The historical classification of dry eye disease (DED) has typically considered two distinct disease entities:
- Aqueous deficient
- Evaporative
The latest thinking from the tear film and ocular surface society (TFOS) DEWs II report suggests moving away from this separation and more towards a blurring of the lines between the two classically considered sub-types. In other words, we should consider the disease as more of a continuum of these two sub-types rather than separate entities.
The latest classification scheme encourages a simplified diagnostic strategy to help triage patients (figure 1). The scheme also importantly considers the cases where patients exhibit dry eye symptoms without evidence of obvious signs or, at the opposite end of the spectrum, present with marked signs but have no dry eye symptoms. It also includes a clinical decision guide for practitioners. The classification also recognises the necessity of symptomatic involvement and the need for presence of associated ocular surface signs in making an actual diagnosis of DED. In this series of case studies, I aim to focus on these cases with different levels of influence of each sub-type and show how management differed.
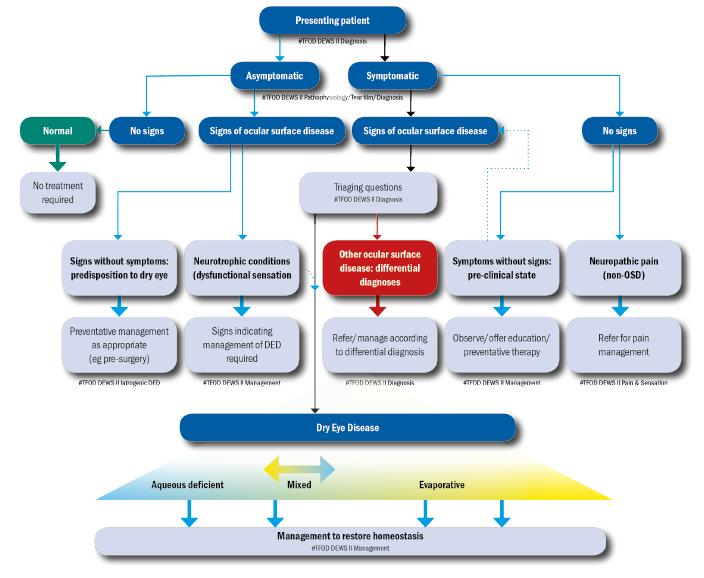
Figure 1: The DEWS II classification of dry eye disease. The upper part of the diagram represents a clinical triage guide, including assessing symptoms, followed by reviewing signs of ocular surface disease. DED exhibits both symptoms and signs and can be treated with appropriate strategies. Symptomatic patients without signs do not fall into the DED group. Asymptomatic patients with signs of DED are then separated into patients with poor corneal sensitivity or those with prodromal signs at risk of developing DED with time or a trigger such as surgery
The lower portion shows the categories of dry eye, now considered as more of a blend or hybrid of the two traditional categories of aqueous deficient (affecting lacrimal gland function) or evaporative (lid related and ocular surface related). More of this sliding scale is devoted to evaporative to reflect the greater proportion of DED attributable to this category. It is acknowledged that, as the disease progresses, it is more likely that both components will become apparent clinically.
Case 1
Visit 1
January 2018
Presentation
Background: KB, female, age 53, office manager role.
KB first attended as a new patient to my dedicated dry eye clinic just over a year ago. She had been told by her previous optometrist that she had dry eye and that was the cause of her contact lens discomfort. She was using Blephaclean wipes infrequently and Hycosan drops twice a day for the past two months. Despite this, she was still suffering significantly enough to seek further help. Her symptoms at presentation were significant bilateral gritty irritation especially in the evening and occasional watery eyes outdoors. She also reported increasing awareness of redness around the eyes.
