Case study
Patient initials: MR Age 39
Condition: microbial keratitis
Date of initial assessment with us October 29, 2016.
History
MR phoned the practice from Bangladesh on October 24, where they were currently on business, to arrange urgent appointment on their return to discuss an issue acquired while abroad.
Normally an extended wear contact lens wearer, MR had developed a red and painful left eye. They saw a GP in the American embassy who arranged a private consultation with a local ophthalmologist who prescribed:
- Moxifloxacin (two hourly)
- Tropicamide (four times daily)
- Lubricants (as needed)
They were also advised to consult an ophthalmologist on return but had experienced difficulties arranging a suitable HES appointment so had contacted us to be seen as a Band 1 Eye Health Examination Wales patient.
Symptoms
On attendance, they reported:
- Left eye is still very sore but not red
- Some left periorbital discomfort
- Left photophobia
- Vision feels blurry in the left eye
- No discharge.
Patient was observed to be partially closing left eye. Due to problems in seeing an ophthalmologist in Bangladesh, MR claimed the drugs prescribed were based around what was available in the doctor’s drawer at the time. The patient also expressed concerns about the onsite storage of drugs, as they were clearly labelled as requiring storage at less than 25º C, but the temperature the patient was travelling in was frequently hotter than this.
The right eye felt completely normal with no redness, discharge, blurring or other symptoms of note.
Current contact lens wear
Coopervision Biofinity
R; 8.6/14.00/-2.25 BCVA @ last visit in January 2016 6/6
L; 8.6/14/00/-1.75 BCVA @ last visit in January 2016 6/6
Wear modality: extended wear and usually wears lenses for full month. Last check was in January 2016.
Has only been using a lens in the right eye since infection, but today attended wearing glasses.
General health
Good; no tablets, medication or reported allergies
Previous ocular history
Has previously reported dryness in LE and occasional blurring of vision.
In 2014 was noted that this eye does not always fully close when sleeping.
The LE orbit received a fracture from an injury sustained kick boxing in 2007 requiring insertion of a metal plate. Has been using glasses since age of 14.
Family history
Nothing reported
Occupation
Inspection engineer – frequent foreign trips.
Hobbies/interests
Kick boxing
Non-smoker
Current refraction and acuities January 2016
RE -2.00/-0.25x75 6/5
LE -1.75/-0.50x150 6/5
Acuities recorded today
RE 6/5
LE 6/6
Clinical findings
LE pupil mid-dilated and slow to react – Px has been using tropicamide 1% which was last used two hours previously. Has noted himself that comfort of eye is improved when using tropicamide.
RE normal reactions to light and accommodation.
No RAPD observed.
RE external examination
Lids, lashes, sclera, conjunctiva and cornea healthy – no redness / follicles / papillae or other issues of note.
Anterior chamber – clear and quiet – no cells / flare. Deep and Grade IV Van Herrick.
No fluorescein staining.
LE external examination
Lids, lashes, sclera and conjunctiva healthy – no redness / follicles / papillae or other issues of note.
Anterior chamber – clear and quiet with no cells or flare.
Cornea shows superior temporal to pupil 0.5mm resolving ulcer – outer ring shows original size of 1mm with moderate haze. Some take up of fluorescein into anterior stroma.
Central ulcer still has slightly white appearance.
Attempted anterior OCT capture of image to assess depth – not ideal but did get scan (figures 1 and 2).
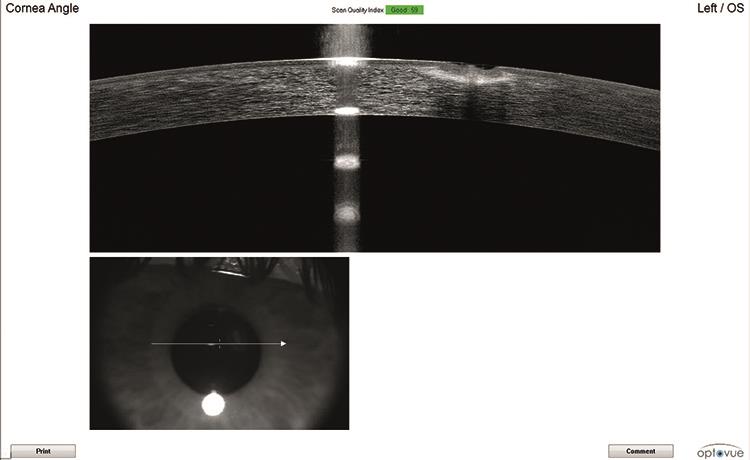
Figure 1: Cross section of ulcer at presentation
Internal examination (Volk Superfield) R&L
Vitreous; clear
Optic Nerve; healthy margins, healthy NRR, ISNT followed, moderate cupping – CD 0.5. Stable c/w previous photos. Moderate vertical ONH size.
