Female patient HG, age 65, presented as a PEARS patient on 16.03.2017 complaining of difficulty removing her right contact lens for approximately the last two weeks, only succeeding in doing so after a period of around seven days continuous wear. The iris appeared to be bluish in colour upon removal, while the LE iris was its usual brown.
Upon questioning, HG stated there was initial soreness, that had now subsided, but no pain. The eye was slightly sticky upon waking and she felt that there was minimal vision in the right eye at present. HG had no back up glasses and presented wearing her left RGP contact lens as her only means of correction. The last sight test and aftercare had been 20 years ago and, yes, the RGP contact lenses were also 20 years old!
HG had only presented today because her relatives had forced her to see an optician. She had been wearing these lenses seven days a week, 6am to midnight, and using a two-step peroxide cleansing regime. She confessed to sleeping in the lenses on occasion and the contact lens case had not been replaced over the 20-year period. The contact lenses were for distance correction with ready readers worn to improve near visual acuity.
Clinical data
POH – no history of HES treatment/trauma
FH – no family history of AMD/diabetes/glaucoma
General health – hypertension, arthritis, smoker
Medication – thyroxine, analgesics (tramadol, naproxen, dihydrocodeine)
R vision; Light perception (LP)
L corrected VA 6/9-
Slit lamp biomicroscopy:
- Meibomian gland dysfunction
- Blepahritis
- G4 conjunctival injection
- Limbal injection
- Neovascularisation ~1.5mm inferiorly
- Corneal haze and opacification with minimal superior sparing
- The anterior chamber, lens and retina were not visible through the corneal opacification.
Signs and symptoms of microbial keratitis include redness, pain, photophobia, discharge and a reduction in visual acuity. However, HG had not presented with pain, but rather an initial soreness that had since subsided. This may be attributed that HG was on three types of painkiller at the time which may have masked the pain.
Redness and yellowing of the cornea had also not been noticed. Upon asking about changes in the corneal appearance, HG said she ‘did not look in the mirror at herself very often.’ Photophobia was not reported at all, surprisingly, perhaps also being masked by the high dosage painkillers. The only reported symptom of significance to HG was the stickiness in the morning, but HG did not find this to be a major concern.
This patient was fortunate to be seen promptly in clinic via the PEARS scheme which has been operating in our area since 2011. She was understandably concerned but for some reason had delayed coming.
Referral
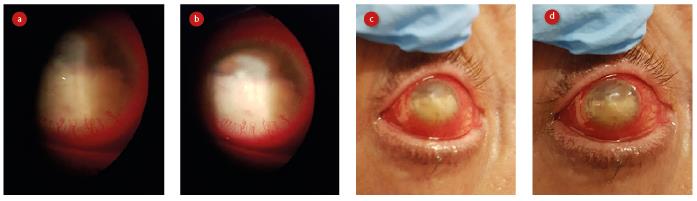
Figure 1a-d: Appearance of eye at first presentation
HG was referred promptly to Moorfields Eye Hospital (MEH) and advised to take her contact lens case for microbial analysis. Case records were obtained (with full permissions) from MEH and the findings are summarised below.
- 16.03.2017: Seen by corneal fellow at MEH. Corneal ulcer with small perforation diagnosed. Corneal scrape was performed; perforation glued and a bandage contact lens (BCL) applied; Oral moxifloxacin 400mg and topical moxifloxacin 0.5% prescribed (see figure 1).
- 17.03.2017: Seen by corneal fellow. HG felt her eye to be more comfortable and a hypopyon of ~5mm was diagnosed. Underlying tissue was thought to be friable and a descemetocele was found centrally with a pinpoint leak. A 3mm patch of glue was applied to seal the leak and another BCL applied. A B-scan ultrasound was ordered to rule out endophthalmitis. Patient was then examined by the consultant on call who found a relative afferent pupillary defect (RAPD), probably caused by the hypopyon covering the pupil. HG was advised of the symptoms of perforation and asked to return immediately were they to arise. Otherwise a three-day recall was advised.
- 20.03.2017: RE vision with BCL still light perception (LP), LE VA with current RGP CL 6/6-1. HG felt the eye to be less sticky. Glue was still in place and hypopyon, although still ~5mm in size, found to be more organised temporally. The anterior chamber appeared deeper than at the last visit and now distinct from the hypopyon. HG was advised to taper moxifloxacin down to once a day and to complete the course of oral moxifloxacin. Corneal scrape results from micropathology were inconclusive and showed no Herpes simplex, bacterial, fungal or Acanthamoeba infection.
