
Even without including the ubiquitous interest in myopia management, it is fair to say that a key area of discussion at the American Academy of Optometry event held last month was paediatric optometry. This article aims to summarise some of the more important lectures and presentations aimed at improving eye sight in children, along with some other developments that caught my eye.
Paediatrics
A key topic of discussion this year was the management of convergence insufficiency. According to one of the lectures, convergence insufficiency (CI) is ‘the most common binocular disorder with a prevalence of between 2.3% and 7.7% in the general population. As well as the more familiar problems of asthenopia with near work, something known to have impact upon a child’s educational progress, CI has also been found to influence the likelihood of a whole host of other diagnoses. Take attention deficit and hyperactivity disorder (ADHD), for example. ADHD has been found to have three times the incidence among patients with CI, and, conversely, there is three times the incidence of CI in the ADHD population.
Stark as some of these statistics might be, CI can be managed to a point where it is no longer a concern. Readers will be familiar with the various exercise, refractive/accommodative and prismatic approaches that may achieve resolution as required, and with good patient compliance, CI need not be a long-term problem. Indeed, back in 2008, a study by the CITT Study Group had shown how ‘75% of patients achieved normalisation of or improvement in symptoms and signs within a 12-week period.’ Since then, evidence has accumulated to suggest that, of the various approaches to management, a programme of regular practice attendance for planned, supervised treatments appears to be most successful (figure 1). This is described in the US as office-based vergence/accommodative therapy, or OBVAT, and should be considered the first-line treatment approach for the treatment of symptomatic CI in children nine to 17 years old. It has also been found that a majority of children who were asymptomatic after 12 weeks of OBVAT maintained their improvements in symptoms and signs for at least a year after discontinuing treatment.
A research group led by Professor Tara Alvarez has been looking at objective indicators of the impact of OBVAT and announced important results at the conference. The Convergence Insufficiency Neuro-Mechanism in Adult Population Study, or CINAP, has looked at the effect of 12 sessions of OBVAT using functional MRI scans and objective disparity eye movements along with analysis of more familiar clinical signs upon a group of young adults with symptomatic CI. The objective data clearly show ‘significant changes in clinical signs and symptoms, disparity vergence responses, and functional activity within the vergence neural circuit after 12 hours of OBVAT in young adults with symptomatic CI. Understanding the underlying neural basis of vision therapy has the potential to lead to personalised and more effective therapeutic interventions to improve binocular coordination in CI patients.’
A team from Berkeley University has looked at the use of the latest video techniques for treating amblyopia in children and found stereoscopic 3D video game play boosts stereoacuity, but not contrast sensitivity. These findings indicate that the neural alterations for enhanced depth perception might have occurred beyond the early stage of visual processing for contrast perception. The team announced, ‘our most recent experiments have shown that these types of video games might have a special benefit for triggering the plasticity of stereo vision in patients with amblyopia.’
In the UK, screening for amblyopia can be hit-or-miss, with many authorities still clinging to the idea that unilateral amblyopia is not necessarily a significant problem to detect. A team from Canada has looked at the inclusion of amblyopia detection into the general health screening programme and found that such an approach was not only successful but also cost-effective.
Yet another paediatric study of interest has been looking at the use of anti-VEGF treatment for retinopathy of prematurity (ROP). Such treatment has obvious value in reducing vascular proliferation in the eye, but presents significant risks to the overall cardiovascular health of the neonate. A team led by Professor Susan Cotter has previously reported that very low doses (as low as 0.031mg) of bevacizumab were effective in treating type 1 ROP. Their latest results show the two-year results which give strong evidence that improvements in ocular health with treatment are still present as the child grows. Ocular findings at two years were similar to those reported in infants treated with higher doses of bevacizumab, including a low incidence of high myopia.
Finally, a presentation looking at the negative impact of screen use in young children caused much interest. For years now in the US, the general advice from paediatricians has been to ‘urge parents to avoid TV for children under two years’. For each 30 minute increase in handheld screen time, researchers have found a 49% increased risk of expressive speech delay, but no apparent link between handheld device screen time and other developmental delays, such as social interactions, body language or gestures. Another study of two-year-olds has found that their body mass index (BMI) increased for every hour per week of media consumed.
Dry Eye
The DEWS II diagnostic report recommends assessment using the non-invasive measures of interferometry and tear meniscus height (TMH) in the sub-typing of dry eye. A team from California has looked at the test efficacy of these two parameters in overall dry eye diagnosis and in the identification of the two major dry eye subtypes.
