A scleral lens can be defined as a lens fitted to vault over the entire cornea, including the limbus, and lands on conjunctiva overlying the sclera (figure 1). Scleral lenses are becoming more popular and are indicated for a number of reasons.
Despite the increasing interest in, and use of, scleral contact lenses in the UK in recent years, most eye care practitioners (ECPs) in primary care will have limited experience of them. It is with this in mind that this CPD exercise has been developed and, indeed, your feedback suggested the rarity of dealing with such lenses in community practice. The source material was based upon the BCLA CLEAR paper on scleral lenses.1
Case for Discussion
A patient who has been previously fitted with scleral contact lenses in a hospital department has contacted your practice. They are unable to attend their six-month aftercare appointment at the hospital and have asked whether your practice might be able to offer this service. They do not require a full eye examination, as this is not due for another six months. You are much nearer and the hospital are happy for you to do so, if you have the capability.
- What might be the reason that this patient was fitted with scleral contact lenses in the first place?
- What would you say is the minimum equipment to be able to undertake this aftercare?
- What would be the key signs and symptoms to look out for when undertaking an aftercare on a scleral contact lens wearer?
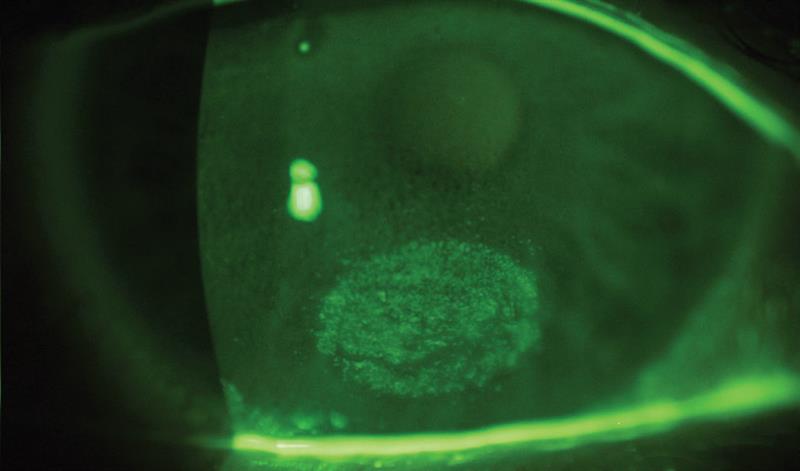
- When assessing the cornea with fluorescein after lens removal, you see a discrete zone of staining (figure 2; appearance after lens removal, pictured below). What might be the cause of this and what course of action (either by you or the hospital clinic) might be indicated?
Indications for Scleral Lenses
According to the BCLA CLEAR paper, there are a number of indications for scleral lenses and these have changed over recent years.
There are numerous optical and therapeutic indications to prescribe scleral lenses2,3. During the 1980s, when scleral lenses were first manufactured in gas permeable materials, the most common conditions treated were:
- 44% high ametropia: aphakia and myopia
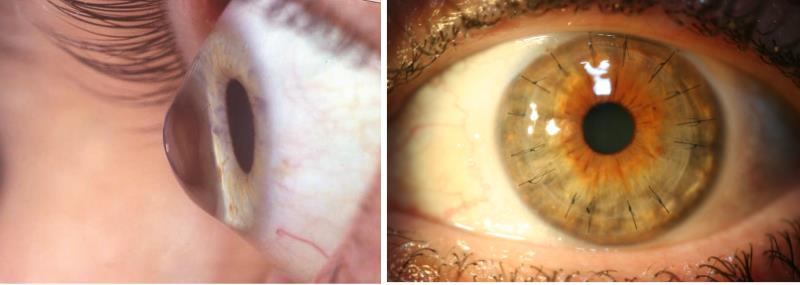
- 32% primary corneal ectasia: keratoconus, pellucid marginal degeneration, keratoglobus (figure 3; Keratoglobus, below)
- 12% post-penetrating keratoplasty (figure 4; Penetrating keratoplasty, below)
- 7% ocular surface disease
Since the advent of silicone hydrogel soft contact lenses used for the refractive correction of aphakia and high myopia, the most common clinical conditions treated with modern highly oxygen permeable scleral lenses are:
- 53% primary corneal ectasia
- 18% ocular surface disease
- 17% post-penetrating keratoplasty
Modern scleral lenses are also used for the correction of simple refractive errors, including presbyopia, particularly when other modalities fail due to vision or comfort issues.
There are some contraindications cited in the literature. These include corneal endothelial abnormalities with reduced endothelial cell density and Fuchs’ endothelial corneal dystrophy. Also, glaucoma patients might not be suitable to fit, especially where there is raised intraocular pressure or there might be aggravation of drainage devices or a bleb. Also, overnight wear is not advisable.4
Your comments included the following: ‘Almost all the patients we’ve accounted that were fitted with scleral lenses at the hospital have had irregular corneas, mainly keratoconus with some continuing to wear the lenses after keratoplasty.’
