The prevalence of myopia is increasing at an unprecedented rate worldwide with current estimates at 23% of the world’s population and a predicted increase to almost 50% by 2050.1 In the United Kingdom (UK) nearly one in five teenagers is myopic,2 and faster progression has been reported to occur in pre-teens.2-4 The debilitating consequences of myopia-associated pathology help to explain why it is not surprising that eye care professionals (ECPs) in the UK and around the world have become increasingly concerned for their young myopic patients, and are keen to discuss treatment options with their patients’ parents.5
Myopia Control with Contact Lenses
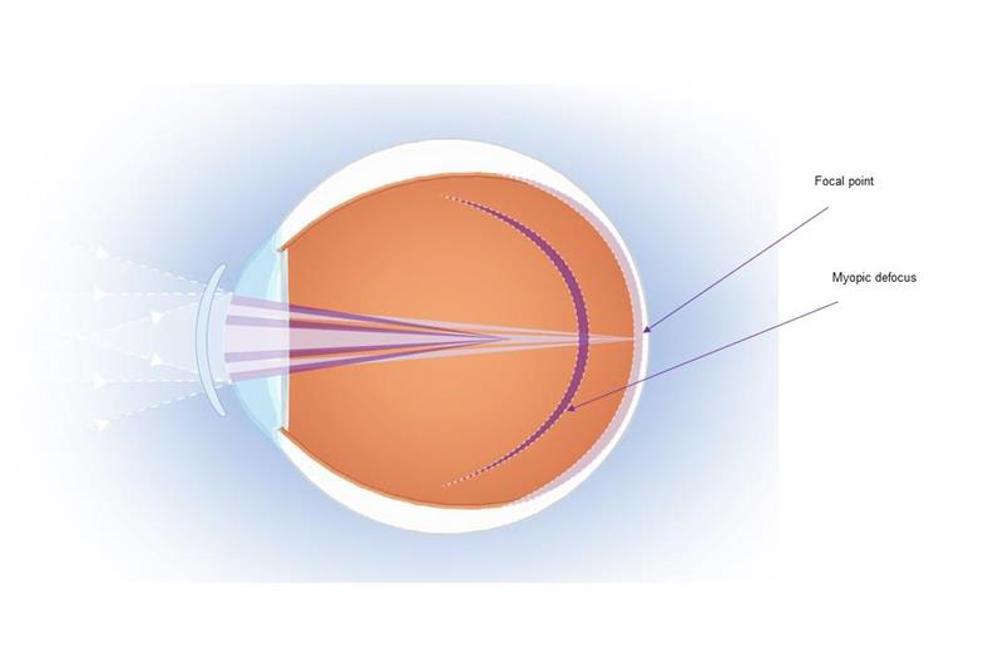
In recent times, there have been many studies aimed at reducing myopia progression with optical methods such as progressive addition lenses, overnight corneal reshaping contact lenses (orthokeratology) and soft contact lenses incorporating multifocal or aspheric optics.6-18 With respect to mechanisms that regulate refractive error development, hyperopic defocus has been shown to encourage eyeball growth; a consequence of which is increasing axial length and myopia28 that ultimately may result in regular prescription changes. In contrast, myopic defocus can retard eye growth.20 There are a number of studies that have shown that use of simultaneous optics can control axial elongation and myopia.21-27
These simultaneous optics are typically concentric alternating powers of distance correction and myopic defocus, often called ‘dual-focus’ optics. These optics have been investigated in contact lenses; in clinical practice, dual focus lenses are designed to either minimise hyperopic defocus, or to induce myopic defocus, while also allowing simultaneous correction of the child’s current refractive error, which may help to control the progression of myopia (figure 1). A study by Anstice and Phillips9 evaluated dual-focus soft contact lenses in children aged 11 to 14 years. This study reported that following 10 months, the change in spherical equivalent refraction (SE) and axial length (AL) in the eye wearing the dual focus lens was significantly less than that in the contralateral eye wearing the single-vision lens (SE: -0.44 vs. -0.69 D; AL: 0.11 vs. 0.22mm).
