Age-related macular degeneration (AMD) encompasses a wide spectrum of retinal changes within the central fundus which can result in a varying amount of functional impairment,1 often significantly impacting on the affected individual’s quality of life.2 In the early stages of the disease, and more commonly in the intermediate stages, sufferers can complain of a variety of difficulties with everyday tasks such as reading and face recognition.
A wide variety of functional measures of visual performance have been shown to be significantly reduced at this stage of the disease.3,4 As there is currently no medical intervention for individuals presenting with such features and symptoms of non-exudative AMD, and with a large increase in the prevalence of the number of individuals presenting with the disease over the next number of years,5 the option of non-medical interventions in the management of such patients is important.
A variety of spectacle lens types or wrap-around glasses, essentially incorporating a coloured filter, have been proposed as being of benefit to patients with AMD, with varying amounts of success being reported.6-11
Recently, a new spectacle lens has been made commercially available for the benefit of individuals suffering with AMD (and other ocular pathologies). The E-Scoop lens (Norville, Gloucester, UK) is a patented loupe spectacle lens, which is built on a number of basic optical features with the aim of enhancing vision. The lens includes the patient’s up-to-date prescription while the thickness and curve of the lens ensures a magnification of 6% for distance and near vision.
The lens is available with three levels of prism (4, 6 or 8 prism dioptres) which is intended to shift the retinal image from the fovea to a healthier part of the retina. The manufacturer recommends prescribing the prism as base-up as this will shift the image into the superior macular area and away from the more commonly affected inferior retina.
Several studies using microperimetry have shown that, in individuals with central scotoma, the majority of them will develop a preferred retinal location in the superior retina.12 Base-down prism is also available if this is subjectively better and in a standard optometry or low vision clinic there may be an element of trial and error in initially determining the appropriate direction of prism.
The lens is yellow in colour (90% light transmission factor) to provide enhanced contrast for the patient. A wide variety of theories have been put forward to try to explain why a yellow filter might enhance vision and these include reduced rod contribution to the chromatic pathway, increased pupil size providing greater retinal illumination and enhanced visibility against short wavelength backgrounds (see Wolffsohn et al, 2002). The lens also has an anti-reflection coating which will improve the light transmission of the lens and help reduce the amount of unwanted reflections and glare.
The purpose of this study is to determine if the E-Scoop lens has a significant effect on a variety of measures of visual function in individuals with non-exudative AMD and mild visual loss. The majority of the previous studies in this area have included participants with a wide range of baseline pathology and visual function, with the majority of those included having a moderate to severe reduction in vision.6-11 Therefore, we wished to know if the E-Scoop brings a significant improvement at an earlier stage in the disease where vision function is still relatively good. Importantly, we wanted to examine the effect the E-Scoop lens has on reading acuity and reading speed, two very important functional aspects of vision.
Methods
The study was conducted in a high street optometry practice in the Republic of Ireland and participants were recruited from a local private ophthalmology clinic. Twenty-two individuals (14 females, eight males) ranging in age from 58 to 80 years (mean 72.5 years) with non-exudative AMD, diagnosed by a consultant ophthalmologist, participated in the study.
Eligible individuals had any soft drusen and/or areas of hypopigmentation and/or hyperpigmentation in the retinal pigment epithelium (RPE) and/or early geographical atrophy seen on dilated fundus examination. Individuals with previous or current exudative AMD in the study eye, retinitis pigmentosa, glaucoma or diabetic retinopathy were excluded.
Individuals with a best corrected distance visual acuity (BCVA) of at least 0.48 logMAR (6/18) and a near word reading acuity of at least 0.8 logMAR (N20) were included. One eye was chosen for the study with the fellow eye occluded during testing. When individuals had bilateral AMD which both met the inclusion criteria, the eye with the worst acuity was chosen as the study eye. Six of the individuals were pseudophakic with the others having varying degrees of age-related lens yellowing including early cataract. There were no individuals where cataract would have been the primary cause of the reduction in vision.
All data was collected in the same clinical testing room by one of the authors (NM), who is an experienced optometrist. All participants had their full refraction status checked prior to the commencement of the study to ensure that each participant had their best corrected spectacle correction and all testing was carried out using the appropriate single vision distance or near prescription.
For the reading task a fluorescent lamp was place at approximately 30cm from the text to insure total illuminance of at least 1,000 lux. Ethical approval from the Research Ethics Committee at the Ulster University was obtained for the research study and all participants gave written consent to be included in the study in accordance with the tenets of the Declaration of Helsinki.