Vessels normal – 2/3 AV ratio
Macula – Sharp reflex
Peripheral retina healthy
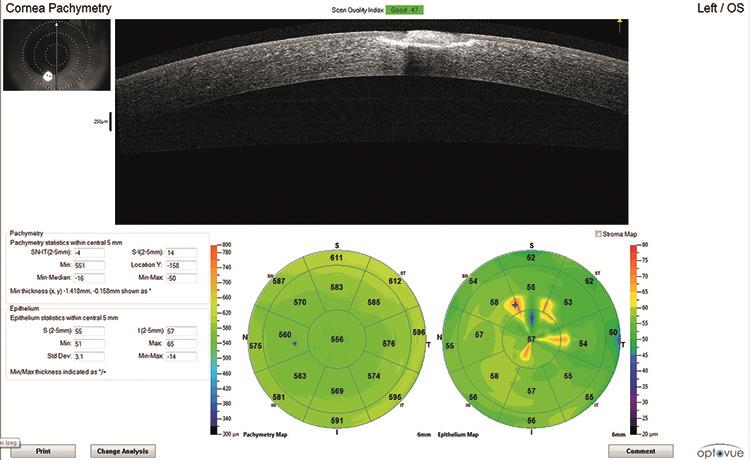
Figure 2: Surface map at presentation
Management
Out of hours access to ophthalmology is challenging in West Wales and on call was in Bronglais Hospital, Aberystwyth, 60 miles and 1.5 hours away. The eye was quiet and the ulcer was appearing to heal. The patient had access to moxifloxacin eye drops which, while not commonly used in the UK, are a fluoroquinolone class eye drop which would usually be the first line of therapy in the UK.
He was running low on tropicamide eye drops so I issued two single dose units of cyclopentolate for use nocte. I advised him to continue his current regime of two-hourly moxifloxacin, tropicamide qd while it lasts and cyclopentolate nocte. I arranged a follow up appointment on Monday with clear guidance that, in the unlikely event that things regressed, he was to attend the practice on Sunday or to simply contact A&E.
A letter was sent to the GP detailing the condition and proposed management as required under EHEW regulations.
Follow up 1
Monday, October 31
Feeling much better – had actually felt 100% better on Sunday but today felt more ‘blinky’.
VA in current glasses RE 6/5 LE 6/6
LE External examination
Lids, lashes, sclera and conjunctiva healthy – no redness / follicles / papillae or other issues of note.
No cells / flare.
Corneal defect improving now <1/4mm but still persistent stain centrally – not penetrating to stroma now.
Clear improvement shown on anterior OCT. Epithelial and general corneal thickness maps were improving.
Patient reports running low on moxifloxacin.
Management
Spoke to mid-grade ophthalmologist at West Wales General – as lesion was still present and patient was running low on moxifloxacin, she suggested switching to UK normal ofloxacin for use QD and was happy with me to review on Thursday.
I wrote to GP requesting a prescription for ofloxacin QD and indicated that this was as advised by ophthalmology. A colleague phoned the surgery who indicated that the GP had been happy to do this and the patient had obtained the ofloxacin.
Follow Up 2
Tuesday, November 1
Patient had contacted practice in morning c/o worsening issues with glare and feeling of blur. Feeling more photophobic.
VA in LE today 6/7.5 in current glasses, noticeably more difficult than at previous visit.
Refraction
RE -2.25DS 6/5
LE -2.50DS 6/5
LE external examination
Lids, lashes, sclera and conjunctiva healthy – no redness / follicles / papillae or other issues of note.
