
Sjögren’s disease (or more accurately syndrome, as the condition can affect multiple sites throughout the body) does not always present as a variation on dry eye disease. Here are two cases involving symptoms of twitching, throbbing and shooting pains.
Case 1
An 85-year-old female rang to say she had been experiencing sharp ‘electric shocks’ on the right side of her face. She had been experiencing them sporadically on a daily basis for the past few days, and now they were happening at increasingly regular intervals. She was now very concerned and was afraid to touch her face.
Ocular examination
• Visual acuity:
• R: 6/18 due to previous episode of atypical optic neuritis some 20 years ago
• L: 6/7.5 with clear intraocular implant and no optic disc abnormality, except for peripheral laser photocoagulation following retinal detachment
• Intraocular pressures: R 17mmHg & L 16mmHg
• Right OCT scan shows no progression of loss of nerve fibres or ganglion cell loss (figure 1)
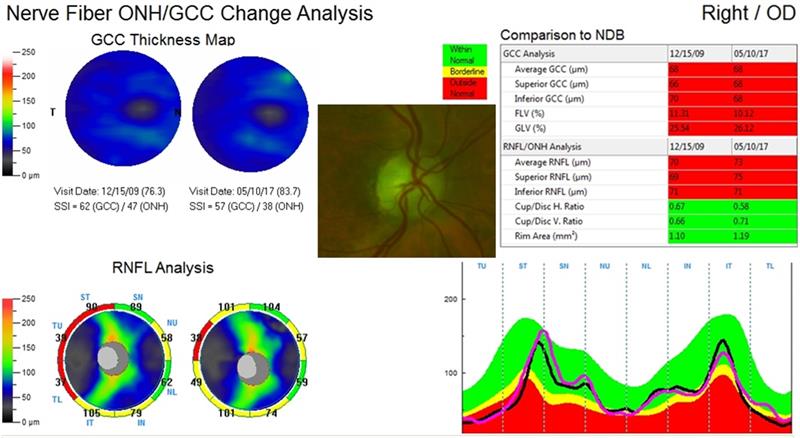
Figure 1: OCT scan results for the right eye showing a pale optic disc (centre) due to previous optic neuritis episode. The ganglion cell complex (top left) and retinal nerve fibre layer analysis (bottom left) show no change from previous scans in 2009 and minor increase in values from 2017 (comparative data on right).
Management
The patient was referred to a neurologist with a tentative diagnosis of trigeminal neuralgia. Possible unstated causes of this might be
multiple sclerosis (although unlikely due to her age), a swollen vessel pushing onto the trigeminal nerve, or an isolated atypical inflammation of the trigeminal nerve.
Neurological assessment
The antibodies that target ‘normal’ proteins within the nucleus of a cell are called antinuclear antibodies (ANA). Lumbar puncture and blood tests revealed increased ANA antibodies in this patient, implying some sort of autoimmune disease.
A brain scan revealed a few white spots on the cerebral cortex. These were thought to be age-related changes rather than sclerotic plaques due to inflammation as might indicate multiple sclerosis.
A diagnosis was made of trigeminal neuropathy (rather than trigeminal neuritis), and she was described as having an underlying autoimmune neuroinflammatory condition; specifically, Sjögren’s disease. Interestingly, the patient did not have symptoms of dry mouth, dry eyes or joint pains (often described as the Sjögren’s triad), yet the neurologist was certain that it was Sjögren’s disease. He prescribed the following drugs to help relieve the ‘sharp electric shocks’:
• Gabapentin 100mg (3x a day)
• Indomethacin (a non-steroidal anti-inflammatory) 50mg (2x a day)
Case 2
A 43-year-old, previously healthy, female patient reported noticing a loss of peripheral vision in her left eye for an hour before bedtime. Next morning, the vision had recovered, but now the patient was aware of a ‘film’ in front of the left eye. There was some throbbing on the left side of her head. What alarmed her most was the concurrent experience of ‘pins and needles’ and slight shooting pain along the right arm.
Ocular examination
• Visual acuity; R and L; 6/6 and N5
• No ocular muscle abnormalities; orthophoria
• No anterior or posterior retinal abnormalities
• Vitreous; early condensation and liquification changes in both eyes
• Visual fields; no visual pathway abnormalities
Management
The patient was referred to her general practitioner to eliminate hypertension, diabetes, hyperlipidaemia or blood dyscrasias (blood thickening diseases) as a cause of the symptoms. It was also stipulated that she be referred to a neurologist to eliminate trigeminal neuropathy or a trapped nerve as possible contributing causes.