Minimum Equipment

As one respondent put it succinctly: ‘Obviously a slit lamp, a keratometer, or better still a corneal topographer, and a scleral fitting set with fluorescein and copious amounts of saline are paramount for this type of lens fitting. We also found the large rubber suckers useful to help the patients insert the lenses (figure 5).’
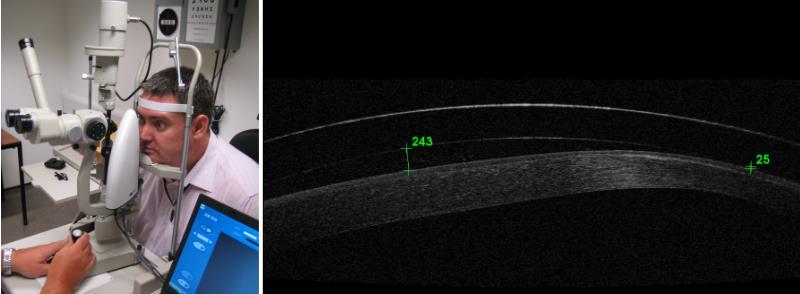
Other instruments mentioned by some of you as to be of benefit when dealing with scleral lenses included anterior OCT (figure 6), which can help visualise the fit and landing area, and specular microscopes (figure 7), which might indicate when endothelial cell density is not adequate to support safe scleral wear.
Figure 6 & 7: Specular microscopy to assess endothelial cell density; Anterior OCT showing scleral lens
Aftercare Signs and Symptoms
As one respondent put it: ‘Aftercare starts with visual acuities, then slit lamp examination of the corneas (for signs of oedema, hypoxia, neovascularisation and corneal staining). The fit and condition of the lenses would also need to be assessed.’
Another respondent listed firstly the symptoms to look out for:
- Pain
- Discomfort
- Reduced wearing time
- Photophobia
- Tearing
- Poor / reduced / unstable vision
And then the signs:
- Conjunctival injection
- Tearing
- Photophobia
- Corneal Staining
- Corneal oedema
- Conjunctival indentation
- Conjunctival prolapse
- Lens surface deterioration
- Midday fogging
- Epithelial bogging
Regarding the area of staining (as shown in figure 2), a number of suggestions were given. One of you correctly suggested: ‘Normally any visible corneal staining is usually associated with the back surface of the lens not completely vaulting the corneal surface. So, increasing the sagittal height would be appropriate.’
Others felt that the stain was related to a trapped air bubble. As in this case: ‘If a bubble remains after correct reapplication, and the use of a more vicious application fluid, it could be an indication that a more appropriated fluid reservoir thickness should be considered.’ Though this is unlikely, the need to reassess the fit and adjust accordingly should result in a positive outcome.
Neil Retallic says
In the 2021 International contact lens prescribing report, 22% of rigid material fits were scleral lenses, although rigid lenses as a group (excluding ortho-k) were only 11% of all lens fits.5 The fact scleral lenses vault the cornea is advantageous, especially for those with corneal-related pathology, irregularities and/or ocular surface disease. The future direction of the scleral lens is promising, including for non-optical use, given battery-operated devices can be embedded with less chance of becoming wet.
For those new to approaching scleral lens fitting there are fantastic resources and workshops available and often experienced practitioners are happy to provide mentorship. Suppliers are readily on call to provide support, following the fitting guide and using software programmes are useful when it comes to optimum lens selection and fit refinement. The absolute minimum equipment to assess the lens fit on eye is a slit lamp, although having more sophisticated imaging instrumentation (such as a topographer, photography or/and anterior OCT) are advantageous for baseline monitoring, reviewing ocular surface shape and to understand key characteristics such as centration, sagittal height, clearance, fluid reservoir thickness, landing zone etc. Using patient reported outcomes are useful along with visual assessments to understand the ‘real world’ performance.
Educating the whole team on the best handling techniques and care procedures and a reminder of the need for regular follow up reviews are important to help maximise success.
- Neil Retallic is President of the BCLA and Head of Professional Development at Specsavers.
Source Material
- Barnett M, Courey C, Fadel D, Lee K, Michaud L, Montani G, van der Worp E, Vincent SJ, Walker M, Bilkhu P, Morgan PB. CLEAR - Scleral lenses. Contact Lens & Anterior Eye, 44, 2021, 270-288
- van der Worp E et al. Modern scleral contact lenses: a review. Contact Lens & Anterior Eye, 2014;37(4):240–50.
- Schornack MM. Scleral lenses: a literature review. Eye & Contact Lens 2015;41(1):3–11
- Fadel D, Kramer E. Potential contraindications to scleral lens wear. Contact Lens & Anterior Eye, 2019;42(1):92–103.
- www.clspectrum.com/issues/2022/january-2022/intern...