- 27.03.2017: Seen by corneal fellow. Moxifloxacin drops were being used six times per day. Hypopyon had cleared and an active infiltrate was found adjacent to the glue patch. RAPD was once again suspected. IOP measured digitally R20mmHg, L20mmHg. A new scrape was ordered and the BCL replaced.
- 03.04.2017: Hyperaemia now graded as ++, infiltrate clearer, and a 1mm hypopyon found inferiorly. HG advised to continue with moxifloxacin 6x per day and dexamethasone 0.1% single unit doses prescribed to apply topically four times a day. Two-week recall recommended.
- 21.04.2017: R vision with BCL remained LP. L VA using current RGP CL 6/6. No corneal leakage, glue in place, no active infiltrate found. BCL replaced and HG asked to taper dexamethasone down to once a day, moxifloxacin to be continued as before. Four-week recall advised (figure 2).
- 26.05.2017: Using glasses, R acuity hand movements (HM), L 6/36 improving to 6/12 using pinhole. On this occasion, HG felt her eye was gritty. Rescrape revealed no culture growth and PCR was negative (PCR, or polymerase chain reaction, allows for a rapid and highly specific diagnosis of infectious diseases, including those caused by bacteria or viruses). On examination, the iris was reported to be ‘pluggy’, with corneal glue still in place. No IOP measurements were possible digitally. BCL replaced. Four-week recall advised.
- 23.06.2017: Using glasses R acuity was LP, L 6/12, improving to 6/6 using pinhole. IOPs measured as R16mmHg, L15mmHg. Anterior chamber found to be patent peripherally. Glue in place, and could not be dislodged with spears (figure 3). Anterior OCT showed healing underneath, but image was incomplete. Plan was made to repeat B-scan ultrasound, BCL was replaced and advice was given to continue with drops. Rehabilitation was discussed and HG was advised that when the glue falls off or dislodges, an RGP CL could be applied in the future to the RE to improve VA. Failing that, HG may need penetrating keratoplasty (PK), synechiae removal and perhaps cataract surgery (though no lens view at present made confirmation impossible at this stage). Three-week recall advised.
- 07.07.2017: Using glasses, R acuity was HM, L 6/12, improving to 6/9 using pinhole. IOP R14mmHg, L16mmHg using iCare (rebound tonometer). BCL had fallen out three days prior to this appointment and HG reported a subsequent slight increase in discomfort. Once again, the glue did not dislodge with a spear but most of it was removed using forceps. There was no epithelialisation beneath the glue. The BCL was replaced. HG was informed that, given the location of the central scar, the iris plug and small pupil, even after re-epithelialisation and remnant glue removal, a RGP lens would be unlikely to improve vision and that HG would more than likely need a PK. One-month recall.
- 11.08.2017: VA using glasses R HM, L 6/6-1. IOP using iCare R22mmHg, L13mmHg (with BCL in situ in RE). External examination found a central scar, complete epithelialisation and anterior synechiae. Tropicamide allowed some superior dilation. HG was given atropine to use in the right eye in order to break the synechiae and asked to consider PK, which she was not particularly keen upon.
To date
HG missed her September appointment at MEH and the next was scheduled for the end of October 2017 (yet to take place at time of writing). Some vision has returned to the RE and HG can make out shadows and shapes.
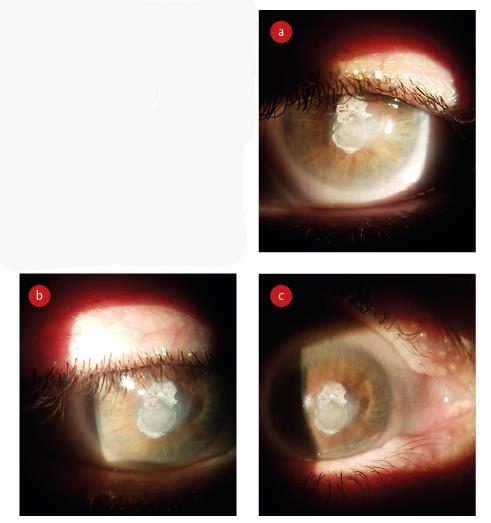
Figure 3: Appearance of eye after 10 weeks
She is still applying atropine daily and feels the latter has contributed to the improvement in VA. However, the improvement in RE VA has brought about with it some disorientation and so she has decided to go ahead with the PK and will inform the HES of her intentions at the next appointment.
This case represents a dramatic illustration of what can happen if aftercare visits are ignored. It also shows how severe damage can occur without any symptoms felt of major concern by a patient.
Farah Awan is an optometrist practising in South London.
