In the first of a two-part discussion concerning what influences measurements with the Mallett unit, Rajula Karania and Bruce Evans look at the theory behind fixation disparity and its measurement
The Mallett fixation disparity test is a widely used diagnostic tool within UK optometry. The purpose of this study was to evaluate for the first time the effect of test instructions on the results of this test in a clinical setting. Previous research indicates that the Mallett unit is a useful tool for detecting symptomatic heterophoria at near, having both good sensitivity and specificity. However, the significance of precise instruction technique has received little attention.
Our research was conducted as a two-part study. In part one, we surveyed and observed the current method of use of the Mallett fixation disparity test by practitioners and then, in part two, we compared results obtained with this 'standard' method of questioning with the more 'specific' method of questioning that has recently been suggested in the literature.1
The results demonstrate that the testing method is important: patients need to be asked not just whether the Nonius strips are aligned but also whether one or both of the strips ever move. In this respect, the authors feel that perhaps further research is indicated to investigate the significance of precise test instructions in other subjective optometric and orthoptic tests. In these two articles we will describe our findings and their implications.
An introduction to fixation disparity
Fixation disparity is a minute ocular misalignment under conditions of binocular single vision and, in the UK, is usually detected using the Mallett fixation disparity unit. This instrument creates natural viewing conditions, whereby the patient's binocular system is fused using both central and peripheral fusion locks. This allows the examiner to determine the minimum prism power that eliminates the fixation disparity: the associated phoria or aligning prism. The spherical power that eliminates the fixation disparity, the aligning sphere, can also be determined.
During normal binocular vision the object of regard stimulates retinal elements in each eye, which give rise to the same subjective visual direction so that the person perceives one image of the object. These elements have conventionally been described as corresponding retinal points or elements.2 The term 'corresponding retinal points' is really a misnomer since this is a point to area correspondence. Panum, in 1858, described these areas as Panum's fusional areas. They are elliptical with their long axes horizontal and increase in size in the periphery.3
Panum's fusional space is the spatial counterpart of Panum's fusional area and is contained within two curved surfaces, one on each side of the horopter surface.4 All objects lying within this three-dimensional space will fall in Panum's areas and will therefore be seen singly. Panum's area allows for some imprecision in eye movements without the person experiencing diplopia.5 Objects lying outside Panum's fusional space may appear in physiological diplopia.
Fixation disparity occurs when the images of a binocularly fixated object do not stimulate corresponding retinal points but still fall within Panum's fusional areas, the object thus being seen singly.6 Fixation disparity allows fusion and binocular single vision without precise bifoveal fixation.7
The angular extent of fixation disparity is a measure of the degree to which the images have slipped.8 The conventional view is that fixation disparity typically measures between 5-10 minutes of arc and rarely exceeds 10 minutes of arc.9 The cone density is greatest at the fovea and therefore here there is little room for error of fixation. Consequently, Panum's areas at the fovea are likely to be small10 and early estimates11,12,13 have shown them to be between 6-15 minutes of arc.10
Away from the macula, beyond a visual angle of 5º, Panum's areas measure approximately 6 per cent to 7 per cent of the angle of eccentricity.14 This is in direct relation to the decreasing cone density in more peripheral regions of the retina. This in turn makes the peripheral visual field more tolerant of larger degrees of disparity and less likely to undergo adaptations like suppression to avoid diplopia.15 Although the variation in size of Panum's area is described in terms of retinal eccentricities, they are in reality a cortical phenomenon.16 Ogle et al17 suggested that the magnitude of fixation disparity depends on the strength of innervations to the extra ocular muscles during fusion. This in turn is related to the magnitude of heterophoria, the strength of compensating fusional vergence, and the complexity of detail of the visual target. Fixation disparity plays an important role as a feedback stimulus to maintain a particular level of vergence innervation.18,19 The finding that the apparent dimensions of Panum's areas vary with different testing conditions and target parameters may help to explain studies indicating that Panum's areas may be much larger than the conventional view.20,21,22,23
The stress theory of fixation disparity and the importance of the fusion lock
Mallett interpreted fixation disparity as a sign of stress when the fusional reflexes are incapable of maintaining perfect superimposition of normally corresponding receptive fields24,25 and there is considerable evidence to support this view.
