The annual Glaucoma Symposium organised by Haag-Streit UK has become an established event on the optometry education calendar, and this year included speakers outlining the latest in assessment and treatment.
Perimetry
Visual fields assessment is still an integral part of the assessment of anyone at risk of glaucoma, or for monitoring the progression of glaucomatous disease. In his overview of perimetry, Professor Paul Artes (Plymouth University) reminded the audience of the great strides made in the evolution of visual fields screeners (figure 1).
Modern instruments, such as the latest Octopus, include an array of strategies, offer data helpful in predicting glaucomatous change, show reliability and help adapt fixation, and include an extensive database – helpful in deciding whether results fall outside the expected. That said, the assessment is a subjective one and always at the mercy of patient responses. Artes reminded delegates that it is always worth considering specificity and sensitivity when deciding on appropriate strategies.
A suprathreshold strategy, where stimuli should be easy to see, might not be so sensitive as to detect the very earliest scotomas or hemifield asymmetry, but is still worth considering for an unreliable patient and better than no fields assessment at all. ‘Consider suprathreshold perimetry,’ stated Artes, ‘for inexperienced patients, when fields screening is repeated periodically and when specificity is paramount.’
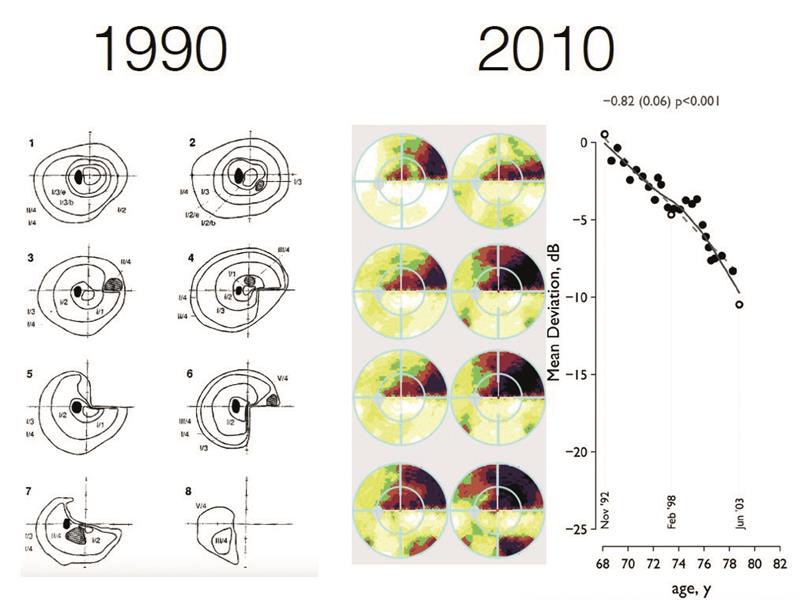
Figure 1: Modern perimetry has evolved from kinetic data to static data analysis
OCT angiography
An update on the exciting new technique of OCT angiography (OCT-A) was presented by consultant ophthalmologist Andrew Tatham (University of Edinburgh). The non-invasive technique that detects changes in blood flow is already established in the management of vascular diseases such as wet AMD or vein occlusions technique (figure 2).
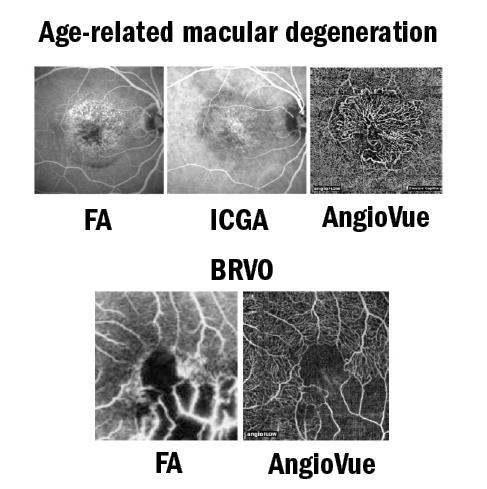
Figure 2: OCT-A usefully complements invasive techniques such as fluorescein angiography (FA) and indocyanine green (ICG) assessment of vascular conditions such as wet AMD and vein occlusion
But what about glaucoma? After a useful discussion of the anatomy of the blood supply to and within the eye, Tatham discussed the latest quantification of the ocular vasculature that is possible with instruments such as the AngioVue. Vessel density represents the percentage of area occupied by vessels, while flow index represents fluctuations in the OCT-A signal that indicates changes in blood flow.
There is increasing evidence that glaucoma is associated with altered ocular blood perfusion as measured by OCT-A, often well in advance of repeatable field loss. OCT-A measurements of vessel density are good at detecting glaucoma, but not as good as conventional structural measurements (such as RNFL thinning). The radial peripapillary capillary network appears the best for aiding any initial diagnosis.
Remember your slit lamp
After the high-tech presentations, nurse practitioner Rebecca Turner (Oxford Eye Hospital) reminded everyone of the importance of good slit lamp technique in glaucoma assessment. Indeed, three of the five diagnostic criteria are achievable with a slit lamp. Turner went as far as describing the slit lamp as ‘the Gucci handbag of glaucoma’. Along with visual fields and pachymetry, the slit lamp is essential for:
- Stereoscopic viewing of the optic nerve head
- Goldmann tonometry
- Gonioscopy and van Herick assessment of the angle and chamber depth
She then described each of these in some detail.
