
Myopia management is, for good reason, a very hot topic in optometry circles at the moment. In a busy clinic, it can be hard to make time to talk to potential patients and their parents about the options now available to them. But it is vitally important to (or arguably, in the author’s humble opinion, negligent not to) inform every emerging myope of the evidence-based options available to allow an informed decision to be made as to whether to proceed or not with a management plan.
In this article, I present a case recently seen in my practice, where we have utilised the new Topcon MYAH combined topographer, biometer and dry eye diagnostics to address the key aspects for consideration in her case (figure 1).
There are a number of key clinical aspects we need to consider when faced with any management decisions concerning young, progressive myopes, emerging myopes and pre-myopes. These include their age, genetics, axial length and lifestyle.
Age and refraction
One of the most significant risk factors for future myopia is if a child is only slightly hyperopic (+0.75DS or less) at age six to seven years.1 If a school-aged child loses 0.50DS or more of age-normal hyperopia in a year, this could also point to future myope, and progression at this age can occur twice as fast as for an 11-year-old.
If you suspect possible pre-myopia, using the MYAH for biometry as a baseline measure at this early stage will allow for accurate future monitoring of axial elongation over time. This is particularly useful given that axial length has been shown to increase in patients up to 18 months prior to myopia onset.
Genetic factors
A good headline number to use with patients and parents is that having one myopic parent increases a child’s risk of developing myopia by three times, having both parents with myopia increases this to six times.
Our patient fit
GGW is a 15-year-old female with paternal history of high myopia (over -6.00DS) and a refractive history as follows:
- First presentation in our clinic in November 2017 complaining of blurry vision noticed on board work since the start of term in September.
- Best corrected visual acuity (non-cycloplegic refraction) was:
- R-1.50 / -0.25 x 180 (6/6)
- L-1.25 / -0.25 x 180 (6/6)
I discussed early intervention with myopia control at this stage, but child seemed very much against the idea. She was given appropriate literature and online links but this was not pursued. Planned six-month follow up.
Although a six-month follow-up was planned, the patient did not return until July 2019 despite reminders. She then stated that she had been getting on ‘OK’ with her glasses, but was aware that her vision, when looking at the board at school, had recently worsened. Her refraction at this time was:
- R-2.00 / -0.75 x 100 (6/5)
- L-2.00 / -0.50 x 80 (6/5)
I further discussed myopic progression and again suggested the option of myopia control. However, the patient and parents wished to first consider all of their options and so we planned either to have contact lens trial appointment or, failing that, a further six-month follow up.
The patient did not then attend for any additional appointments until September 2020, at which time she told of how she was again aware of her vision dropping. Refraction at this time was:
- R-2.75 / -0.75 x 100 (6/5)
- L-2.75 / -0.25 x 80 (6/5)
I had another careful discussion with GGW’s parents and both she and they were now happy to consider myopia control. This was based on them now having borne witness to the deterioration in vision over time.
Conclusion so far
Despite my best efforts to offer earlier intervention and monitoring, the patient had not returned at the planned intervals for review and further discussion. By visit three, GGW was presenting a clear myopic shift pattern which was following that of her father’s high myope. The need for further encouragement into myopia control strategy was clearly indicated by both the pattern of progression and the paternal risk factor.
Axial Length
Axial length measurement is considered the ‘gold standard’ when researching myopia control and, increasingly, is becoming recognised as an important parameter in clinical settings where reducing any axial elongation in order to reduce eye health risk is the ultimate goal. Indeed, there is currently growing opinion among authorities that axial length is a more accurate predictor of myopic complications than refractive error.2 This is particularly relevant when one considers how the different optical components of the eye, each of which contribute towards the overall refraction, may develop at different rates. For example, the corneal curvature and crystalline lens thickness may have the effect of reducing the overall measured refractive error over time to that predicted by the measured axial length. However, the ability to measure accurately the axial length allows you to state the risk of myopia for a child and to offer a more reliable follow-up of myopia progression over time than with refractive error alone.
Typical axial length (AL) is between 22 and 25mm. Eyes with an AL of over 26mm are at much greater risk of myopic
complications. Elongation in axial length is normally governed by the emmetropisation process which usually accounts for 0.1mm per year up to age 12.3 The rate of change in axial length has been shown to increase up to 18 months prior to the onset of myopia. Therefore, AL measurement over the time period of pre-myopia or early myopia allows for early diagnosis and earlier intervention. Thus, AL measurement is important for myopia progression diagnosis and control. The MYAH shows a trend analysis of the axial length measurements, helping to monitor axial elongation over time (figure 2).