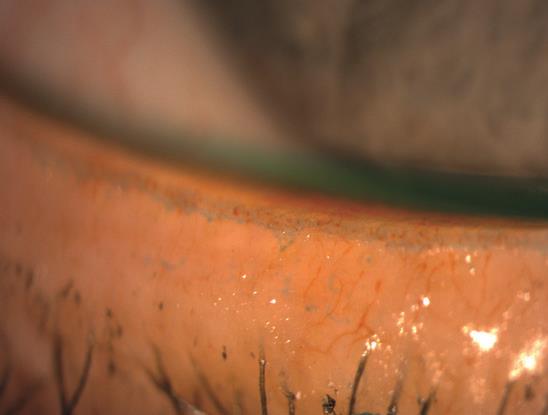
Figure 2
She was wearing monthly replacement PureVision multifocal contact lenses (B&L), and complained of end of day discomfort. She had recently ceased wear due to intolerance of the poor comfort.
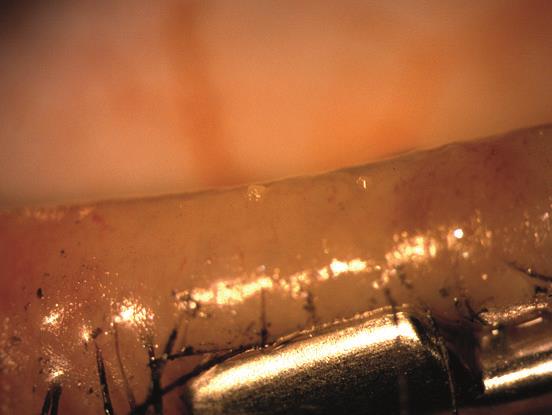
Figure 3
Relevant History; recent bad allergic reaction to eyelash extensions, removed.
Clinical Findings; (author throughout uses grading based on a modified Efron grading principle; 0 = normal, 4 = severe):
- DEQ-5 score; 14
- Acuity; R 6/6, L 6/6
- Osmolarity (TearLab); R332, L328 mOsm/L
- Eyelid aspects:
- Lid closure analysis; normal
- No incomplete blinks observed LWE; grade 1 showing some irregularity and increased width of staining band along lid wiper portion of lid (figure 2)
- Meibomian gland functionality (see figure 3 for baseline appearance)
- Expressability; grade 2 on expression, with a significant number of glands failing to express on pressure with MG forceps, (as can be seen in figure 3)
- Secretion viscosity grade variable, with most grade 3 lower lids and grades 2 or 3 upper lids. R and L eyes similar
- Multiple gland notching visible lower lid margins (figure 4) indicating gland atrophy, scarring and shrinking underneath the gland orifice, each a likely sign of a chronic disease processes
- Significant telangiectasia of vessels noted on all inner lid margins (see figure 5) tending to be a sign of chronic duration of MGD and inflammation
- Posterior migration of gland orifices observed in (see figure 6; note the row of gland orifices clearly showing posterior migration of the gland orifice)
- Blepharitis; grade 0
- Conjunctival hyperaemia grade 1 (see figure 7)
- Minimally elevated pinguecula
- Meibography grade 3 R grade 2 L indicating moderate gland drop out and shortening of overall length (see infrared figure 8 for lower lid and figure 9 for upper lid)
- Meniscometry; tear prism height 0.2mm, indicating normal volume levels (see figure 10 – the meniscus is highlighted for ease of visualisation with fluorescein)
- Fluorescein TBUT; R 4, L 5 seconds
- Ocular surface staining with fluorescein; corneal superficial punctate epithelial erosion (SPEE), grade 2.
- Ocular surface staining with lissamine green; small patch of staining over the pinguecula (see figure 11)
- LIPCOF: grade 0
Diagnosis
My conclusions drawn from the clinical assessment was a working diagnosis of a longstanding evaporative dry eye disease state with meibomian gland drop out.