MiSight 1 day Myopia Management Contact Lenses
MiSight 1 day contact lenses (CooperVision, Inc) were introduced to the UK from February 2017 and are manufactured using the omafilcon A material and implement a dual focus design. Four alternate rings of power are used to correct existing myopia, and to create myopic defocus over the entire retina. MiSight 1 day has a central distance correction zone for clear vision with a concentric treatment zone introducing myopic defocus. A further distance and treatment ring completes the design (figure 2).9
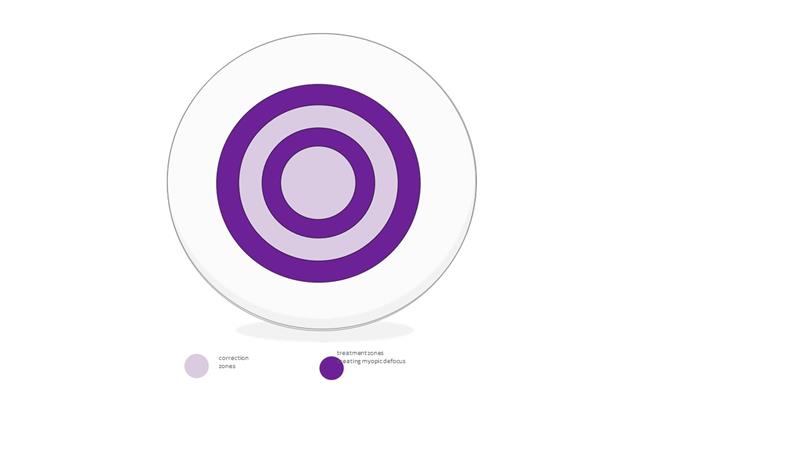
Figure 2: MiSight 1 day Lens Design
Slowing the progression of childhood myopia with MiSight 1 day
The results of a randomised, three-year clinical study into the effectiveness of MiSight 1 day have been presented in recent years at key global clinical conferences and have recently been published in Optometry and Vision Science.28 This article summarises the key findings from the research.
MiSight 1 day: Study outline
The study enrolled 144 children who were randomly assigned to either the control group or the treatment group. The treatment group wore MiSight 1 day (n=70,) and the control group wore Proclear 1 day (n=74), these interventions were identical in all respects apart from optical design (table 1).
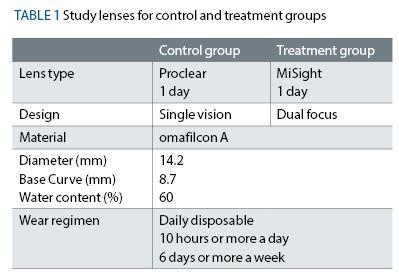
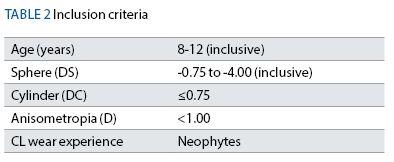
To help ensure the children recruited to the study were ethnically diverse, four clinical research sites located in the United Kingdom, Canada, Portugal and Singapore were chosen. Myopic children with no prior contact lens experience were recruited with specific inclusion criteria (table 2).
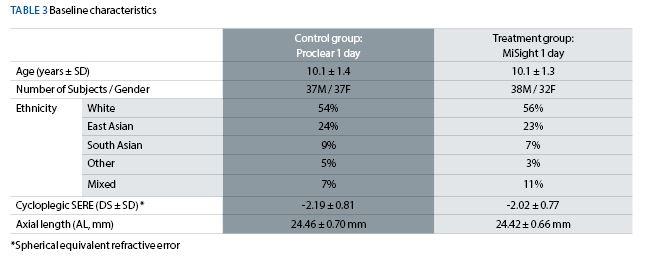
The investigators, children and parents were unaware of which group they had been assigned to for the duration of the study due to a rigorous randomisation and masking procedure. Further, both groups were recruited to be extremely well matched with no significant differences between the groups for all factors considered to be important in myopia control (table 3).
The children were instructed to wear the assigned contact lenses on a daily disposable basis for a minimum of 10 hours per day, at least six days per week, for the duration of the study. Follow-up visits were scheduled after one week and one, six, 12, 18, 24, 30 and 36 months.
A total of 109 children completed the clinical trial (53 wearing MiSight 1 day, 56 wearing Proclear 1 day) which represents an extremely high retention rate for a study of this nature and duration.
Key findings:
Refractive error and axial length
Cycloplegic refractive error (converted to spherical equivalent refractive error, or SERE) and axial length (AL) were measured at baseline, 12-month, 24-month and 36-month visits.28 Open-field autorefraction was conducted with a Grand Seiko autorefractor and AL was measured using an IOL Master. The results for the change in SERE and AL for the MiSight 1 day and Proclear 1 day groups are shown graphically in figures 3 and 4 respectively.