Joshua and Bishop26 found that the binocular response from optimally superimposed receptive fields is greater by about 45 per cent than the sum of uniocular responses. Fixation disparity, as detected with the Mallett unit, is associated with a reduction of the binocular visual evoked potential27 and of binocular visual acuity.28,29,30,31 Similarly, fixation disparity is associated with a reduction in stereo-acuity.32,33,34 Fixation disparity can be induced in normal subjects under abnormal test conditions such as reducing the ambient lighting to mesopic levels35,36 or reading at an unusually close working distance.37 Computer users who prefer longer than average viewing distances have abnormal fixation disparity curves and are more likely to experience symptoms if forced to work at a normal viewing distance.38
Several authors have concluded that fixation disparity tests should include both foveal and peripheral fusion details.39,40,41,42,43,44 The lack of a central fusion lock destabilises45 and increases46 fixation disparity and under these unnatural conditions fixation disparity is therefore a less useful indicator of visual stress.1
Instruments for measuring fixation disparity
Typically, studies have tended to measure fixation disparity using the method of moving monocular markers (bars or lines) until they are aligned in a binocular vernier alignment task. The amount through which the line has to be moved is translated into an angular measurement of fixation disparity. However, instruments that measure the angular fixation disparity tend not to have a central fusion lock so that the monocular marker lines are directly adjacent. This facilitates the vernier alignment task, but leads to higher levels of fixation disparity and less stable results than when a central fusion lock is present.46 Indeed, fixation disparity measurements are affected by a number of target design characteristics47,48 and by inclination of gaze.49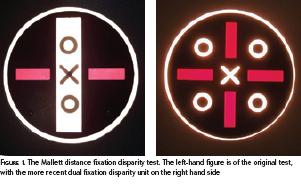
The Sheedy disparometer50 and Wesson card,51 neither of which are widely used in the UK, are examples of instruments that measure the actual fixation disparity. These devices can be used to plot the forced vergence fixation disparity curves showing the effect of horizontal prisms on fixation disparity. Ogle et al52 first described these as four classic types and their clinical relevance was evaluated by Sheedy and Saladin.50 Yekta et al found that the central slope of the forced vergence disparity curve was not significantly associated with symptoms.53
The Mallett Unit
The Mallett unit is perhaps the most commonly found orthoptic instrument in optometric practices in the UK. It detects fixation disparity and determines the prismatic power (associated phoria/aligning prism) or spherical lens power (aligning sphere) that eliminates the fixation disparity1: the Mallett unit does not measure the angular fixation disparity.
 The Mallett distance (Figure 1) and near (Figure 2) fixation disparity tests were designed so that the only disturbances to normal binocularity are the monocularly-viewed Nonius markers54 and the reduction of ambient lighting by the cross-polarising visor. To allow for this reduction in illumination, the ambient lighting should be increased. The original distance test (Figure 1, left-hand figure) employed a target that could be rotated for investigating vertical and horizontal heterophoria independently.55 This was later modified (Figure 1, right-hand figure) so that both horizontal and vertical heterophoria could be assessed without adjusting the test and this was shown to produce similar results to the original design.56 Mallett55 explained some design details by which the distance chart differs from the near unit. On the distance Mallett unit, the Nonius test lines are 18.3 and 5.2 minutes of arc in length and width respectively.
The Mallett distance (Figure 1) and near (Figure 2) fixation disparity tests were designed so that the only disturbances to normal binocularity are the monocularly-viewed Nonius markers54 and the reduction of ambient lighting by the cross-polarising visor. To allow for this reduction in illumination, the ambient lighting should be increased. The original distance test (Figure 1, left-hand figure) employed a target that could be rotated for investigating vertical and horizontal heterophoria independently.55 This was later modified (Figure 1, right-hand figure) so that both horizontal and vertical heterophoria could be assessed without adjusting the test and this was shown to produce similar results to the original design.56 Mallett55 explained some design details by which the distance chart differs from the near unit. On the distance Mallett unit, the Nonius test lines are 18.3 and 5.2 minutes of arc in length and width respectively.
