Two years on from the start of my eye problems, and some 30 eye clinic visits later I am starting to feel it is time to accept and hopefully adapt to my wavy world and get on with life.
I don’t like to think about the hours my poor husband has wasted driving me to appointments then sitting around waiting for me to be finished before driving us home. It is just as well neither of us need to rely on a steady wage from full-time work. I doubt any employer would have been happy with the time off we would have needed, often at short notice. I don’t like to even think about how much money we could have been earning in our respective self-employed work.
From eye care provider to eye care recipient
In those two years I have gone from being an experienced, qualified eye care professional delivering optometric services on the high street to being a naïve but frequent user of hospital-based eye clinic services. The staff have always been friendly and helpful but there is definitely a cattle market air to being in any hospital environment. The staff share friendly banter and platitudes but I found there was no real feeling of permanence or even continuity.
Staff are constantly having to search for forms and pieces of equipment that should be to hand. They all come across as proficient in their area of expertise but too often had little understanding of the wider hospital organisation; for example, what time other departments close for the day. Despite digitisation, patient records are often not to hand so staff have to rely on the patient for a history. In a high street practice a lost (or misplaced) patient record is a major cause of concern because any practitioner is well aware of the well-intentioned but distorted histories that patients relate.
How it began
My story started simply enough with floaters. As a medium to high myope, I had always seen small floaty bits in my field of vision but these new ones were more intrusive. I assumed, given my age, that they were probably the result of a posterior vitreous detachment, so no immediate cause for concern.
However, having done a battery of subjective tests on myself, I was worried enough to make an appointment with a colleague who had an Optomap. This meant I would be able to see for myself whether my retina appeared intact. By then I did have a slight reduction in acuity (possibly due to early cataract) and evidence that maybe I should get my blood pressure checked. However, there were no visible signs to indicate that anything was amiss.
But sometimes intuition takes over. We both felt that something was going on that justified requesting a referral to ophthalmology. Maybe if I had had a colleague with an OCT our suspicions might have confirmed and faster action would have been instigated.
Since blood pressure is routinely checked twice by a practice nurse, it was nearly a month before I got to speak to my GP and realised she had not acted on the referral letter. Fortunately, she did listen to me and agreed to refer me on to an ophthalmologist. In retrospect, I wondered if cataract surgery would sort out some of my concerns.
For some months I had been contemplating purchasing a new ophthalmoscope, or at least getting my current one serviced. Vision through it was like looking through a dirty lens. Whenever possible I preferred to supplement my ophthalmoscopic view with fundus photography. I have come to understand more recently that many practitioners rely less on their trusted ophthalmoscope, increasingly using alternative forms of imaging the fundus.
Unfortunately, my practice owner insisted that patients paid for this additional service and, even though this was 2015-16, most people (at least in the area I worked) still objected to paying for a private sight test. So very few were agreeable to paying extra for supplemental tests.
First eye clinic visit
I finally made it to the eye clinic. It still took a few months, but despite seeing several different ophthalmologists and having numerous tests (blood tests. X-rays, MRIs, fluorescein angiography and finally OCT), no definitive cause for my symptoms were found. Vision remained only slightly blurred, though over time black clouds of threads and centrally distorted vision did supplement my chunky floaters. Topical and systemic steroids were started because, as I understood it, there were some signs of inflammatory disease.
High street opticians are increasingly using OCTs routinely, but my old school senior consultant seemed content to rely on his view of the fundus using indirect ophthalmoscopy and more traditional tests. Fortunately, thanks to a more recently qualified locum ophthalmologist, I did have an OCT scan.
I remember having to remind the ophthalmologist at my follow up appointment that there were results from other investigations to be viewed – whether my records would have flagged up if there had been any issues I don’t know. So far as I was told the OCT was the only test that confirmed anything significant, showing a ragged internal limiting membrane and inflammatory response within the retinal layers.