The following monocular visual function measures were taken, the fellow eye being occluded, for each participant using their habitual up-to-date refraction and with each of the three different coloured lenses using trial sets purchased from the manufacturers. The E-Scoop trial kit consists of three clip-on sets of lenses in yellow with 4 base up, 6 base up and 8 base up prism respectively.
After baseline measures with the habitual spectacles, the order of lens used was randomised between patients with distance visual acuity, contrast sensitivity and reading acuity measured on one visit and reading speed measured at a second visit, which was within three weeks of the first visit. This was done to minimise the impact of fatigue on the reading speed measures.
Distance visual acuity
Distance visual acuity was measured at a distance of 3 metres with an ETDRS illuminated chart (Clement Clarke, Harlow, UK). Four different versions of the chart were used to try to reduce any learning effects. The individual was encouraged to read down the chart as far as possible until they did not read any correct letters for a full line. Each letter read correctly up to that point was given a score of 0.02 log units.
Contrast sensitivity
Contrast sensitivity (CS) was measured at a distance of one metre with the Pelli-Robson CS chart (Clement Clarke, Harlow, UK) with a luminance of 80-120 cd/m². This corresponds to a fixed spatial frequency of 1.5 cyc/deg at this testing distance. Both versions of the chart were used to reduce the effects of learning with an additional +0.75 DS added to the participants distance prescription to correct for the shortened working distance. CS measurements were measured with each letter read correctly having a value of 0.05 log units.13
Reading acuity and maximum reading speed
Reading acuity and reading speed were measured with the MNRead Acuity Charts (Precision Vision, LaSalle, Illinois) which are continuous text reading acuity charts for measuring acuity and reading speed at different print sizes. There are four versions of the chart available and each contains 19 sentences of different print size made up of 60 characters.
This gives a print size range between 1.3 and -0.5 logMAR at the recommended viewing distance of 40cm. The participants were seated at a desk with total illuminance being provided by the ambient room light and the localised light from the cool fluorescent lamp positioned at 30cm from the MNRead near acuity chart. All participants were instructed to hold the MNRead near acuity charts at 40cm, or at a more comfortable working distance if needed.
Reading acuity and reading speed were measured using the manufacturers recommended protocol. Reading acuity was measured by getting the patient to attempt as many of the sentences as was possible with their reading correction (with and without the various clip-on lenses). Final acuity was calculated as the smallest print size read plus an additional 0.01 logMAR for every word read wrongly up to that point with a correction for a different working distance from the standard 40cm, where appropriate.
Maximum reading speed, which is defined as the best reading performance that can be attained when print size is not a limiting factor, was measured using the MNRead chart using the manufacturers guidelines. Participants were instructed to read each sentence continuously one after the other as fast as they could aloud.
The time taken to read each of the sentences was measured using a stopwatch (to 0.1 of a second) and the number of word errors for each sentence was recorded throughout. Reading speed in words per minute (wpm) was plotted against print size (logMAR) on the chart supplied by the manufacturer and maximum reading speed was recorded at the plateau of this relationship. At acuities higher than the plateau, reading speed is lower than the maximum reading speed. Reading speed for each line is calculated using the formula: Reading Speed = 60 × (10 – errors) / (time in seconds).
Data analysis
The data was stored in Microsoft Excel 2013 and inputted into Statistical Package for the Social Sciences SPSS (version 22) for statistical analysis purposes. A Shapiro-Wilk’s test (p>0.05) and a visual inspection of their histograms showed that distance logMAR acuity and reading speed were normally distributed.
For these measures a one way ANOVA statistical test, with colour filter type as the factor, was used to establish if the coloured filter had a significant effect on visual function. Differences between the lens conditions were examined with post-hoc analysis (Tukey’s test). CS values and reading acuity were not normally distributed so the effect of the filter was analysed using the Kruskal-Wallis test.
Results
Age, gender, refractive status and baseline visual function measures are given in table 1 for all participants. Mean best corrected visual acuity (BCVA) with the control lens (clear distance prescription spectacle lens) for the group as a whole was 0.23 logMAR (range from 0.06 logMAR to 0.44 logMAR). Average BCVA for near vision with the control lens (clear reading prescription spectacle lens) was 0.27 logMAR (which is approximately equal to 0.8M or slightly better than N8) and ranged from 0.06 to 0.72 logMAR.