The angular separation of the lines is 20.6 minutes of arc. For the near Mallett unit, the Nonius strips are approximately 26 minutes of arc in length, nine minutes of arc in width, with a separation of 30 minutes of arc at 40cms.56 Ukwade found that fixation disparity is most repeatable when measured with a central fusion lock and Nonius separation of 20 minutes of arc or less.57
Mallett stated that any displacement of one or both strips is important, however small the displacement may appear to the patient.58 The angle of the actual fixation disparity is not very strongly correlated with the magnitude of the aligning prism,59 as would be expected owing to the different types of fixation disparity curves.60
A small number of people perceive a noticeable misalignment of the two Nonius strips without the polarised filters in place. This may be a true 'alignment error', which some people experience on vernier tasks61,62, or may indicate an unreliable patient.1
There are other instruments that measure aligning prism such as the American Vectographic Slides,63,64 the Zeiss Polatest,65,66 Bernell test lantern46, Borish near point card,67 and RMS rotary near point card.68 However, the present paper concentrates only on the Mallett unit since this is the most commonly used fixation disparity test in the UK.
Relationship of fixation disparity and aligning prism with symptoms
The measurement of aligning prism is considered to be a useful clinical test in the investigation of binocular stress but should not be considered in isolation from other test results and must be related to the presence or absence of symptoms.69 Mallett70 claimed that patients with decompensated heterophoria all have fixation disparity with his test; and conversely the absence of fixation disparity demonstrates the adequacy of the fusional reserves to cope with whatever heterophoria may be present. It might be appropriate at this stage to consider the symptoms of decompensated heterophoria, which Evans1 classified into four categories: visual symptoms (blur, diplopia, distorted vision); binocular difficulties (difficulty with stereopsis, improved comfort with monocular viewing, difficulty changing focus); asthenopia (headache, aching eyes, sore eyes); and referred (general irritation). These symptoms are non-specific in that they can arise from other causes, which is why clinical tests are necessary to confirm the diagnosis of decompensated heterophoria.
Mallett70 stated that, in rare cases, decompensated heterophoria might be present without any associated symptoms: if there is deep foveal suppression in one eye as a sensory adaptation to avoid symptoms, lack of critical visual tasks, or if the patient is being tested with a different/new refractive correction. These cases, where decompensated heterophoria is not synonymous with symptomatic heterophoria, are said to be rare affecting only 6 per cent of a clinical sample that exhibited a fixation disparity with the Mallett Unit.70
Studies of fixation disparity tests in the detection of symptomatic heterophoria
Sheedy and Saladin71,72 performed two studies of the relationship between asthenopia and various diagnostic criteria for horizontal imbalances, including fixation disparity. However, they used the Sheedy disparometer, which does not have a good foveal fusion lock.
Yekta and Pickwell73 used a Mallett Fixation Disparity Unit which was modified such that the angular fixation disparity could be measured as well as the aligning prism. They found a low correlation between the magnitude of the heterophoria and fixation disparity. They found no significant difference in heterophoria between symptomatic and asymptomatic subjects, but the symptomatic participants did have significantly higher degrees of fixation disparity.
This agrees with the suggestion of Mallett70 and Sheedy and Saladin72 that fixation disparity is a better indicator of decompensated heterophoria than the degree of heterophoria. Yekta et al69 again found no significant relationship between symptoms and heterophoria, but found that both fixation disparity and aligning prism for near vision are associated with symptoms.
They concluded that, compared with heterophoria, fixation disparity and aligning prism are better indicators of decompensation of binocular vision at near and that they are more useful tests to incorporate in the routine optometric examination.
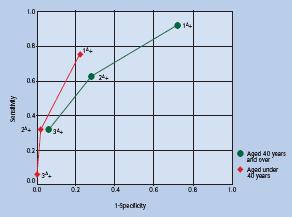 Jenkins et al74 investigated the relationship between aligning prism at near and symptoms. Their data, summarised in Figure 3, suggest that if an aligning prism of 1? or more is taken as indicating a test fail for the Mallett test, then the sensitivity would be 75 per cent and specificity 78 per cent for detecting symptomatic heterophoria in pre-presbyopes.
Jenkins et al74 investigated the relationship between aligning prism at near and symptoms. Their data, summarised in Figure 3, suggest that if an aligning prism of 1? or more is taken as indicating a test fail for the Mallett test, then the sensitivity would be 75 per cent and specificity 78 per cent for detecting symptomatic heterophoria in pre-presbyopes.
Pickwell et al75 investigated the relationship between Mallett aligning prism and symptoms. They were unable to demonstrate any useful relationship for distance vision but found that aligning prism can be very useful in the detection of decompensated heterophoria at near.