Neurological assessment
Blood tests all proved negative. The peripheral visual aura was confirmed as due to visual migraine and aspirin was prescribed as a prophylactic.
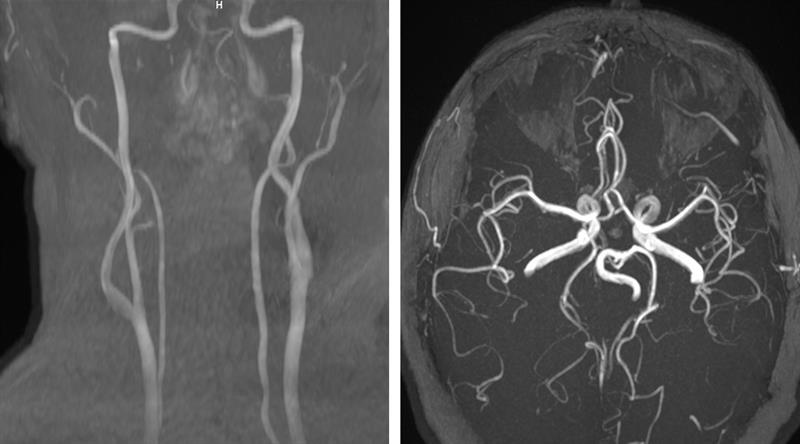 Figure 2: MRA of the neck (left) showing no stenosis of the carotid or vertebral arteries. MRA of the head (right) showing the basilar, internal carotid, anterior cerebral, middle cerebral and posterior cerebral arteries with good patency an no signs of occlusion.
Figure 2: MRA of the neck (left) showing no stenosis of the carotid or vertebral arteries. MRA of the head (right) showing the basilar, internal carotid, anterior cerebral, middle cerebral and posterior cerebral arteries with good patency an no signs of occlusion.
Brain scans revealed no intracranial concern and an MRA (magnetic resonance angiogram) confirmed patent cerebral vessels (figure 2). MRI (magnetic resonance interferometry) of the neck showed bulging discs at the level of C5 and C6 vertebrae (figure 3). This would account for the symptoms of ‘pins and needles’ along the right arm. No treatment was given for this except physiotherapy initially and if the nerve sensation continued then acupuncture as a second line of treatment.
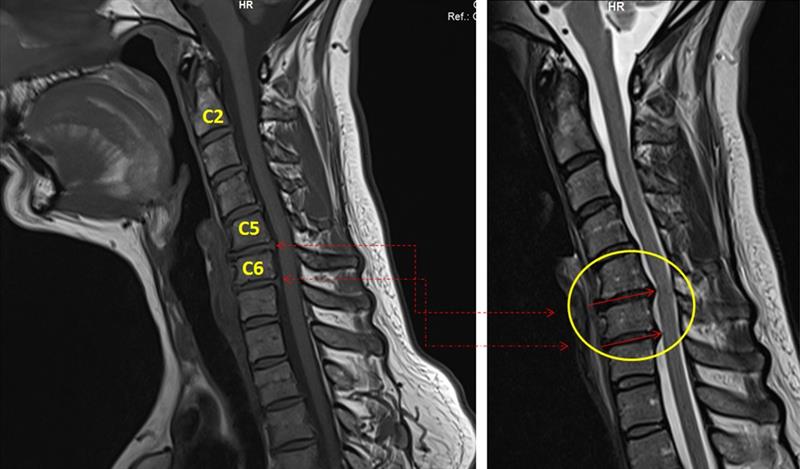 Figure 3: MRI of the neck showing bulges at the level of vertebrae C5 and C6. Bulging or herniating discs are pushing against the white cerebrospinal fluid, and this is shown as a stenosis or narrowing of the space behind the spine. The herniating discs may press against the spinal cord, including the nerves innervating the shoulder and arm and may give rise to sensation or numbness in these areas.
Figure 3: MRI of the neck showing bulges at the level of vertebrae C5 and C6. Bulging or herniating discs are pushing against the white cerebrospinal fluid, and this is shown as a stenosis or narrowing of the space behind the spine. The herniating discs may press against the spinal cord, including the nerves innervating the shoulder and arm and may give rise to sensation or numbness in these areas.
The neurologist further suggested that the patient have an electrodiagnostic test, namely visual evoked potential (VEP), to rule out any signs of optic neuritis or related demyelination problems. I undertook this, and the VEP results showed no latency or amplitude issues with the myelin sheath signal processing (figure 4).