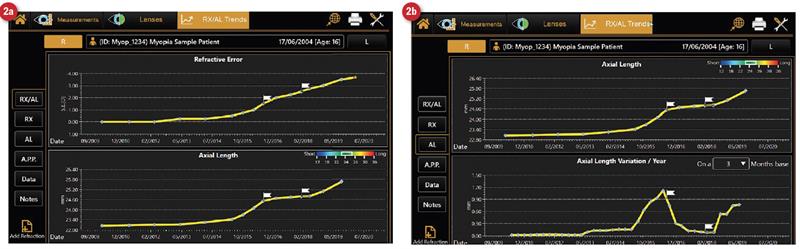 Figure 2: Data output on the MYAH (not for case GGW) showing (a) refractive error and axial length over time and (b) axial length and the rate of change of axial length over time. As variation in length over a given time slows, this will be seen as a dip in the line on the lower graph
Figure 2: Data output on the MYAH (not for case GGW) showing (a) refractive error and axial length over time and (b) axial length and the rate of change of axial length over time. As variation in length over a given time slows, this will be seen as a dip in the line on the lower graph
Our patient fit
At the September 2020 visit from GGW, biometry was undertaken using the MYAH (Topcon Inc, Tokyo, Japan) and axial lengths were measured as follows:
- R 24.87mm
- L 24.66mm
The report from the MYAH plots the axial length alongside the refractive data, both current and historical. For the coming visits, both her refractive data and axial length will be integrated into the MYAH, which will present a longitudinal trend analysis, allowing visualisation of the rate of change over time (figure 2). The benefits of this include visualisation of eye elongation and easy treatment monitoring and demonstration.
Outdoor and lifestyle education
Regarding patient habits and lifestyle, the current evidence base suggests that we should be recommending an average of two hours a day of outdoor time4 to have the optimal effect for delaying or preventing myopia onset. Near work activities of three hours or more outside of school may also have an impact in speeding up myopic shift.5
Our patient fit
GGW does like to play computer games regularly. It would, therefore, seem logical that good advice regarding outdoor time is still valid. That said, this will likely have less of an effect now due to her age and the myopic progression that has already taken place. It is worth noting that the amount of time outdoors has been shown to be less effective at decreasing myopic shift after onset.6 Since GGW was already 12 years old and an established myope at first presentation, and remembering the lack of compliance to myopia management for the preceding three years, any significant impact of advice about outdoors activity might not be expected in this case.
Binocular function
Higher accommodative convergence/accommodation (AC/A) ratios, typically seen with near esophoria, have an increased risk of myopia development,7 but it has also been shown that intermittent exotropia is a risk factor too. Managing these disorders may reduce risk. It is still uncertain as to whether accommodative lag is a risk factor for myopia.
Our patient fit
Binocular status on cover test:
- Distance; orthophoric
- Near; minimal exophoria with rapid recovery
Child and parent education
In a busy clinic, it can be difficult to make time to discuss with patients and parents the risks of myopia progression and the treatments available. However, education is the key to patient compliance. Engaging directly with the child, with the parent an active participant, is considered best practice to engage and encourage the child to take ownership of their treatment plan and follow-up.
Talking in terms of axial length, rather than refractive error, is important in the communication process. It helps to get across the message that it is the eye length that is the issue and high myopia is not just about requiring glasses but instead is related to the impact that a longer eye length can have on increasing the risk of sight-threatening eye disease in the longer term. This approach better encourages an informed decision about the best opportunity for successful treatment. Using online resources, educational videos and materials to support discussions is vital in securing enthusiastic engagement from both the child and parents. It can also help to maintain a continued point of contact with the practice to answer any questions or concerns and so help give reassurance to the family.
Our patient fit
Despite my best efforts to offer early intervention and close monitoring, initially GGW neither accepted treatment nor returned at the planned intervals. By the third visit, almost three years after she first came to our clinic, she presented with a clear myopic shift.
Education, leaflets and videos directed at the patient, with active parent engagement and participation, helped to encourage GGW to engage with myopia treatment, rather than solely depending upon her single vision spectacles. Throughout this period, the patient had become more self-conscious in spectacles and more open to the idea of full-time contact lens wear. This is important when one remembers that MiSight contact lens treatment, for example, requires a recommended six days a week, 10 hours a day. Figure 3 shows the MiSight lenses prescribed for GGW in situ. Figure 4 shows the refractive error change over time, including before intervention, and a flat rate of change with
intervention.