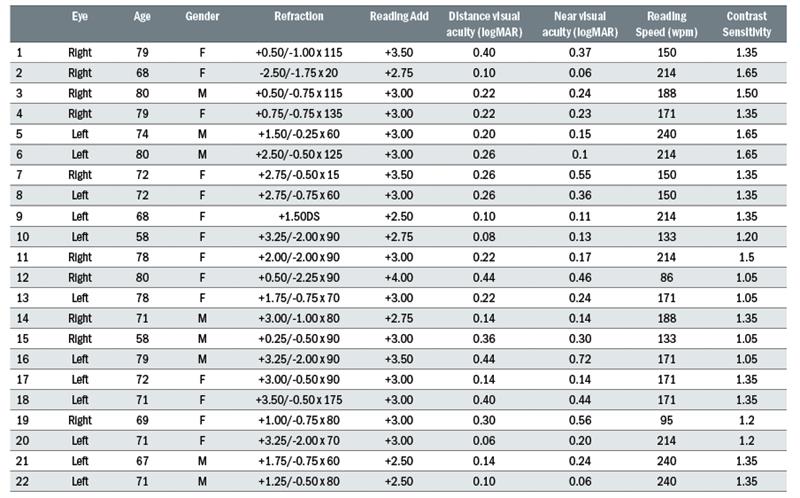
Table 1: Baseline information on participants who took part in the study. Best corrected visual was measured with the ETDRS logMAR chart, contrast sensitivity with the Pelli-Robson chart and near visual acuity and maximum reading speed with the MNRead chart
Visual acuity
Figure 1 shows the effect of each lens condition on mean distance logMAR acuity for all participants. A one-way ANOVA showed that lens condition has a significant effect on distance acuity (F =3.55, p =0.018). Post-hoc analysis (Tukey’s test) showed that acuity was poorer in the control condition (clear spectacle lens) compared to all other lenses, but that there was no significant difference in distance acuity between any of the other three filter lenses. The average improvement in mean distance acuity with the lenses was 0.10 logMAR, with an individual range of improvement between 0 and 0.26 logMAR.
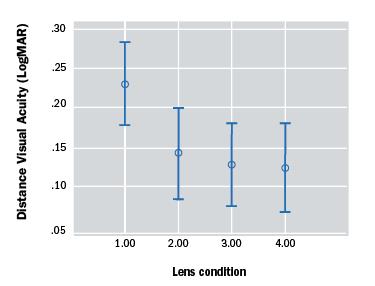
Figure 1: Mean distance logMAR acuity for 22 eyes for each of the seven different lens conditions (error bars represent the 95% confidence intervals). Lens condition 1= Clear spectacle lens, Condition 2= E-Scoop with 4 prism dioptres base-up, Condition 3= E-Scoop with 6 prism dioptres base-up, Condition 4= E-Scoop with 8 prism dioptres base-up
Contrast sensitivity
Figure 2 shows the effect of each lens condition on contrast sensitivity for all participants. Mean contrast sensitivity with the control lens for the group was 1.35 log units (range 1.05 – 1.65). Lens condition had a statistically significant effect on contrast sensitivity (Kruskal-Wallis test, p<0.01) with each of the three lens conditions bringing an average improvement in CS of 0.15 log units (individual range 0-0.45 log units.
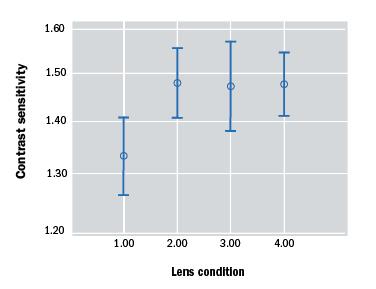
Figure 2: Mean contrast sensitivity for 22 eyes for each of the four different lens conditions (error bars represent the 95% confidence intervals)
Reading acuity and reading speed
Figure 3 shows the effect of each lens condition on reading acuity for all participants. Lens condition did not have a statistically significant effect on reading acuity (Kruskal-Wallis test, p=0.82).