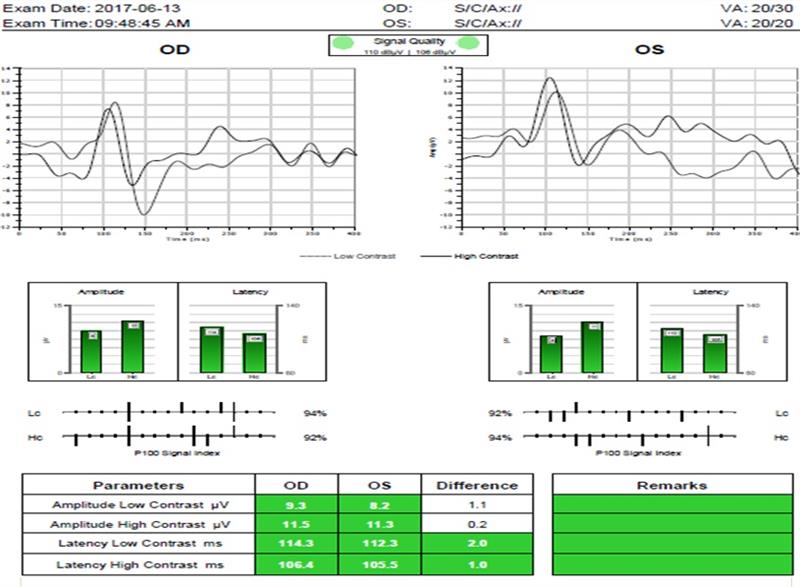
Figure 4: Visual evoked potential showing no latency in the myelin sheath transfer of information along the visual pathway and a good amplitude response from the retinal ganglion complex.
Discussion
Sjögren’s syndrome
Sjögren’s syndrome is a systemic autoimmune disease that may affect the entire body. It is a chronic disease in which the white blood cells attack the moisture producing glands and mucous membranes.
The first symptoms usually include extensive dryness of the eyes, mouth, vagina, skin and lungs. The latter is usually the cause of a persistent dry cough. Other complications include profound fatigue, chronic joint pain (often reported as a stiffness and swelling) and neuralgia (nerve pain).
There is also an association with lymphoma, a malignancy of the lymphocytes found in the lymph nodes, spleen, thymus and bone marrow. Sjögren’s can occur with other autoimmune conditions, such as systemic lupus erythematosus (SLE) or rheumatoid arthritis.
Sjögren’s syndrome typically first presents in people aged between 40 and 60 years, and is more common in women than in men. It is thought to have both genetic and hormonal influences. Oestrogen hormone is thought to play a pivotal role, and hence the greater incidence in females. Usually, it is triggered by a viral or bacterial infection rallying the white blood cells which not only fights the infection but also attacks the body’s own cells.
Blood tests confirm the presence of anti-nuclear antibodies. For defence against infection our body releases antibodies, and the antibodies that target normal protein within a nucleus are called anti-nuclear antibodies (ANA). The presence of large amounts of ANA can
indicate autoimmune disease such as Sjögren’s. Seventy percent of Sjögren patients are positive to antibody ANA.
Cervical spine
The cervical spine has seven vertebrae with soft discs between them. With age, the discs bulge (or herniate) and push against the spinal cord or nerves that supply the neck, shoulder, arms and legs. When the upper herniating discs (C1-C8) are affected, patients will experience shooting pains or numbness along the neck, shoulders and arms. When the lower spine discs are affected (L1-L5), the lower limbs are affected and cause sciatica.
Sciatica pain can be debilitating for patients and usually happens in the 30 to 50 year age group. The sciatic nerve is the largest nerve of the body and runs either side of the lower spine through deep into the buttocks, back of the thighs and all the way down to the foot. Pain usually affects one leg and there may also be feelings of numbness, weakness, tingling or shooting pains. Figure 5 shows herniating discs affecting L4 & L5 part of the lower vertebrae.
 Figure 5: Herniation of the discs at the level of vertebrae L3 and L5 resulting in pinching of the lower back nerves and resulting in sciatic pain.
Figure 5: Herniation of the discs at the level of vertebrae L3 and L5 resulting in pinching of the lower back nerves and resulting in sciatic pain.
Conclusion
Hopefully, I have given an insight into shooting pains that can occur throughout the body and shown how conditions we may consider as ocular have significant impact and related associations throughout the body.
Kirit Patel is an optometrist in independent practice in Radlett, Hertfordshire.