References
1 Evans B J W. Pickwell's Binocular Vision Anomalies. Investigation and Treatment, 2002; Fourth Edition, Butterworth-Heinemann, Oxford.
2 Tschermak A. cited in Ogle, 1964 Fortgesetzte studien uber binokularsehen. I. uber farbenstereoskopie. Arch f d ges Physiol, 1924; 204, 177-202.
3 Mitchell DE. A review of the concept of 'Panum's fusional areas'. American Journal of Optometry, 1966; 43, 387-401.
4 Mallett RFJ. Fixation disparity-its genesis and relation to asthenopia. The Ophthalmic Optician, 1974 Nov 30, 1159-1168.
5 Nelson J. Binocular vision: disparity, detection and anomalous correspondence. In Textbook of Optometry, 1988; (editors K. Edwards and R. Llewellyn), Butterworths, London, pp.217-237.
6 Cline D, Hofsteller HW, Griffin JR. Dictionary Of Visual Science, 1989; (4th Edition), Radnor P A Chilton: 205.
7 Dowley D. Fixation disparity. Optometry and Vision Science, 1989; 66, 98-105.
8 Carter DB. Parameters of fixation disparity. Am J Optom Physiol Opt, 1980; 57, 610-617.
9 Sheedy JE. Actual measurements of fixation disparity and its use in diagnosis and treatment. Journal of the American Optometric Association, 1980; 51, 1079-1084.
10 Carter DB. Studies of fixation disparity-historical review. American Journal of Optometry and Physiological Optics, 1957; 34, 320-329.
11 Volkmann AW. Die stereoskopischen Erscheinungen in ihrer Beziehung zu der Lehre vom den identischen Netzhautpunkten. Arch f Ophthalmology, 1859; 5:1-100.
12 Ogle KN. Analytical treatment of the longitudinal horopter: its measurement and application to related phenomena, especially to relative size and shape of ocular images. J Optic Soc Amer, 1932; 22:665-728.
13 Brecher GA. Form und Ausdehnung der Panumschen Areale bei Fovealem Sehen. Arch f d Ges Physiol, 1942; 246:315-328.
14 Ogle KN. Researches in Binocular Vision, 1964; New York: Hafner: 69-93.
15 Steinman SB, Steinman BA, Garzia RP. Foundations of Binocular Vision. A Clinical Perspective, 2000; McGraw Hill Companies.
16 Reading RW. Comparison of two fixation disparity determinations. Optometry and Vision Science, 1989; 66, 612-615.
17 Ogle KN, Martens TG, Dyer JA. Oculomotor Imbalance in Binocular Vision and Fixation Disparity. Philadelphia: Lea and Febiger, 1967; 145-151: 75-119.
18 Schor CM. Fixation disparity: a steady state error of disparity -induced vergence. American Journal of Optometry and Physiological Optics, 1980; 57, 618-31.
19 Schor CM, Ciuffreda KJ eds. Vergence Eye Movement. Basic and Clinical Aspects, 1983; Butterworths, London: 465-516.
20 Fender DH, Julesz B. Extension of Panum's fusional area in binocularly stabilized vision. Journal of the Optical Society of America, 1967; 57, 819-830.
21 Hyson MT, Julesz B, Fender DH. Eye movements and neural remapping during fusion of misaligned random dot stereograms. Journal of the Optical Society of America, 1983; 73, 1665-1673.
22 Erkelens CJ, Collewijn H. Eye movements and stereopsis during dichoptic viewing of moving random dot stereograms. Vision Research, 1985; 25, 1689-1700.
23 Collewijn H, Steinman R M, Erkelens C J, Regan D. Binocular fusion, stereopsis and stereoacuity with a moving head. In Vision and Visual Dysfunction, 1991; (ed J Cronly-Dillon), Macmillan, London, pp. 121-136.
24 Mallett RFJ. Fixation disparity-its genesis and relation to asthenopia. The Ophthalmic Optician, 1974; Nov 30, 1159-1168
25 Mallett RFJ. Techniques of investigation of binocular vision anomalies. In Textbook of Optometry, 1988; (editors K.H. Edwards and R.D Llewellyn) Butterworths, London, pp238-269
26 Joshua and Bishop. Binocular single vision and depth discrimination. Receptive field disparities for central and peripheral vision and binocular interaction on peripheral single units in cat striate cortex. Exp Brain Research, 1970; 10, 389-416.