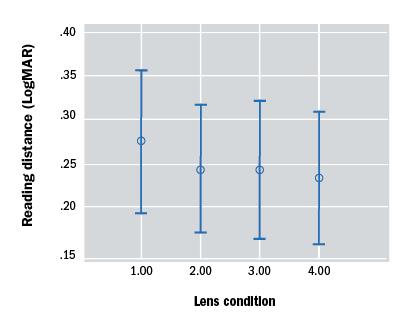
Figure 3: Mean reading acuity for 22 eyes for each of the four different lens conditions (error bars represent the 95% confidence intervals)
Figure 4 shows the effect of each lens condition on reading speed for all participants. Mean reading speed for the clear lens was 178 wpm (range from 86-240). Although the mean improvement in reading speed with each of the lenses was approximately 20wpm (individual increase of between 0 and 64 wpm) a one-way ANOVA showed that lens condition did not have a statistically significant effect on reading speed (F=1.12, p=0.345).
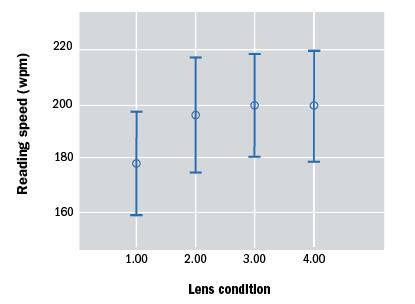
Figure 4: Mean reading speed for 22 eyes for each of the four different lens conditions (error bars represent the 95% confidence intervals
Discussion
Coloured spectacle lenses or wraparound filters have long been suggested as being a useful management strategy in helping individuals with various amounts of functional sight loss, with a wide variety of success previously reported.6-11,14
This study has shown that a new commercially available lens, the E-Scoop can significantly improve VA and contrast sensitivity in a number of individuals with mild vision loss from age-related macular degeneration.
In addition, although the coloured lens does not significantly improve reading acuity for the group as a whole, there was on average a small improvement with reading speed and some individuals did show improvements which would be of significant functional value to them. More participants may have led to a statistically significant improvement in reading speed but this would disguise the fact that there is significant inter-individual variation in response to the lenses with some displaying no change and others benefiting quite considerably.
The E-Scoop lens can be ordered with different amounts of prism incorporated (base up or base down) with the idea that the retinal image will be moved to a healthier portion of the retina than the foveal centre. Recent meta-analysis of the small number of research studies in this area demonstrates the benefit of using prism for low vision rehabilitation after macular function loss with poor acuity.15
However, it also must be noted that one large randomised clinical control trial (225 participants) found that prism spectacles were no more effective than conventional spectacles for patients with AMD.16 Indeed, this study also found from patient feedback questionnaires that prism spectacles may actually add to patient’s problems.16
Several studies have looked at the effect of a variety of coloured lenses/wraparound filters on visual performance and subjective perception of vision but these studies included participant cohorts where baseline visual acuity was often much worse than that of those in the current study.6-11,14 Wolffsohn et al looked at the effect of a variety of different wrap around lenses (yellow, orange, red and grey) on functional and perceived benefits in a small group of patients (n=10) with atrophic AMD, and a small age-matched control (n=5) group worn for seven days.
A yellow or orange wraparound had no statistically significant effect on visual acuity (baseline values were between 0.3 and 0.8 logMAR acuity) although a grey wraparound significantly reduced acuity. However, they did find that yellow and orange increased contrast sensitivity values (measured using computer presented gratings at five spatial frequencies) and concluded that the subjective benefit of coloured lenses is this small enhancement of contrast sensitivity.
Interestingly they also found that the filter colour had no significant effect on total error score of the Farnsworth-Munsell 100 hue test with no change in the angle of confusions in AMD patients. However, there was a significant shift towards the blue-yellow axis with the use of coloured lenses in their controls. We did not assess any effect the E-Scoop has on colour vision in this study.
Bailie et al examined the functional and perceived benefits of wearing coloured filters in patients with AMD. In their study they initially offered their participants the opportunity to try a choice of coloured filters (green, amber, orange and yellow) from which they choose their preferred one to trial for two weeks (as well as a matched neutral density transmission filter as a control).
Almost half of the 39 participants choose the amber filter with the majority choosing a medium intensity. The study showed the filter had no significant effect on binocular visual acuity (mean baseline acuity of group was 0.75 logMAR) or binocular Pelli-Robson contrast sensitivity (baseline average 0.96 log units) but did increase the total error score of the jumbo D-15 colour vision test.
When the vision tests were repeated in the presence of a glare source VA was slightly reduced and CS significantly reduced in all three conditions (no lens, chosen filter lens and ND filter lens). Follow-up telephone questionnaires revealed that the participants felt that the coloured filters had a number of subjective benefits including helping when distinguishing facial features, making objects stand out from one another, watching television and participating in outdoor activities. The subjective benefit from the coloured filters was much greater than that from the neutral density filter.
