This is the first in a short series of four different cases treated at Advance VisionCare, Harley Street over the past two years and recorded by Emma Firmager. They are all unique, and present challenges beyond the normal routine of refractive surgery. They show how it is sometimes possible to treat patients who may not have always been included in the past, or who have had complications from previous surgical experiences.
Lasik post radial keratotomy
Case history (DOB: 27/02/59)In 1990 radial keratotomy (RK) was performed in both eyes. The patient's original Rx was approximately - 6 DS R & L. The patient had no accurate records when attending for assessment at the clinic. Having regressed in 1997, the patient underwent R photo refractive keratectomy (PRK) as an enhancement procedure. His motivation to seek further advice last year was due to poor uncorrected acuity (UCVA) and best corrected acuity (BCVA).
The patient had no other ocular or general health complications.
Preoperative refraction
| UCVA | Sph | Cyl | Axis | BCVA | |
| R | 6/15- | +2.50 | -2.75 | 25 | 6/7.5 -1 |
| L | 6/48 | -0.75 | -3.50 | 164 | 6/7.5 -1 |
Bin: UCVA 6/15 - Bin: BCVA 6/7.5
Clinical information
Scotopic pupil size: R 5.5 mm L 5.5 mm
Pachymetry: R 514µm L 545µm
Orbscan keratometry readings:
R 42.5D x 120 Max L 41.5D x 132 Max
R 40.9D x 30 Min L 40.7D x 42 Min
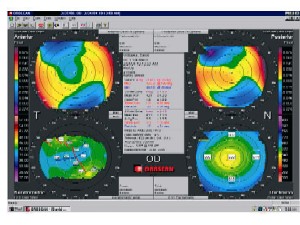
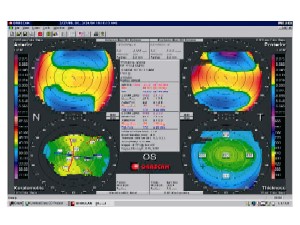
The Orbscan provides information on elevation of the anterior and posterior cornea in addition to axial keratometric maps. This provides detailed information on whether it may be safe to perform laser refractive surgery (Figures 1 and 2).
 |
|
Figure 1 |
 |
|
Figure 2 |
Biomicroscopic examination: Anterior segment clear, but two arcuate corneal cuts at 6 and 12 o'clock in both eyes.
Treatment plan
L PlanoScan (standard, non wavefront) Lasik followed by R PlanoScan Lasik two weeks apart, unilateral treatment
| Sph | Cyl | Axis | Optic zone | |
| R | +2.00 | -2.50 | 25 | 6.2 |
| L | -0.75 | -3.00 | 164 | 6.3 |
Special zero compression Hansotome microkeratome head was used. The optic zone size was chosen depending on the scotopic pupil size. Great care was taken to ensure no damage was caused to the previous RK incisions. The surgery was routine, with no complications for either eye.
Follow up
One day
These appointments were of course on separate dates.
Vision: R 6/12 L 6/7.5 BIN 6/7.5. No refraction is carried out at one day postoperative.
Biomicroscopic examination: Both corneas and interface clear and quiet. Arcuate cuts visible.
Action: Px to continue FML (qds), Exocin (qds) and Snotears (as required) for one week.
One week
Biomicroscopic examination was as before:
| UCVA | Sph | Cyl | Axis | BCVA | |
| R | 6/10 | 0.00 | -1.25 | 110 | 6/7.5 -1 |
| L | 6/7.5 | +0.50 | -0.50 | 20 | 6/7.5 |
Six weeks
Biomicroscopic examination was as before:
| UCVA | Sph | Cyl | Axis | BCVA | |
| R | 6/15- | 0.00 | -1.25 | 110 | 6/7.5 -1 |
| L | 6/7.5 | +0.75 | -0.50 | 10 | 6/7.5 |
At six months postoperative the patient is happy. The R is good for near vision, L for distance. The patient reports doing well.
Conclusion
This was an unusual case in that with Lasik post radial keratotomy there are risks of corneal rupture and the outcome cannot be certain. By careful treatment planning and selection this patient has had a successful outcome and improved quality of life.
- Emma Firmager is an optometrist and professional services manager for Advance VisionCare.
