In a recent article on hysteresis (Optician 08.03.2019), I described a patient with contact tonometry readings suggesting ocular hypertension.
Case to consider
These were the key findings:
History:
- 36-year-old male, healthy and on no medications
- Had been under the hospital eye service (HES) some four years ago for raised intraocular pressures – had been discharged after initial visit
- No family history of glaucoma
Presentation of right eye today:
- Goldmann applanation tonometry; 24 mmHg
- Central corneal thickness; 535 µm
- Vertical C/D ratio of 0.5
- Full threshold fields; full
Plan:
- Review in two years
I asked, would you agree with this approach?
Key information
So with regard to the updated NG81 guidance1 and the College of Optometrists guidelines relating to ocular hypertension,2 the key points to consider are as follows:
- The patient presents with a repeatable GAT IOP of 24mmHg
- Vertical C/D remains stable (comparison with previous photos was possible)
- Threshold visual fields: Full
Other factors to consider include:
- No family history
- Open angle (VH4)
- The patient is a confirmed ocular hypertensive. However, the future risk of visual impairment had been assessed and deemed of low risk and he had been discharged from HES.
- No obvious conversion detected at today’s visit
Based on this presentation, reassessment in 18 to 24 months would be acceptable.1
Discussion
This case represents a not uncommon presentation of ocular hypertension. Ocular hypertension (OHT) is generally defined as an elevated intraocular pressure (IOP) (greater than 21mmHg) as measured by Goldmann applanation tonometry (GAT) in one or both eyes in the absence of clinical evidence of optic nerve damage, visual field defect or other pathology that could explain high IOP.2 The prevalence for OHT ranges from 4.5% to 9.4% in the population aged over 40 years, carrying a 10% risk of conversion to primary open angle glaucoma within five years.2
Ocular hypertension has historically accounted for 30 to 45% of the referrals into the HES,3-5 and an interpretation of previous
Clinical Pearls about Corneal Hysteresis (CH)
- CH is a measure of the biomechanical properties of the cornea
- CH is generating interest as a predictor of glaucoma risk
- The lower the CH, the greater the risk of glaucoma development and progression
- CH aids in developing management strategies, such as goal IOP and frequency of visits
- The lower the baseline CH, the greater the IOP reduction following various glaucoma therapies
- Can be incorporated into clinical practice and helps refine risk assessment- it is possible to define risk based on CH values as ‘low’, ‘medium,’ or ‘high’
Assigning risk based on IOP and CH:
- Low CH, Low IOP: Moderate/ Low risk: Consider early assessment
- Low CH, High IOP: High risk: Early assessment
- High CH, Low IOP: Low risk: Routine assessment
- High CH, High IOP: Low/ Moderate risk: Consider early assessment
NICE guidelines addressing treatment and diagnosis as relating to referral resulted in high levels of unnecessary referrals.6 A glance at the revised NICE guidelines (which do address referral criteria) suggests that, from the primary care point of view, the threshold of when to refer for OHT is ≥ 24mmHg and a knowledge of the central corneal thickness (CCT) is no longer required. The latter forms part of the diagnosis process and conducted following referral.1
While raised IOP is the strongest risk factor (after age) for primary open angle glaucoma,7 studies have shown that, in isolation, no single IOP level provides sufficiently high sensitivity and specificity for detection of glaucoma.3,8 This reinforces the importance of accurately interpreting IOP in conjunction with optic disc examination and visual field test as an effective screening tool for glaucoma.
Corneal biomechanics measurements
The utilisation of the ORA G3 (figure 1) offers a greater insight into the biomechanics of the cornea. The data gathered can impact on management, and is of particular relevance when considering ocular hypertension.9 Corneal hysteresis (CH) in particular has a potential role, both as an IOP correction factor and as a proxy marker of an individual’s susceptibility to glaucomatous optic neuropathy.10
Data produced by the ORA of interest include:
- Corneal compensated IOP (IOPcc) – the first parameter given by the ORA report. It reveals an estimation of the IOP unaffected by the corneal properties such as central corneal thickness11 and is thought to offer a truer picture of IOP.9
- Goldmann-correlated IOP (IOPg) – correlates with IOP obtained by GAT.12
- Corneal hysteresis (CH) – the difference between the two pressures (P1-P2) measured when the cornea is first applanated on deformation and again when regaining its shape. This parameter is thought to represent the viscoelastic nature of the cornea, or its ‘viscous-damping’ capacity.
CH varies from individual to individual,13 with an average range being quoted from 10.24 to 10.7.14,15 Higher CH appears to indicate a greater viscoelasticity of ocular tissues and may be protective against glaucomatous nerve damage by ‘insulating’ the optic nerve head in patients with ocular hypertension or with existing glaucoma-like optic discs.10 Conversely, lower CH is significantly associated with an increased risk of developing glaucoma and of this progressing more rapidly. A lower CH is more predictive of visual field changes than any other factors.16 Indeed, each 1mmHg lower CH was associated with a 22% increase in the risk of developing glaucoma during follow-up.17
So, will these measure influence our case management presented here? The ORA measurements for this patient are shown in figure 2.