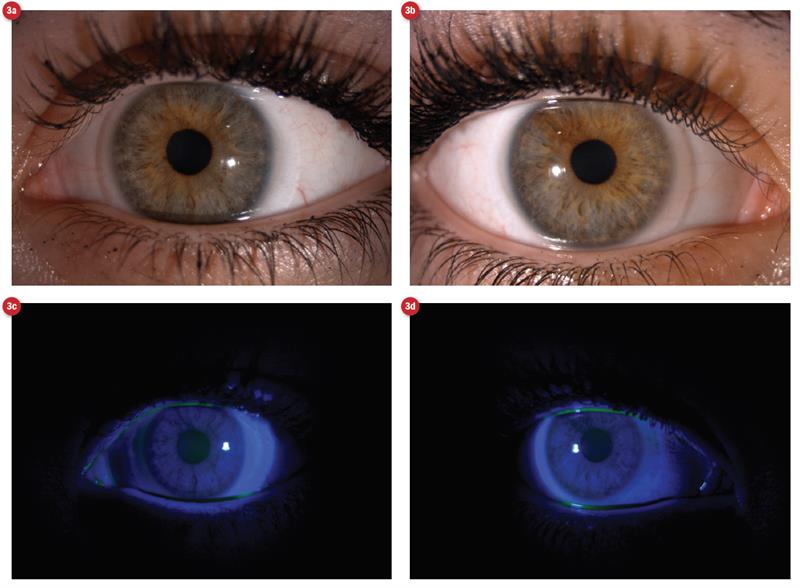 Figure 3: MiSight lenses in situ (a) and (b) under white light and (c) and (d) under blue light
Figure 3: MiSight lenses in situ (a) and (b) under white light and (c) and (d) under blue light
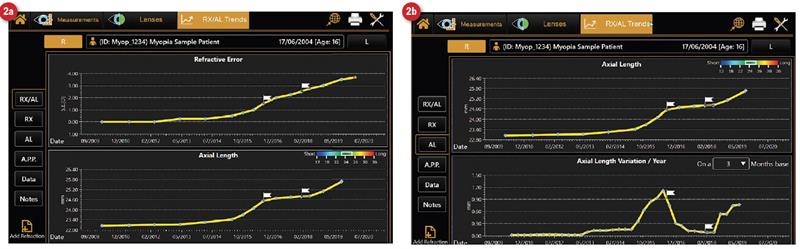 Figure 4: Refractive error and rate of change of error for period before and during intervention for GGW
Figure 4: Refractive error and rate of change of error for period before and during intervention for GGW
Application and Removal Compliance
Ensuring confidence with application and removal (A and R) of contact lenses, while allowing enough time for tuition and safe practice, helps to improve the success rate with initial lens wear at home. Using resources such as guides and videos helps to cement learning and tips at home. Continuing the relationship via a point of contact in the practice is also a valuable resource in case of difficulties during this period.
If changes need to be made to contact lenses in the future, the MYAH onboard database of lenses offers a simulation of orthokeratology lens fit, aiding optimal selection of a lens with minimal placement into the eye (figure 5).
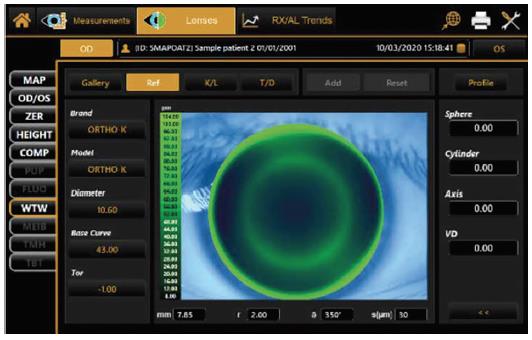 Figure 5: Suggested rigid lens profile for myopia management is calculated by the MYAH from existing data
Figure 5: Suggested rigid lens profile for myopia management is calculated by the MYAH from existing data
Our patient fit
GGW found A and R straightforward, having watched our instructional video screen before starting and having being given clear, structured guidance from our support team member. Follow up video resources were also emailed to her.
Role of the MYAH
The role of the MYAH in a practice providing myopic management services is clear. Being able to quickly and simply generate axial length data at each visit, and to produce a reliable trend analysis to review the rate of axial elongation and rate of refraction change, gives the practitioner the ability to measure directly what it is we are trying to treat.
The use of the latest technology in practice also reassures our patients and their parents that they are receiving the most accurate and up to date care possible. The trend analysis report is clear, concise and easy to explain to patients. The graphical format also improves understanding as it is very easy to comprehend the rate of progression with a simple to interpret plot.
Discussion
As the awareness of treatment options for myopia grows among the population, the need to offer the clinical services associated with this also will. As practitioners, we all have choices to make about what technology to invest in for our clinics. One could easily argue that, in order to meet the growing need for myopia control, we should also be utilising technology that allows us to directly measure, understand and ultimately treat the disease that is myopia.
Sarah Farrant is a therapeutic optometrist with a specialist interest in dry eye disease and myopia management practising in Somerset, UK.
Useful Resources
I strongly recommend the following, excellent website
www.myopiaprofile.com.
References
- Jones-Jordan LA, Sinnott LT, Manny RE, Cotter SA, Kleinstein RN, Mutti DO, Twelker JD, Zadnik K, Ethnicity tCLEo, Refractive Error Study Group. Early Childhood Refractive Error and Parental History of Myopia as Predictors of Myopia. Investigative Ophthalmology & Visual Science. 2010;51(1):115-21.
- Tideman JW, Snabel MC, Tedja MS, et al. Association of Axial Length With Risk of Uncorrectable Visual Impairment for Europeans With Myopia. JAMA Ophthalmology. 2016;134:1355-1363.
- Mutti DO. Endpoints in myopia control studies Ophthalmic & Physiological Optics. 2017:Conference proceedings IMC.
- Xiong, S et al. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmologica 95, 551-556, 2017.
- Rose KA, Morgan IG, Ip J, Kifley A, Huynh S, Smith W, Mitchell P. Outdoor Activity Reduces the Prevalence of Myopia in Children. Ophthalmology. 2008;115:1279-1285.
- Xiong S et al. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmologica 95, 551-556, 2017.
- Mutti DO et al. the CLEERE study Group. Accommodative lag before and after the onset of myopia. Investigative Ophthalmology & Visual Science. 2006;47:837-846
