At the NEG/Independents Day conference in November 2016, Heidelberg Engineering scanned three real patients from optometrist Peter Waite’s practice, KG Miles in Birmingham. All the patients were scanned live on the big screen using the Spectralis Imaging Platform and were assessed for both retinal disease and glaucoma. Their cases were presented in Optician and follow-up examinations were subsequently performed on these patients at Optrafair 2017. A case study is presented below in the last of a three-part series examining how each of the patients has progressed.
The case
A 77-year-old female patient of Afro Caribbean ethnicity attended complaining of reduced vision in the right eye. Previously, the patient had been referred to hospital eye services for a suspected right macular hole on the 12/06/12. The referral had been based upon history, signs and symptoms and clinical examination, prior to any Spectralis OCT assessment.
Subsequent in-practice OCT examination (figures 1 and 2), revealed spontaneously resolved epiretinal membrane (REM) and vitreoretinal traction (VMT). A follow up OCT examination was recommended at next routine sight test.
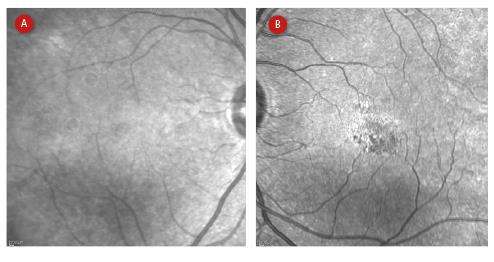
Figure 1: Near IR cSLO fundus imaging of right eye (a) and left eye (b) from 2015
A slight reduction was observed in VA in the left eye and was consistent with VMA. Following consultation with the patient, observation with follow-up OCT assessment was recommended. RPE/photo receptor disruption was also noted; this was likely to be long standing and may be secondary to an old episode of CSCR as its presentation would appear to be unilateral.
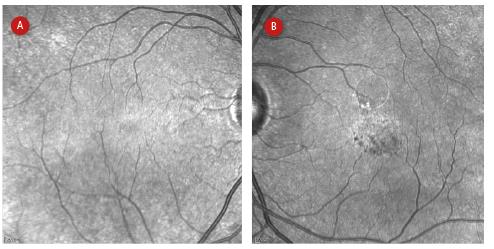
Figure 2: Near IR cSLO fundus imaging of right eye (a) and left eye (b) from 2017
OCT examination right eye
OCT line scans of the right eye show irregular foveal profile (figure 3), with steepened slope of the clivus visible on horizontal and vertical sections. The horizontal section shows an irregular epiretinal surface with interruption of the ILM and RNFL. No significant change observed.
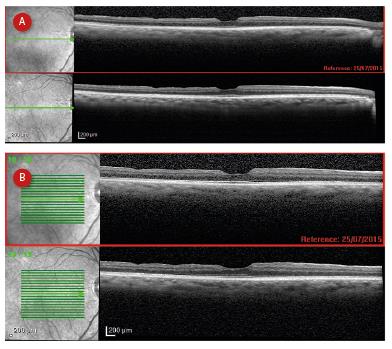
Figure 3: Follow up OCT single line (a) and multiple line (b) scans of the right eye showing irregular foveal profile and comparing newest (lower) with previous (upper) scan
OCT map right eye
The OCT map (figure 4) shows thinning of the retinal inferiorly, with a ‘scalloped’ edge to the thickness map. Once again no significant change observed, with the central macular thickness increased by 1µm.
OCT examination left eye
OCT examination of the left eye showed a shallowed and irregular foveal profile, with central macular thickening (figure 5). A hyper-reflective structure can be observed within the vitreous cavity, with firm attachment at the optic nerve, fovea and temporal to the macular. There is no schisis or cavitation of the retina and the changes observed are consistent with vitreo-macular adhesion (VMA). The follow up examination shows slightly increased VMT and associated macular thickening.
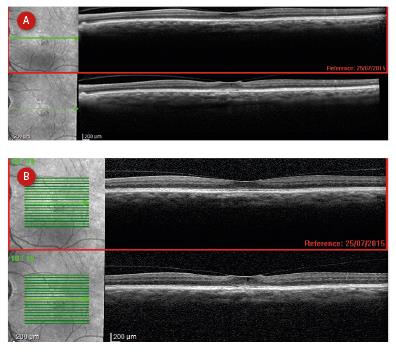
Figure 5: Single (a) and multiple (b) line scans of left eye showing a shallowed and irregular foveal profile, with central macular thickening
OCT map left eye
The OCT colour map (figure 6) shows a shallowing of the foveal depression and an increase in CMT of 29µm. This observed change is consistent with a progressing VMT.
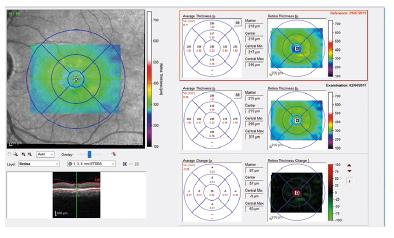
Figure 6: OCT colour map of left eye suggestive of progressive vitreomacular traction
High magnification follow-up OCT examination left eye
The high magnification follow up examination (figure 7) shows increased VMT and further shallowing of the foveal profile. The outer retinal layer now shows an elevation of the RPE-BM complex (red arrow) and a schisis of the RPE-photoreceptor interdigitation zone (yellow arrow), these changes are consistent with progressing VMT.
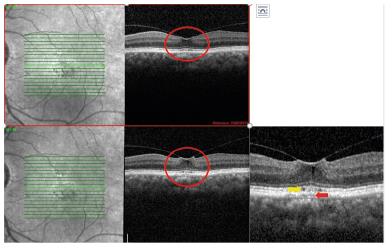
Figure 7: High magnification (area circled) OCT scan showing RPE-BM elevation (red arrow) and a schisis between RPE and photoreceptors (yellow arrow)
Discussion
The right eye shows no progression since the last sight test and OCT examination.
The left eye at presentation demonstrated a slight reduction in acuity which could have been consistent with the VMA observed at that time. OCT monitoring was recommended. At the time of the examination, some RPE/photo receptor disruption was noted. This was thought to be long standing. As the patient has no acute symptoms or visual disturbance, no urgent referral was indicated and it was decided to monitor the patient with OCT.
Follow up examination show progression of the VMT with early macular schisis forming, the patient’s VA remains unchanged and with no visual symptoms. The natural history for VMA/T is to progress to posterior vitreous detachment, therefore continued monitoring with OCT is recommended. The frequency of review should be increased and the patient advised to return if a reduction in VA is noted or new visual symptoms observed.