27 Heravian-Shandiz J, Douthwaite WA and Jenkins TCA. Effect of induced fixation disparity by negative lenses on the visually evoked potential wave. Ophthal Physiol Opt, 1993; 13, 295-298.
28 Pickwell LD, Kaye NA and Jenkins TCA. Distance and near readings of associated heterophoria taken on 500 patients. Ophthalmic and Physiological Optics, 1991; 11, 291-296.
29 Jenkins TCA, Abd MF, Pardhan S and Murgatroyd RN. Effect of fixation disparity on distance binocular visual acuity. Ophthal Physiol Opt, 1994a;14, 129-131.
30 Jenkins TCA, Abd MF and Pardhan S. The effect of artificially created fixation disparity on near visual acuity. Optom Vis Sci (Supp), 1994; 647-648.
31 Jenkins TCA, Abd M and Pardhan S. Clinical research note: fixation disparity and near visual acuity. Ophthal Physiol Opt, 1995; 15, 53-58.
32 Cole RG and Boisvert RP. Effect of fixation disparity on stereo-acuity. Am J Opom Physiol Opt, 1974; 51, 206-213.
33 Saladin JJ. 'Starkfest' vision and clinic science special issue effects of heterophoria on stereopsis. Optometry and Vision Science, 1995; 72, 487-492.
34 Ukwade MT, Bedell HE and Harwerth RS. Stereopsis is perturbed by vergence error. Vision Research, 2003; 43, 181-193.
35 Pickwell D, Yekta AA and Jenkins TCA. The effect of reading in low illumination on fixation disparity. American Journal of Optometry and Physiological Optics, 1987; 64, 513-518.
36 Pickwell LD, Jenkins TCA and Yekta AA. Fixation disparity in binocular stress. Ophthal Physiol Opt, 1987; 7 (1) pp37-41
37 Pickwell LD, Jenkins TCA and Yekta AA. The effect on fixation disparity and associated phoria of reading at an abnormally close distance. Ophthalmic and Physiological Optics, 1987; 7, 345-347.
38 Jaschinski W. The proximity-fixation-disparity curve and the preferred viewing distance at a near visual display as an indicator of near vision fatigue. Optometry and Vision Science, 2002; 79, 158-169.
39 Brautaset RL and Jennings JA. Measurements of objective and subjective fixation disparity with and without a central fusion stimulus. Med Sci Monit, 2006; 12, MT1-MT4.
40 Carter DB. Fixation disparity with and without foveal fusion contours. American Journal of Optometry Arch Am Acad Optom, 1964; 41, 729-36
41 Hebbard FW. Foveal fixation disparity measurements and their use in determining the relationship between accommodative convergence and accommodation. American Journal of Optometry, 1960; 37, 3-26.
42 Jampolsky A. Esotropia and convergent fixation disparity of small degree: differential diagnosis and management. Am Journal Ophthalmol, 1956; 41, 825-33
43 Lyons JG. Fixation disparity researches Part 1-8 Optician, 1966; 151,152 etc.
44 Ogle KN, Mussey F, Prangen A de H. Fixation disparity and the fusional processes in binocular single vision American Journal of Ophthalmology, 1949; 32(8), 1069-87.
45 Wildsoet CF and Cameron KD. The effect of illumination and foveal fusion lock on clinical fixation disparity measurements with the Sheedy disparometer. Ophthalmic and Physiological Optics, 1985; 5, 171-178.
46 Brownlee GA and Goss DA. Comparisons of commercially available devices for the measurement of fixation disparity and associated phorias. Journal of the American Optometric Association, 1988; 59, 451-460.
47 Goss DA and Patel J. Comparison of fixation disparity curve variables measured with the Sheedy disparometer and the Wesson fixation disparity card. Optometry and Vision Science, 1995; 72 (8), 580-588.
48 Ukwade MT. Effects of Nonius line and fusion lock parameters on fixation disparity. Optometry and Vision Science, 2000; 77, 309-320.
49 Jaschinski W, Koitcheva V and Heuer H. Fixation disparity, accommodation, dark vergence and dark focus during inclined gaze. Ophthal Physiol Opt, 1998; 18, 351-359.