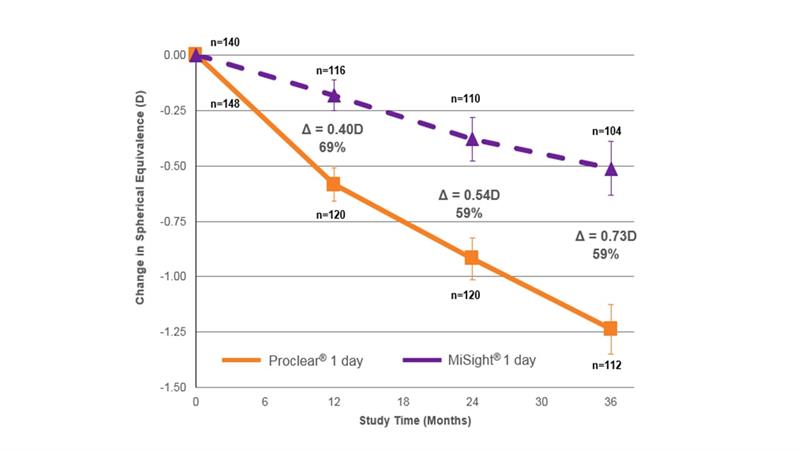 Figure 3: Mean change in spherical equivalent refractive error from baseline showing that MiSight 1 day reduced the rate of myopia progression by 59% over a three-year period. All available eyes28
Figure 3: Mean change in spherical equivalent refractive error from baseline showing that MiSight 1 day reduced the rate of myopia progression by 59% over a three-year period. All available eyes28
As is typical in studies of this nature, a linear mixed model was applied to account for study group imbalances that could possibly affect the primary outcome measures, for example age, gender and site location. However, the results of the linear mixed model analysis did not significantly change the primary outcome results, as such, we only present the unadjusted data in this article.
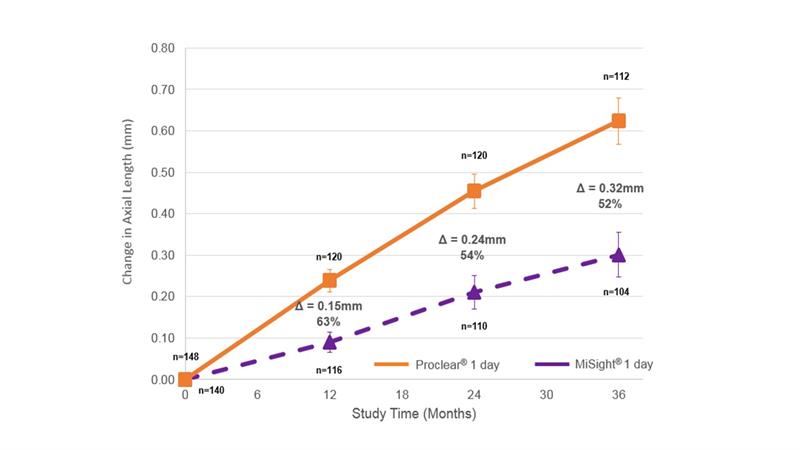 Figure 4: Mean change in axial length from baseline showing that MiSight 1 day wearers had 52% less axial growth over a three-year period. All available eyes28
Figure 4: Mean change in axial length from baseline showing that MiSight 1 day wearers had 52% less axial growth over a three-year period. All available eyes28
The distribution of individual eye responses for the change in SERE after 36 months for both the MiSight 1 day and Proclear 1 day groups are presented in figure 5. These results show that 41% of the eyes in the children wearing the MiSight 1 day showed no myopia progression (≤ 0.25D SERE change) as compared with only 4% of the eyes in the children wearing the Proclear 1 day lens. In contrast, 62% of the eyes of the children wearing the Proclear 1 day lens had progressed by more than -1.00D as compared with only 18% of the eyes in the children wearing MiSight 1 day. In practice, with a similar population of children wearing MiSight 1 day, a significant proportion could see their myopia progression halted although managing expectations with parents and children in practice will need a careful approach.
