were asymmetrical with the right pupil measuring 2mm in diameter and the left pupil 1.5mm respectively. Bilateral anterior segments were quiet.
With indirect ophthalmoscopy and dilated pupils, the right eye showed a large (three disc diameters in size), sharply circumscribed, glistening white in appearance, and deeply excavated, infero-nasal, chorioretinal defect. Cup to disc ratio was 0.2 and shallow. Myelinated nerve fibres were noted between 4 and 5 o'clock (Figure 1). In the left fundus there 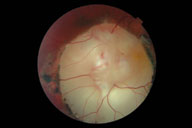 was a very large (six disc diameters in size), sharply circumscribed, very deeply excavated, chorioretinal defect, glistening white in appearance and involving the disc (Figure 2).
was a very large (six disc diameters in size), sharply circumscribed, very deeply excavated, chorioretinal defect, glistening white in appearance and involving the disc (Figure 2).
The patient had a small Rx in the right eye (0.00/-0.50 x 90 VA 6/5) and hypermetropic in the left eye (+1.50DS VA 6/120- central viewing, VA 6/96 with eccentric viewing).
A diagnosis of microphthalmos (left eye) and bilateral coloboma was made. The coloboma did not extend to any other ocular structures.
A central 30-2 threshold visual field test (HFA II) showed a superior visual field defect in both quadrants in the left eye and a superior visual field defect in the right quadrant of the right eye.
With respect to her occupational application, an Esterman visual field test (HFA II) was also carried out and a single point was missed in the superior right quadrant (within 20¡ from fixation). It was discussed with the patient that she had failed to pass the driving standards specified by the Ambulance Service. The visual standards for the Ambulance Service are that all applicants must meet the minimum standards laid down by the Department of Transport and EC for Group II drivers which are:
A visual acuity, with corrective lenses if necessary, of at least 6/9 in the better eye and at least 6/12 in the worst eye
If corrective lenses are used, the uncorrected acuity in both eyes must be 3/601
No visual field defect.
The Royal College of Ophthalmologists in its advice to the DVLA has defined that the minimum visual field for safe driving is a field of vision of at least 120