50 Sheedy JE and Saladin JJ. Exophoria at near in presbyopia. Am J Optom Physiol Opt, 1975; 52 (7), 474-481.
51 Weeson MD, Koenig R. A new clinical method for direct measurement of fixation disparity. South Journal of Optometry, 1983; 1, 48-52.
52 Ogle KN, Martens TG, Dyer JA. Oculomotor Imbalance in Binocular Vision and Fixation Disparity. Philadelphia: Lea and Febiger, 1967; 145-151: 75-119.
53 Yekta AA, Pickwell LD, Jenkins TCA. Binocular vision, age and symptoms. Ophthalmic and Physiological Optics, 1989a; 9, 115-120.
54 Goss DA. Ocular accommodation, convergence and fixation Disparity: A Manual of Clinical Analysis (2nd Edition), 1995; Butterworth-Heinemann.
55 Mallett RFJ. A fixation disparity test for distance use. Optician, 1966; 152, 1-8.
56 Mallett RFJ and Radnan-Skibin R. The new dual fixation disparity test. Optometry Today, 1994; March 14th, pp 32-34.
57 Ukwade MT. Effects of Nonius line and fusion lock parameters on fixation disparity. Optometry and Vision Science, 2000; 77, 309-320.
58 Mallett RFJ. A new fixation disparity test and its applications. Optician, 1983; 186, 11-15.
59 Pickwell LD. Significance of the central binocular lock in fixation disparity and associated heterophoria, Trans International Congress. Frontiers of Optometry, British College of Optometrists, 1984; 1, Pgs 108-113.
60 Ogle KN, Martens TG, Dyer JA. Oculomotor Imbalance in Binocular Vision and Fixation Disparity. Philadelphia: Lea and Febiger, 1967; 145-151: 75-119.
61 Tomlinson A. Alignment errors. The Ophthalmic Optician, 1969; April 5, 330-341.
62 Jaschinski W, Brode P, Griefahn B. Fixation disparity and Nonius bias. Vision Research 1999; 39, 669-677.
63 Griffin JR and Grisham JD. Binocular Anomalies. Diagnosis and Vision Therapy (3rd Edition), 1995; Butterworth-Heinemann.
64 Goss DA. Ocular accommodation, convergence and fixation. Disparity: A Manual of Clinical Analysis, 1995; (2nd Edition), Butterworth-Heinemann.
65 Haase HJ. Binocular testing and distance correction with the Berlin Polatest (Transl W. Baldwin) Journal of the American Optometric Association, 1962; 34, 115-124.
66 Cameron KD. The effect of fixation disparity on the size of Panum's fusional area. Aust J Optom, 1982; 65, 12-16.
67 Borish IM. The Borish near point chart. Journal of American Optometric Association, 1978; 49, 41-44.
68 Goss DA. Fixation disparity. In Clinical Procedures in Optometry, 1991; (eds Eskridge J, Amos J, Bartlett J) Lippincott Co, Philadelphia.
69 Yekta AA, Jenkins T, Pickwell D. The clinical assessment of binocular vision before and after a working day. Ophthalmic and Physiological Optics, 1987; 7, 349-352.
70 Mallett RFJ. Fixation disparity-its genesis and relation to asthenopia. The Ophthalmic Optician, 1974; Nov 30, 1159-1168.
71 Sheedy JE, Saladin JJ. Phoria, vergence and fixation disparity in oculomotor problems. American Journal of Optometry and Physiological Optics, 1977; 54(7), 474-478
72 Sheedy JE, Saladin JJ. Association of symptoms with measures of oculomotor deficiencies. American Journal Optometry and Physiological Optics, 1978; 55(10), 670-676.
73 Yekta AA and Pickwell LD. The relationship between heterophoria and fixation disparity. Clinical Exp Optometry, 1986; 69, 228-231.
74 Jenkins TCA, Pickwell LD, Yekta AA. Criteria for decompensation in binocular vision. Ophthalmic and Physiological Optics, 1989; 9, 121-125.
75 Pickwell L D. Significance of the central binocular lock in fixation disparity and associated heterophoria, Trans International Congress. Frontiers of Optometry. British College of Optometrists, 1984; 1, Pgs 108-113.
? Rajula Karania was postgraduate research optometrist at City University and is specialist optometrist at Moorfields Eye Hospital. Bruce Evans is visiting professor at City University and director of research at the Institute of Optometry