Langagergaard et al also examined how contrast sensitivity values were affected by two different filter lenses, the Corning 527 and an alternate product the LVI 527 filter (from Multilens) in 32 patients diagnosed with non-exudative AMD.
At 100% contrast neither filter had a significant effect on vision, but CS values improved slightly for the LVI filter at 10% contrast targets. The average change at 10% contrast although statistically significant appears to be of little clinical significance. There was a wide range of acuities included (average 0.6 logMAR) and no information was presented on how baseline acuity may have influenced any improvement with the lenses.
One limitation of this study was that visual function was measured with symbols rather than letters or gratings, which may have some limits in an adult population. The authors report that even in the Corning lens, where there was no measurable change in function, patients felt a subjective improvement in vision. Therefore, the use of a coloured filter in AMD patients may be indicated even where clinical measures of visual function stay at a similar level.
In this study we also investigated the effect of the E-Scoop lens on reading acuity and reading speed. The average reading speed for the group as a whole was 176 wpm with almost a three-fold range in reading speed (range from 86-240wpm). This would be a similar value to that found by Patel et al, who investigated maximum reading speed in a large cohort of AMD patients who had a wide spectrum of disease from drusen to geographical atrophy and scarring from neovascular AMD.17
The lens had no significant effect on reading speed for the group as a whole but there were some individuals whose reading speed improved markedly from the control condition (maximum improvement of 64 wpm). There is no single gold-standard metric for assessing reading function with reading acuity, maximum reading speed and critical print size all being suggested as measuring important aspects of reading.18
One of the limitations to our study was that we only measured reading performance for each lens on a one-off basis with little adaptation time. Previous study has shown that test-retest variability of many reading performance metrics is quite high and that the coefficient of repeatability for maximum reading speed also depends on the analysis method used (although the method we used has been shown to be the most repeatable of the three options with this chart).17
There are several other charts available for measuring reading performance in the clinic and these warrant further investigation in any future studies investigating the functional benefit of coloured lenses.
There is very little published information on the effect of coloured lens filters on reading speed in AMD patients. Eperjesi et al measured reading rates with the Rate of Reading Test with 12 different coloured overlays (Intuitive Overlays) in 12 individuals with non-exudative AMD associated with a relative scotoma and central fixation with an average near visual acuity of 0.60 logMAR (range 0.3-1.00).
They found no evidence that any of the of the coloured light filer overlays improved reading rate. In a further study Eperjesi et al, also examined reading speed with a yellow Corning Photochromic Filter (CPF) 450, a grey neutral density filter and a clear filter in the same AMD group and 12 healthy individuals.
The AMD group demonstrated a statistically significant 5% average improvement in reading speed with the CPF 450 compared with the other filters although some AMD individuals had improvements of 10-15%. Although they question the clinical usefulness of a 5% improvement they conclude, similar to this study, that the use of filters should be considered in AMD patients on a case-by-case basis with consideration of both any measurable functional change and subjective feedback from the patient.
In this study we only examined monocular performance of one eye in all of our participants. However, as the E-Scoop lenses are designed to be prescribed with equal amounts of prism in each eye a measure of binocular function with the lenses would also have been very useful as this will be the individual’s habitual viewing condition.
We did not do this as not all participants had signs of AMD in both eyes and for those with binocular AMD we were limited by time constraints, and wanted to reduce any effect of fatigue caused by repetitive retesting of function. Therefore, the findings of this study must be considered in view that the measurements are for one eye only and do not reflect binocular performance.
Future studies in this area should collect binocular visual function data. Another limitation to this study was that participants were given no period of adaptation time for each of the filter lenses and the participant did not have an extended trial of these lenses to see what benefit they bring to everyday life. It would be interesting to follow-up with some of these participants several weeks or months after using the lenses as several individuals went on to use them after the initial study was completed.
In this type of study design (observational) we also cannot disguise the intervention that the individual is receiving so there may have been a tendency for performance to be enhanced by the very fact that the individual knew they were using the E-Scoop lens rather than just their own glasses, and the benefit for some individuals may simply be a placebo effect.
In conclusion, this study has found the E-Scoop lens can significantly improve a variety of clinical measures of visual performance in AMD patients with minor visual loss which could improve several simple visual function tasks like reading and watching television.