No cells / flare.
Still a small epithelial defect, with no stromal and only epithelial staining.
Anterior OCT confirmed epithelium is healing (figure 3).
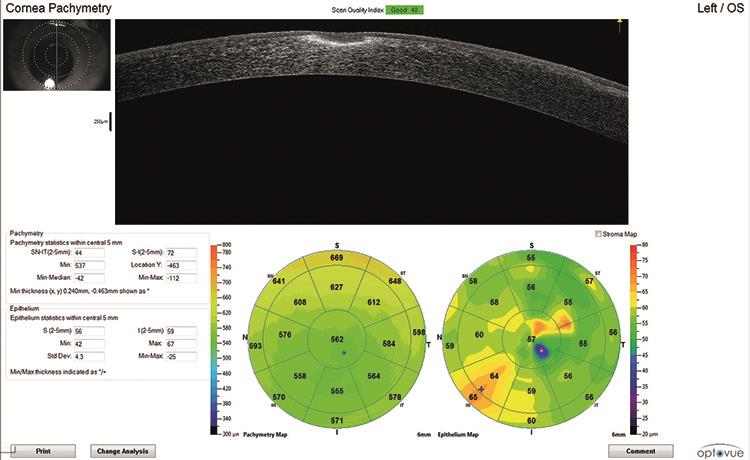
Figure 3a: Surface map showing significant change since last assessment
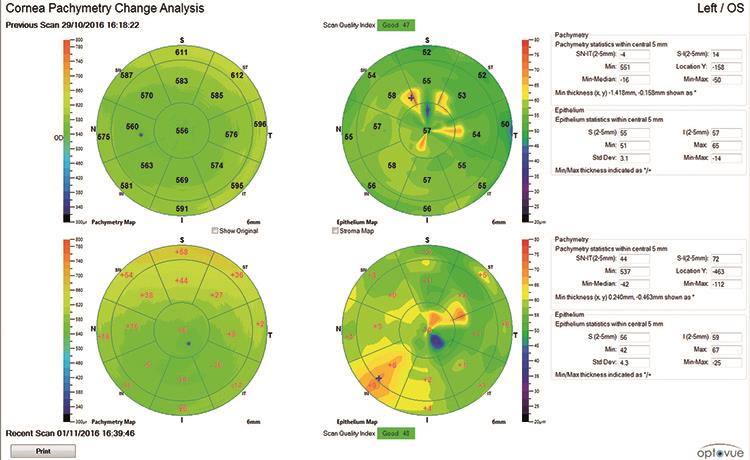
Figure 3b: Surface map showing last assessment
Management
Patient was greatly reassured by finding that VA could be improved. Explained that it was possible that scarring had subtly altered corneal profile inducing more myopia. Keep review appointment already scheduled for Thursday. PR is travelling to Jordan on Monday for week and as current spectacles were giving poor VA and contact lenses are contraindicated at this stage requested glasses be made to Rx above for use while problems resolves. He is aware that his prescription may change further once healing completed.
Thursday, November 3
Vision feeling better though still somewhat variable. Px collected new glasses for upcoming trip and immediately felt vision to be improved.
VA in new glasses 6/5 R&L
LE external examination
Lids, lashes, sclera and conjunctiva healthy – no redness / follicles / papillae or other issues of note.
No cells / flare.
Tiny remnant of epithelial defect – annulus of negative stain adjacent to rough looking epithelial staining.
Continue with ofloxacin qd to provide cover while away in Jordan.
MR to see how he feels about glare whilst away with new Rx – if still issues recheck with me on return. Else suggested return for full sight test to ascertain post injury refractive outcome and to have discussion about resuming CL wear.
Monday, November 22
Routine refraction and sight test revealed stable prescription. Patient was refitted into daily disposable silicone hydrogel lenses. No further problems or intervention required.