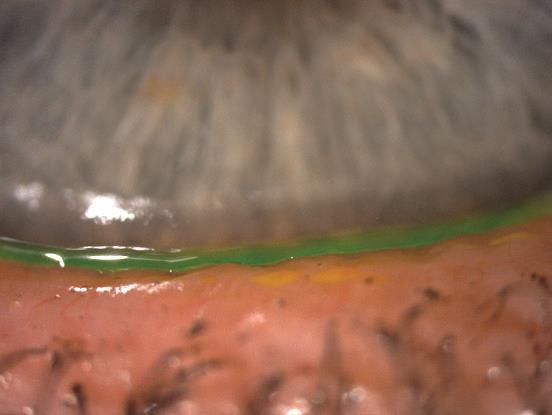
Figure 4
Management plan
My proposed management plan was divided into the in-practice component and the at-home plan.
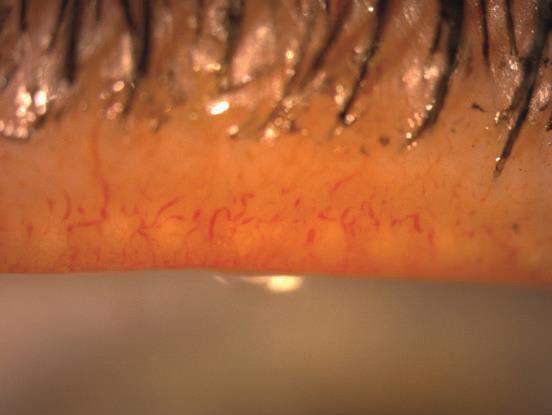
Figure 5
In-practice plan:
1 All four lids had complete expression using meibomian gland forceps (from specialisedophthalmicservices.com)
2 All four lid margins debrided using golf club spud
3 Educated and explained full diagnosis and management plan to patient
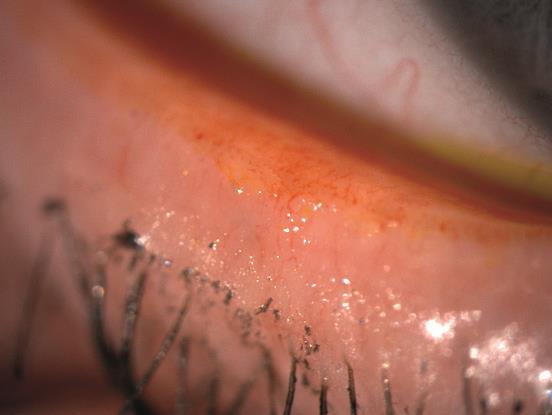
Figure 6
Management plan at home:
1 Warm compress with mask 10 minutes once a day
2 Omega-3 supplement provided
3 Carry on with preservative free drops (qds)
4 Book contact lens refit appointment.
Visit 2 and 3
Contact lens refitting March and April 2018
The patient was refitted with Proclear Monthly multifocals (was very keen to keep to a multifocal monthly lens if possible) and supplied with Puremoist solutions.

Figure 7
She returned for a contact lens follow up feeling much more comfortable and reporting her wearing time had already gone back up to 10 to 12 hours of comfortable wear.
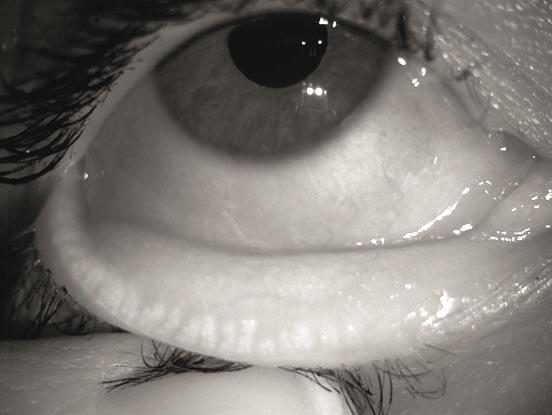
Figure 8
Visit 4
August 2018; Dry eye follow up appointment (no contact lenses worn to appointment)
Presentation
Patient presented having been generally compliant with the at-home management plan. Contact lens comfort had significantly improved since the refit and she was back to five days wear each week for up to 10 hours a day. There was still some variable end of day irritation, but this had significantly improved from baseline. She feels in control of her condition and happy with the comfort levels.