They conclude that ‘these two clinical non-invasive assessments are not helpful in dry eye diagnosis or subtype differentiation. Higher precision instrument-based TMH such as with the Oculus Keratograph 5M and lipid layer thickness with LipiView may be necessary to improve dry eye subtype differentiation.’
The CORE team from Waterloo University had some nice results concerning the use of omega-3 supplementation in dry eye disease management. Their study of a group of patients who were predominantly in the severe DED category by OSDI classification found clinically meaningful improvements in their dry eye symptoms with supplementation with fatty acids. Also, ‘the addition of the omega-6 GLA in the formulation may have contributed to the significant improvement in dry eye symptoms.’
Technology
There was some interesting new research in OCT use. Dr Chris Clark and his team have been looking at whether it is possible to use machine learning to correlate changes in HbA1c levels in diabetics with changes in retinal structure that are not detectable through current means such as traditional OCT and fundus photography.
Clark’s team have determined that the ‘fine k-nearest neighbours algorithm (KNN) model’ was the best at differentiating SD-OCT images by HbA1c at the time of a patient’s screening visit. The fine KNN model could detect unique structural changes in the SD-OCT image regardless of the HbA1c level, even at HbA1c levels of six. Clark hopes that using the model could potentially reduce unnecessary visits for diabetics with otherwise healthy retinas and detect systemic diabetes in patients currently not diagnosed with diabetes.
Another study of interest has been looking at how OCT-measured parameters can change throughout the day. Dr Laura Pardon (figure 2) and her group began a presentation of their research by emphasising how ‘OCT has enhanced clinical management of optic neuropathies through its ability to provide high-resolution quantification of optic nerve head (ONH) and peripapillary structures. While retinal nerve fibre layer (RNFL) thickness has been well-established as a repeatable measure, other parameters have been suggested to exhibit diurnal fluctuations; repeatability for these parameters would therefore be expected to vary based on the relative time of day at which subsequent scans are acquired.’
 Figure 2: Dr Laura Pardon presents results on OCT measurement.
Figure 2: Dr Laura Pardon presents results on OCT measurement.
Radial scans have long been used to generate values for the ONH minimum rim width (MRW) and Bruch’s membrane opening (BMO) height (figure 3). This new study shows that MRW is decreased at 7pm relative to 7am, and the repeatability of MRW is influenced by the time of day at which repeat scans are obtained. While MRW has been shown to be a sensitive measure for detecting optic neuropathies, these results suggest that MRW measures should be obtained at the same time of day in a clinical setting in order to optimise repeatability. Perhaps we should get used to noting timings with OCT measurements in the same way we do for tonometry?
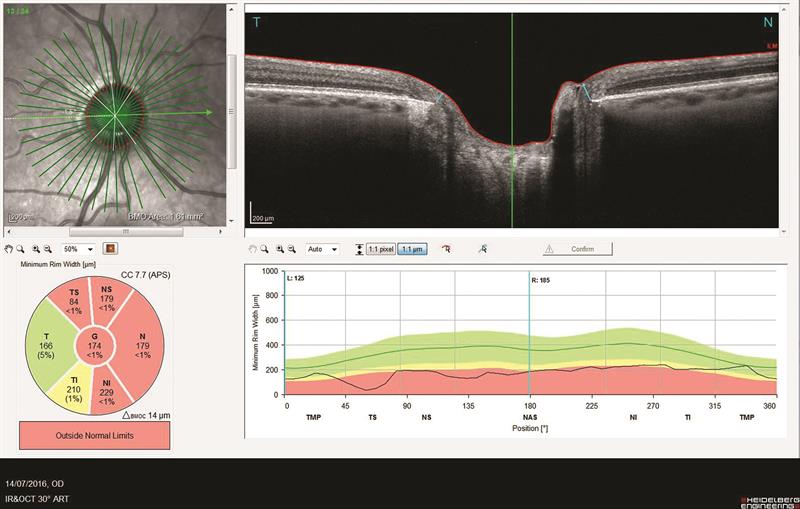 Figure 3: MRW has been shown to be a sensitive measure for detecting optic neuropathies but changes throughout the day.
Figure 3: MRW has been shown to be a sensitive measure for detecting optic neuropathies but changes throughout the day.
At present, there is no FDA approved treatment for adenoviral conjunctivitis. Dr Tammy Than reported the results of the Reducing Adenoviral Patient-Infected Days (RAPID) study, a double-masked randomised pilot trial of 5% povidone-iodine (PVP-I) for treatment of adenoviral conjunctivitis. It seems patients receiving a one time, in-office application of 5% PVP-I showed improvement in signs and symptoms, lower viral titres, and lower inflammatory indicator levels at day four compared to participants who received just artificial tears.’