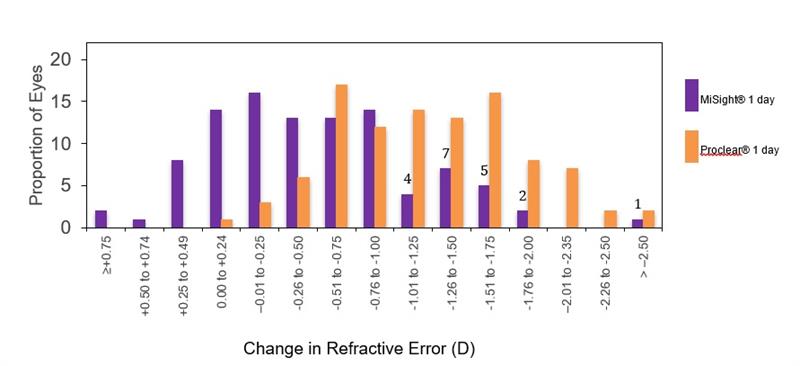 Figure 5: Frequency of eyes by change in refractive error at three years28
Figure 5: Frequency of eyes by change in refractive error at three years28
By one month, over 80% of the children from both the test and control groups described contact lens application as ‘kind of easy’ or ‘really easy’. Similarly, more than 90% of children reported that contact lens removal was ‘kind of easy’ or ‘really easy’ for all study visits. This demonstrates that children from the age of eight are able to confidently handle their contact lenses soon after the initial fitting.
Presenting visual acuity with contact lenses varied slightly at follow-up visits as can be seen in figure 6. However, with spherical over-refraction, best-corrected visual acuity with contact lenses remained similar for the two lens types and better than 6/6 for each follow-up visit. Questionnaire responses correlated with these findings with over 90% of children agreeing that MiSight 1 day gave them clear vision at a variety of distances during everyday activities including playing outdoors, schoolwork, reading and watching television with nine out of 10 children preferring their MiSight 1 day lenses to wearing their spectacles.
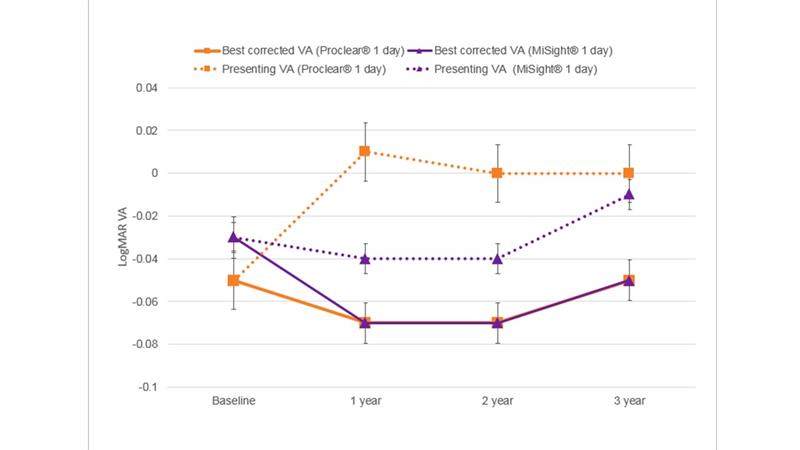 Figure 6: Comparison of presenting VA with MiSight 1 day, Proclear 1 day and best-corrected VA with spherical over-refraction.28
Figure 6: Comparison of presenting VA with MiSight 1 day, Proclear 1 day and best-corrected VA with spherical over-refraction.28
The key findings of this carefully designed and controlled three-year clinical study clearly demonstrate that MiSight 1 day contact lenses were effective in significantly reducing both the progression of myopia and the associated increase in axial length over the 36-month study period. It is reassuring that the controlling effects on both the refractive error progression and the axial length elongation persisted throughout the study period.
A reduction in the natural progression of myopia during childhood and adolescence will result in a lesser degree of myopia after stabilisation, with associated ocular health and quality of life benefits.29,30 It is important to remember that in addition to myopia management benefits, contact lens wear in children and teens has been reported to offer advantages in social settings, for sport and to improve self-esteem, when compared with spectacle wear.31-33
These findings were supported in this study with nine out of 10 children expressing a preference for contact lenses compared to their spectacles.
The children taking part in the study were generally able to handle their contact lenses independently of their parents, consistent with reports from other studies.34,35 This supports the findings of a recently conducted survey in which ECPs worldwide would consider fitting children from 8.8 years of age with myopia management contact lenses with ECPs across Europe considering fitting children from 7.3 years of age.5
No serious or significant ocular complications were reported during the three-year study period. This supports current evidence that soft contact lens wear in children carries similar low-level risk as contact lens wear in teenagers and adults.36,37
The MiSight 1 day clinical study is now in its sixth year – the longest continuous contact lens study to date. All the children wearing Proclear 1 day (control) have been moved to MiSight 1 day to help understand the impact of MiSight 1 day in an older population of children. The children in both groups showed similar rates of progression through years four and five in both refractive error and axial length growth.38
The five year results from the MiSight 1 day clinical study were presented at BCLA in June 2019, where the CooperVision team were presented with the prestigious BCLA Industry Award in recognition of the commitment to develop, research and produce MiSight1 day to address the developing epidemic of myopia.