Figure 9
Clinical findings:
- DEQ-5; score 7
- VA; R 6/6, L 6/6
- Osmolarity; R 318, L 327 mOsm/L
- Meibomian gland dysfunction on expression; grade 1 (some 2) and secretion grade 1 (see figure 12).
- Lid margin telangiectasia less visible (figure 12)
- Lower lids show a much improved clinical picture of meibum viscosity compared to the baseline
- Conjunctival hyperaemia; grade 1
- Meibography; grade 1 to 2
- Grade 0 Blepharitis
- Tear prism height; 0.2mm
- Fluorescein TBUT; R 8, L 8 seconds (much improved from previous assessment)
- Corneal SPEE inferior central cornea grade 0 (again, improved)
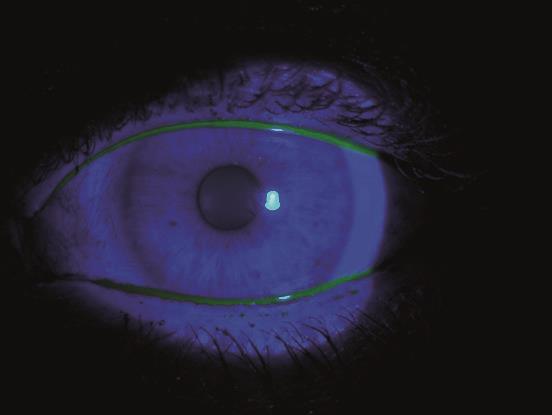
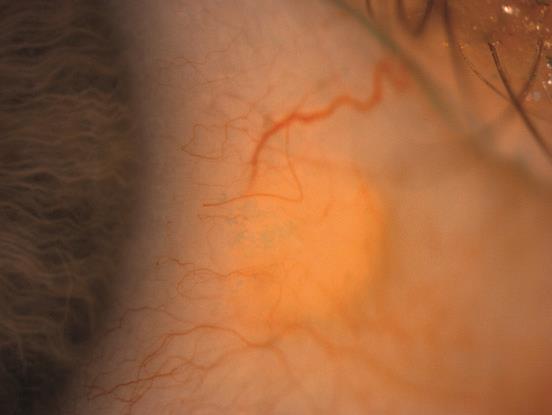
Figure 11
Interpretation
Meibum viscosity in glands was responding well to the current in-practice and at-home regime, and patient compliance was good. It was decided to continue with the same regime and review again in further six months for further maintenance.
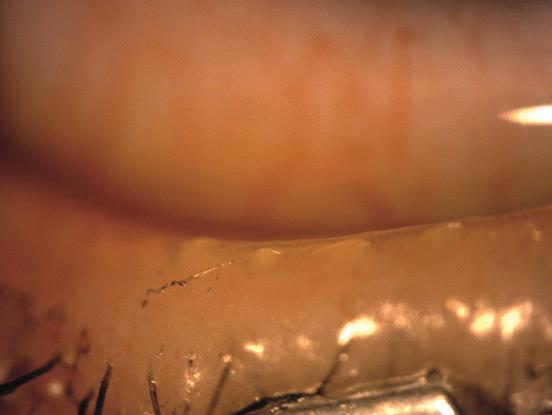
Figure 12
Conclusion
This case review gives us a simple example of what results can be achieved with a straight forward working diagnosis and targeted management plan. I have always advocated the need for a separate dedicated consultation as the only way to spend enough time on work up, active in-house treatment and effective patient education to really achieve results. I still get such satisfaction every time I am able to make a patient with dry eye disease more comfortable. The work-up, diagnosis and management of dry eye patients is a very rewarding part of the services we can offer in primary eye care.
Resource
The DEWS II report is a fantastic free resource for giving practitioners evidence based best guidance on work up, diagnosis and logical management strategies for dry eye disease.
www.tfosdewsreport.org or download the app.
Sarah Farrant is a therapeutic optometrist with a special interest in dry eye disease who works in independent practice in Somerset.