However, there was significant inter-individual variation in functional response to the filters and several individuals who did not show any functional improvement anecdotally reported they felt a subjective improvement in the perception of their quality of vision in the short period for which they wore the lenses.
Future studies with this lens should measure binocular function in patients with a wider range of disease stage and determine their real world functional benefit after an extended period of use with consideration of how to negate any placebo effect. Therefore, clinicians in practice should consider the benefit of prescribing such lenses in individuals with AMD on a case-by-case basis considering any measurable change in function in conjunction with the subjective feedback from the patient.
Dr Raymond Beirne works in the Vision Science Research Group, School of Biomedical Sciences, Ulster University and Noel Meehan is based at Specsavers Opticians, Galway, Republic of Ireland.
References
1 Nivison-Smith L, Milston R, Madigan M, Kalloniatis M. Age-related macular degeneration: linking clinical presentation to pathology. Optom Vis Sci 2015; 91: 832-848.
2 Berdeaux GH, Nordmann JP, Colin E, Arnould B. Vision-related quality of life in patients suffering from age-related macular degeneration. Am J Ophthalmol 2005; 139: 271-279.
3 Neelam K, Nolan J, Chakravarthy U, Beatty S. Psychophysical function in age-related maculopathy. Surv Ophthalmol 2009; 54: 167-210.
4 Hogg RE, Chakravarthy U. Visual function and dysfunction in early and late age-related maculopathy. Prog Retin Eye Res 2006; 25: 249-276.
5 Rein DB, Wittenborn JS, Zhang X, Honeycutt AA, Lesesne SB, Saaddine J. Forecasting age-related macular degeneration through the year 2050: the potential impact of new treatments. Arch Ophthalmol 2009; 127: 533-540.
6 Bailie M, Wolffsohn JS, Stevenson M, Jackson AJ. Functional and perceived benefits of wearing coloured filters by patients with age-related macular degeneration. Clin Exp Optom 2013; 96: 450-454.
7 Eperjesi F, Fowler CW, Evans BJ. Do tinted lenses or filters improve visual performance in low vision? A review of the literature. Ophthalmic Physiol Opt 2002; 22: 68-77.
8 Eperjesi F, Fowler CW, Evans BJ. The effects of coloured light filter overlays on reading rates in age-related macular degeneration. Acta Ophthalmol Scand 2004; 82: 695-700.
9 Eperjesi F, Fowler CW, Evans BJ. Effect of light filters on reading speed in normal and low vision due to age-related macular degeneration. Ophthalmic Physiol Opt 2004; 24: 17-25.
10 Frennesson IC, Nilsson UL. Contrast sensitivity peripheral to an absolute central scotoma in age-related macular degeneration and the influence of a yellow or an orange filter. Doc Ophthalmol 1993; 84: 135-144.
11 Wolffsohn JS, Dinardo C, Vingrys AJ. Benefit of coloured lenses for age-related macular degeneration. Ophthalmic Physiol Opt 2002; 22: 300-311.
12 Greenstein VC, Santos RA, Tsang SH, Smith RT, Barile GR, Seiple W. Preferred retinal locus in macular disease: characteristics and clinical implications. Retina 2008; 28:1234-40.
13 Elliott DB, Sanderson K, Conkey A. The reliability of the Pelli-Robson contrast sensitivity chart. Ophthalmic Physiol Opt 1990; 10: 21-24.
14 Langagergaard U, Ganer HJ, Baggesen K. Age-related macular degeneration: filter lenses help in certain situations. Acta Ophthalmol Scand 2003; 81: 455-458.
15 Markowitz SN, Reyes SV, Sheng L. The use of prisms for vision rehabilitation after macular function loss: an evidence-based review. Acta Ophthalmol 2013; 91: 207-211.
16 Smith HJ, Dickinson CM, Cacho I, Reeves BC, Harper RA. A randomized controlled trial to determine the effectiveness of prism spectacles for patients with age-related macular degeneration. Arch Ophthalmol 2005; 123: 1042-1050.
17 Patel PJ, Chen FK, Da Cruz L, Rubin GS, Tufail A. Test-retest variability of reading performance metrics using MNREAD in patients with age-related macular degeneration. Invest Ophthalmol Vis Sci 2011; 52: 3854-3859.
18 Rubin GS. Measuring reading performance. Vision Res 2013; 90: 43-51.