Conclusions
Being a daily disposable lens, MiSight 1 day can offer well documented advantages over reusable lenses39,40 and are widely considered to be an ideal option for children and teens. With MiSight 1 day, ECPs now have the option of prescribing an easy to fit contact lens to help manage myopia progression in their young patients. Intervention at an early age, when the amount of myopia is low, should be discussed with all parents.
Paul Chamberlain is Director of Myopia Research within the Research and Development department at CooperVision Inc where Elizabeth Lumb is EMEA Head of Professional Services, MiSight 1 day. Kathy Dumbleton is a clinical research scientist based in the US.
Acknowledgement
Thanks to Visioncare Research Ltd as the Clinical Research Organisation for this study.
This clinical trial was funded by CooperVision Inc.
References
1 Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 2016;123:1036-42
2 McCullough SJ, O’Donoghue L, Saunders KJ. Six Year Refractive Change among White Children and Young Adults: Evidence for Significant Increase in Myopia among White UK Children. PLoS One. 2016;11:e0146332
3 Dong L, Fazzari M, Gwiazda J, Comet. Myopia stabilization and associated factors among participants in the Correction of Myopia Evaluation Trial (COMET). Invest Ophthalmol Vis Sci. 2013;54:7871-84
4 Donovan L, Sankaridurg P, Ho A, Naduvilath T, Smith EL, 3rd, Holden BA. Myopia progression rates in urban children wearing single-vision spectacles. Optom Vis Sci. 2012;89:27-32
5 Wolffsohn JS, Calossi A, Cho P, Gifford K, Jones L, Li M, et al. Global trends in myopia management attitudes and strategies in clinical practice. Cont Lens Anterior Eye. 2016;39:106-16
6 Cho P, Cheung SW. Retardation of Myopia in Orthokeratology (Romio) Study: A 2 year Randomized Clinical Trial. Invest Ophthalmol Vis Sci. 2012;53:7077–85.
7 Cho P, Cheung SW, Edwards M. The Longitudinal Orthokeratology Research in Children (Loric) in Hong Kong: A Pilot Study on Refractive Changes and Myopic Control. Curr Eye Res 2005;30:71–80
8 Walline JJ, Jones LA, Sinnott LT. Corneal Reshaping and Myopia Progression. Br J Ophthalmol 2009;93:1181–5
9 Anstice NS, Phillips JR. Effect of Dual-focus Soft Contact Lens Wear on Axial Myopia Progression in Children. Ophthalmology 2011;118:1152–61
10 Sankaridurg P, Holden B, Smith E, 3rd, et al. Decrease in Rate of Myopia Progression with a Contact Lens Designed to Reduce Relative Peripheral Hyperopia: One-year Results. Invest Ophthalmol Vis Sci. 2011; 52:9362–7
11 Walline JJ, Greiner KL, McVey ME, et al. Multifocal Contact Lens Myopia Control. Optom Vis Sci. 2013;90: 1207–14
12 Fujikado T, Ninomiya S, Kobayashi T, et al. Effect of Low-addition Soft Contact Lenses with Decentered Optical Design on Myopia Progression in Children: A Pilot Study. Clin Ophthalmol. 2014;8:1947–56
13 Lam CS, TangWC, Tse DY, et al. Defocus Incorporated Soft Contact (Disc) Lens Slows Myopia Progression in Hong Kong Chinese Schoolchildren: A 2-year Randomised Clinical Trial. Br J Ophthalmol 2014;98:40–5
14 Paune J, Morales H, Armengol J, et al. Myopia Control with a Novel Peripheral Gradient Soft Lens and Orthokeratology: A 2-year Clinical Trial. Biomed Res Int 2015;2015:507572
15 Aller TA, Liu M, Wildsoet CF. Myopia Control with Bifocal Contact Lenses: A Randomized Clinical Trial. Optom Vis Sci 2016;93:344–52
16 Cheng X, Xu J, Chehab K, et al. Soft Contact Lenses with Positive Spherical Aberration for Myopia Control. Optom Vis Sci 2016;93:353–66
17 Ruiz-Pomeda A, Perez-Sanchez B, Valls I, et al. MiSight Assessment Study Spain (MASS). A 2-Year Randomized Clinical Trial. Graefes Arch Clin Exp Ophthalmol 2018;256:1011–21