Despite repeated requests and them knowing my background as an optometrist, I don’t think I was given any more information about what was happening than any other patient. I was permitted a brief view of my OCT scan, but any opportunity for careful examination came from subsequent discussion with optometric colleagues.
They would have welcomed more detailed information than I was able to give. Words like vitritis and anterior, posterior or pan uveitis simply acknowledge the ocular areas where signs of inflammatory response were present. Ophthalmology has come a long way in the last century but there is still so much that that is being discovered.
Epiretinal membrane
Having completed my last course of steroids I was surprised when the consultant on that day started talking about having epiretinal membrane peels. I had assumed there was nothing further that could be done s and had been expecting to simply be discharged so this came as a shock. I had though I should just be grateful that my vision seemed to have stabilised at a level where I could still drive and read although it still prevented me from seeing clearly with an ophthalmoscope.
As we had recently moved over 60 miles away from this hospital, and the travelling had been time consuming for routine check-ups, I did not want to be so far away if I needed to have more intrusive surgery.
I asked if it was OK to change hospitals. I had earlier been advised not to change hospitals mid-treatment but to wait till things had quietened down. At which point the consultant annoyed me by saying that it was OK to just speak to my GP when I was ready to be referred to a local eye clinic. Nowadays in most areas, eye clinic referrals are more likely to be organised by optometrists.
I knew I wanted to discuss this with a local optometrist to find out which hospital eye clinics they would recommend for epi-peels. My problem now was how to decide which practice to make an appointment with. None of my previous colleagues had any local contacts and,while a Google search told me something about the technology some local practises offered, it told me nothing about the people.
Speaking to neighbours, they seemed to go for the cheap multiples; but I knew I wanted an independent. All I could do was make an appointment and hope for the best.
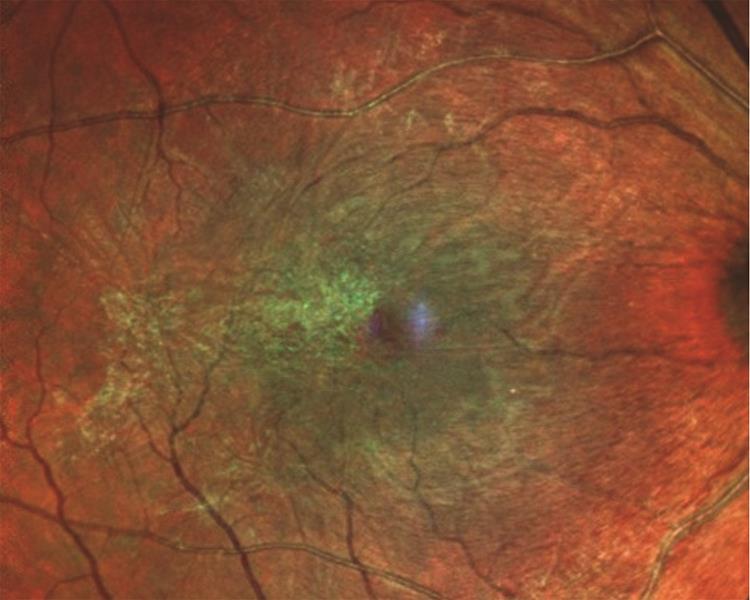
Figure 2: Epiretinal membrane peeling is one management option
After treatment
A year later and epi-peel and cataract surgery on each eye has at least banished the physical dark clouds of tangled threads that had added to what I now acknowledge was probably a dark cloud of depression caused by not knowing what the future might hold.
From my perspective, surgical and medical treatments have addressed the structural damage so my potential for clear and even sharp acuity has been improved but has left my vision distorted. Straight lines may be in sharp focus but are wavy which makes fusion difficult. So, whilst monocular vision is improved, I am still finding everyday life an effort.
I have been lucky. I hope that my future will not be adversely affected by the level of impaired vision I have. I know that there are alternative ways of ‘seeing’ the world that I could use if my vision was more affected but I am not sure how well I would cope with learning how to use them.