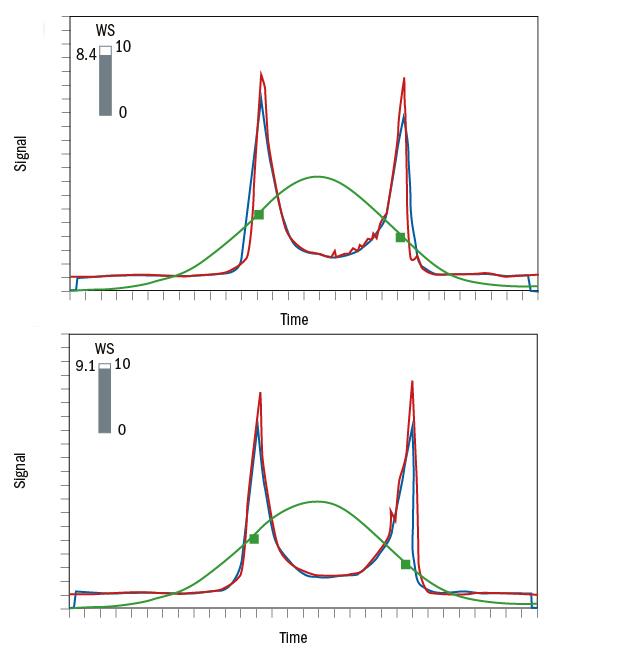
Figure 2: ORA data from the patient
In this case, the patient’s CH falls into the ‘above average’ range which is considered to have a protective role in patients with elevated IOP,18 with a low likelihood of conversion to primary open angle glaucoma.19 Therefore, in this case reassessment in two years is appropriate.
Consider however, a second scenario (figure 3) where the presentation is identical yet the CH reading is in the ‘lower than average’ range. From the preceding discussion, it becomes clear that this patient is at a greater likelihood of conversion and would benefit from an earlier reassessment within one year.

Figure 3: ORA data where the CH reading is lower than average
Corneal biomechanics offers a greater understanding of glaucoma development and more thorough monitoring of progression. Coupled with the prevalence of OHT and the risk of progression in the context of the updated NICE NG81, it is perhaps time to consider integrating corneal hysteresis assessment into routine optometric examinations.
Dr Rohit Narayan is a therapeutic optometrist based in the Midlands.
References
1 Glaucoma: Diagnosis and Management. NICE Guidelines (NG81) 2017: https://www.nice.org.uk/guidance/ng81
2 Ocular hypertension (2018) The College of Optometrists. https://www.college-optometrists.org/guidance/clin...
3 Chan Michelle P Y, Broadway David C, Khawaja Anthony P, Yip Jennifer L Y, Garway-Heath David F, Burr Jennifer M et al. Glaucoma and intraocular pressure in EPIC-Norfolk Eye Study: cross sectional study BMJ 2017; 358: j3889
4 Lockwood AJ, Kirwan JF, Ashleigh Z. Optometrists referrals for glaucoma assessment: a prospective survey of clinical data and outcomes. Eye (Lond) 2010;358:1515-9.
5 Khan S, Clarke J, Kotecha A. Comparison of optometrist glaucoma referrals against published guidelines. Ophthalmic Physiol Opt 2012; 358: 472-7
6 Glaucoma: Diagnosis and Management. NICE Guidelines (NG85) 2009 https://www.nice.org.uk/guidance/cg85
7 Burr JM, Mowatt G, Hernández R, et al. The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation. Health Technol Assess2007;358:iii-iv, ix-x, 1-190. doi:10.3310/hta11410 pmid:17927922.
8 Tielsch JM, Katz J, Singh K, et al. A population-based evaluation of glaucoma screening: the Baltimore Eye Survey. Am J Epidemiol 1991; 358:1102-10.
9 Dascalescu D, Corbu C, Vasile P, et al. The importance of assessing corneal biomechanical properties in glaucoma patients care - a review. Rom J Ophthalmol. 2016;60(4):219-225.
10 Murphy, Melissa L., et al. “Corneal hysteresis in patients with glaucoma-like optic discs, ocular hypertension and glaucoma.” BMC ophthalmology 17.1 (2017): 1.
11 Luce DA. Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. J Cataract Refract Surg 2005;31(1):156-62.
12 Yaoeda, Kiyoshi, et al. “Comparison of intraocular pressure adjusted by central corneal thickness or corneal biomechanical properties as measured in glaucomatous eyes using noncontact tonometers and the Goldmann applanation tonometer.” Clinical ophthalmology (Auckland, NZ) 10 (2016): 829.
13 Deol M, Taylor DA, Radcliffe NM. Corneal hysteresis and its relevance to glaucoma. Curr Opin Ophthalmol. 2015;26(2):96-102.
14 Shah S, Laiquzzaman M, Bhojwani R, Mantry S, Cunliffe I. Assessment of the biomechanical properties of the cornea with the ocular response analyzer in normal and keratoconic eyes. Invest Ophthalmol Vis Sci 2007;48:3026–31.
15 Carbonaro F,Andrew T,Mackey DA, etal. The heritability of corneal hysteresis and ocular pulse amplitude: a twin study. Ophthalmology 2008; 115:1545– 1549.
16 De Moraes CV, Hill V, Tello C, Liebmann JM, Ritch R. Lower corneal hysteresis is associated with more rapid glaucomatous visual field progression. J Glaucoma. 2012;21(4):209-213
17 Susanna, Carolina N., et al. “A prospective longitudinal study to investigate corneal hysteresis as a risk factor for predicting development of glaucoma.” American Journal of