Discussion
Microbial keratitis is more common in contact lens wearers and more so in extended wear. It is interesting to note that the prevalence has not fallen as far or fast as expected with the advent of daily disposable silicone hydrogel lenses. Standard RGP lenses still present the lowest risk with between 0.4 to 4.0 incidents per 10,000 patients rising to 20.9 per 10,000 in extended wear. It has also been noted that increased use of cosmetic coloured contact lenses and the rise in orthokeratology may be implicated in the rise in microbial keratitis. As well as a rise in number there has also been a rise in severity of keratitis reported.1
Microbial keratitis can be caused by a variety of organisms such as bacteria (Staphylococcus spp, Streptococcus spp, Pseudomonas aeruginosa), viruses, Acanthamoeba, Fusarium etc. A recently published 12-year study from Manchester Royal Eye Hospital (MREH) shows 63.3% of cases were Gram positive, 27.3% were Gram negative, 7.1% were fungal and 2.3% were Acanthamoebal.3
Treatment of a corneal ulcer would ideally often involve taking a culture from the cornea to identify the specific organism to ensure that an appropriate antibiotic is being used, especially to identify whether the organism is Gram positive or Gram negative. Gram negative organisms have an outer cell wall that does not take up the crystal violet stain used in the Gram stain test. Obviously, in the case presented here, following a course of moxifloxacin a corneal swab would have yielded very little useful information, though it might still have been considered should the ulcer have failed to respond.
Typically, in the UK such presentations would be treated with a fluoroquinolone, and in more complex cases, especially those where antibiotic resistance occurs a fortified antibiotic such as cefuroxime-gentamicin may be used. The MREH study also showed that ofloxacin covered 83.1% of Grampositive and 90.8% of Gram negative cases whilst cefuroxime covered 86.6% of Gram positive and 61.4% of Gram negative.
Gentamicin is highly efficacious with 88.8% cover for Gram positive and 96.5% cover for Gram negative.3 This study also noted that there is no significant rise in in-vitro resistance in the UK. It is worth noting however, that gentamicin is quite toxic to the corneal epithelium so, perversely, can slow down wound healing.4
Though commonly the guidance is not followed chloramphenicol should not be issued to a contact lens wearing patient with a suspect infection specifically due to the increased prevalence of Pseudomonas aeruginosa infections in contact lens wearers and against which chloramphenicol is ineffective.
Some ophthalmologists advocate the use of a topical steroid to reduce inflammation and scar formation once the initial wound is sterile though there is not a strong evidence base to support this in practice.5,6
Acute presentation of an infective keratitis is a high risk emergency that is unlikely to be managed in primary care. Specifically, as a corneal scrape should be taken for culture prior to starting an antiobiotic therapy.7
In this instance having an IP qualification would have facilitated MR’s management as I would have been in a position to directly arrange and manage this patient to resolution without having to trouble either ophthalmology or the patient’s General Practitioner.
Next month we will consider enhanced service management of a glaucoma patient.
References
1 Cheung, N. et al. 2016. Emerging trends in contact lens-related infections. CURRENT OPINION IN OPHTHALMOLOGY 27(4), pp. 327–332.
2 Coleman, A.L. et al. 2013. Bacterial Keratitis Secretary for Quality of Care- Cornea/external disease preferred practice pattern development process and participants. American Academy of Ophthalmology Cornea American Academy of Ophthalmology . Available at: www.aao.org/ppp.
3 Tan, S.Z. et al. 2017. Twelve-year analysis of microbial keratitis trends at a UK tertiary hospital. EYE 31(8), pp. 1229–1236.
4 Tuft,S,Burton, M. 2013. Microbial keratitis. FOCUS,The Royal College of Ophthalmologists , pp. 1–5.
5 Ni, N. et al. 2016. Use of adjunctive topical corticosteroids in bacterial keratitis. CURRENT OPINION IN OPHTHALMOLOGY 27(4), pp. 353–357.
6 Tallab, R.T. and Stone, D.U. 2016. Corticosteroids as a therapy for bacterial keratitis: an evidence-based review of `who, when and why’. BRITISH JOURNAL OF OPHTHALMOLOGY 100(6), pp. 731–735.
7 College of Optometrists 2017. Microbial keratitis (bacterial, fungal). Available here
Andy Britton is an optometrist and co-director of Specsavers Haverfordwest in South Wales (and currently undertaking IP qualification).