General reflections
I feel my binocular vision difficulties were aggravated by the time I had to spend ‘getting by’ with poor vision whilst awaiting the next surgical intervention. I understand the surgeons needed to be sure that my eyes had settled following the last procedure before attacking them again, but it has meant the last two years I have been in a state of limbo, hoping it would not be necessary to relearn new ways of seeing and doing because ‘normal vision will be restored’ as soon as possible.
My wavy vision is definitely better than with the dark clouds that had distorted my vision. My new spectacles have restored my driving vision, for which I am grateful, but reading and writing is still a battle. Hopefully, near vision exercises will give me control over my near diplopia, but only time will tell.
When reading, I am aware that I like to scan the text quickly, and this is one reason why I currently struggle. If I take my time and give my eyes time to make the effort to come together to recognise each word, then I can see clearly and singly. But then I lose the thread of what I am reading or writing.
While struggling to see clearly, I realised how important memory was. Or to put it another way, how clear sight makes us lazy about using our memory in everyday life. I was aware that I needed to pay more attention to my sense of touch. I had to take time to ensure I had a firm grasp of an object using both hands or it would tumble to the floor. When doing anything, I needed to remember more precisely where I was relative to what I wanted to do. Having impaired vision is mentally hard work.
It was and still is necessary to limit any activities that require vision, as the mental effort was and still is taxing. And I am at a loss for how to be mentally stimulated without clear sight. Radio 4 has too many repeats. TV fills a gap and makes me feel I am exercising my vision back to usefulness (a bit like physiotherapy for the visual system?) without being too much of an effort. Audio on computers, again, relies on new ways of remembering. When reading I can go at my own pace, re-reading when I lose the thread or have been distracted. Listening to read-out-loud text always seems too slow and I can’t scan back to retrieve what I had not remembered as significant.
Hospital environment
Bright lights, floor to ceiling windows and pale walls are great for creating a light airy feel, but a nightmare for the visually impaired patient (VIP) or anyone who has been dilated. Maybe all hospital staff should have to spend a day dilated, wearing a high-powered contact lens and occlusion over the other eye (or a completely different strength lens) and be set a task of visiting six unfamiliar departments on different floors in different zones (instructions given by word of mouth only) and collecting a specified item/form from each department – a bit like a treasure hunt. VIPs do not only visit the eye clinics.
Appointments
Despite ophthalmologists saying I needed to be seen within a set time period (often because of the need to monitor medication or avoid being left without sufficient medication), on more than one occasion I had to contact the referral centre to ensure I had the necessary appointment booked – and then argue that my consultant had told me to do so. Inevitably, this meant I was then slotted in as an extra in the clinics list – so making the clinic overrun.
On the other hand, on one occasion I needed to cancel an appointment at very short notice, due to sickness. Despite the emphasis on letting the clinic know if an appointment could not be kept, it was not obvious how to go about doing this at very short notice. I realise this was such short notice that my slot could not be offered to another patient, but I did not wish my record to show simply that I had failed to show and risk not being able to rebook.
The future
Having been away from work for two years, I do not know if I have the confidence to return to practising as an optometrist. It would mean re-registration with the GOC, reinstated by completing two years’ worth of missed CET.
I would have to cope with the stress of working to an inflexible appointment system and balancing time spent on safe clinical assessment against the economics of ensuring a good conversion rate of sales of spectacles. On the high street, spectacles have to be sold to keep the practice financially viable and to pay for the expensive high-tech diagnostic equipment which is becoming essential for safe practice.
The days when opticians could make a comfortable living from NHS work are long gone. Unfortunately, high street opticians have to take their place in the commercial marketplace. Unless someone can come up with a model which pays them for time spent counselling VIPs it is unlikely that low vision services will be available in many high street practises. However, I do believe that optometric services should and can play a greater role in supporting VIPs
This feature is based on a blog written by the author on the Visualise website.
For more information on our Continuing Educational Training (CET) for optometrists and opticians click here.