18 Allen PM, Radhakrishnan H, Price H, et al. A Randomised Clinical Trial to Assess the Effect of a Dual Treatment on Myopia Progression: The Cambridge Anti-Myopia Study. Ophthalmic Physiol Opt 2013; 33:267-76
20 Smith EL, 3rd. Prentice Award Lecture 2010: A case for peripheral optical treatment strategies for myopia. Optom Vis Sci. 2011;88:1029-44
20 Smith EL, 3rd, Hung LF, Arumugam B. Visual Regulation of Refractive Development: Insights from Animal Studies. Eye (Lond) 2014;28:180-8
22 Liu Y, Wildsoet C. The Effect of Two-zone Concentric Bifocal Spectacle Lenses on Refractive Error Development and Eye Growth in Young Chicks. Invest Ophthalmol Vis Sci 2011;52:1078-86
23 Liu Y, Wildsoet C. The Effective Add Inherent in 2-zone Negative Lenses Inhibits Eye Growth in Myopic Young Chicks. Invest Ophthalmol Vis Sci. 2012;53: 5085–93
24 Arumugam B, Hung LF, To CH, et al. The Effects of Simultaneous Dual Focus Lenses on Refractive Development in Infant Monkeys. Invest Ophthalmol Vis Sci 2014;55:7423–32
25 Benavente-Perez A, Nour A, Troilo D. The Effect of Simultaneous Negative and Positive Defocus on Eye Growth and Development of Refractive State in Marmosets. Invest Ophthalmol Vis Sci 2012;53:6479-87
26 Arumugam B, Hung LF, To CH, et al. The Effects of the Relative Strength of Simultaneous Competing Defocus Signals on Emmetropization in Infant Rhesus Monkeys. Invest Ophthalmol Vis Sci 2016;57: 3949-60
27 Tse DY, Lam CS, Guggenheim JA, et al. Simultaneous Defocus Integration During Refractive Development. Invest Ophthalmol Vis Sci 2007;48: 5352-9
28 Chamberlain, P et al. A 3-year Randomized Clinical Trial of MiSight Lenses for Myopia Control. Optometry and Vision Science. 2019; 96(8): 556-567
29 Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012;31:622-60
• For full references see online at opticianonlline.net.
30 Rose K, Harper R, Tromans C, Waterman C, Goldberg D, Haggerty C, et al. Quality of life in myopia. Br J Ophthalmol. 2000;84:1031-4
31 Dias L, Manny RE, Weissberg E, Fern KD. Myopia, contact lens use and self-esteem. Ophthalmic Physiol Opt. 2013;33:573-80
32 Walline JJ, Gaume A, Jones LA, Rah MJ, Manny RE, Berntsen DA, et al. Benefits of contact lens wear for children and teens. Eye Contact Lens. 2007;33:317-21
33 Walline JJ, Jones LA, Sinnott L, Chitkara M, Coffey B, Jackson JM, et al. Randomized trial of the effect of contact lens wear on self-perception in children. Optom Vis Sci. 2009;86:222-32
34 Walline JJ, Long S, Zadnik K. Daily disposable contact lens wear in myopic children. Optom Vis Sci. 2004;81:255-9
35 Walline JJ, Lorenz KO, Nichols JJ. Long-term contact lens wear of children and teens. Eye Contact Lens. 2013;39:283-9
36 Bullimore MA. The Safety of Soft Contact Lenses in Children. Optom Vis Sci. 2017;94:638-46
37 Chalmers RL, Wagner H, Mitchell GL, Lam DY, Kinoshita BT, Jansen ME, et al. Age and other risk factors for corneal infiltrative and inflammatory events in young soft contact lens wearers from the Contact Lens Assessment in Youth (CLAY) study. Invest Ophthalmol Vis Sci. 2011;52:6690-6
38 Chamberlain P. et al. Further comparison of myopia progression in new and established myopia control treatment (MiSight groups). BCLA Clinical Conference 2019
39 Cho P, Boost M. Daily disposable lenses: the better alternative. Contact Lens Anterior Eye. 2013;36:4-12
40 Chalmers RL, Hickson-Curran SB, Keay L, Gleason WJ, Albright R. Rates of adverse events with hydrogel and silicone hydrogel daily disposable lenses in a large postmarket surveillance registry: the TEMPO Registry. Invest Ophthalmol Vis Sci. 2015;56:654-63
