
In the discussion of the first interactive exercise, which looked at the initial choice of correction of presbyopia, I expressed my surprise at the clear split in responses between those favouring multifocal lenses and those preferring monovision. A healthy topic for discussion should always reveal some divergence of views, and it would appear that this second exercise has similarly shown a split of opinion among respondents.
I think it is safe to suggest that the debate about whether to choose a conventional hydrogel or a silicone hydrogel as first choice for daily disposable contact lens wear is still alive and well. For example, it was only last year during an online education event (see Optician 07.05.21), that a healthy discussion between Professors Nathan Efron and Phil Morgan touched upon the subject, with Efron tending to emphasise the benefits of a silicone material while Morgan defended the many benefits of a hydrogel approach. The debate has also been covered in this publication, with reviews of the topic reflecting a wide literature base to support either material choice.1,2
This was the very core of the discussion you were invited to take part in and it would seem that, when seeing a daily disposable hydrogel wearer presenting at aftercare with no signs of any hypoxic stress, there is an almost exact 50/50 split between those wanting to refit with a silicone hydrogel lens and those wanting to leave the patient as they are.
The Case for Discussion
The case focused on a 28-year-old male attending for his 24 month aftercare. He is currently wearing conventional hydrogel daily disposable contact lenses. His wearing time averages at 12 hours per day, seven days a week. He reports no concerns regarding vision or comfort and scores each as 10/10.
On examination, there is no evidence of hypoxic stress and no sign of any adverse event.
You were asked to discuss with a colleague the following:
- What are the early indicators of hypoxic stress that might be looked for in the consulting room?
- Would you consider changing this patient to a different type of lens? Please offer your reasoning for your answer.
- How would you explain your decision to the patient?
Hypoxic Stress
Not surprisingly, the vast majority of respondents were able to relate the signs to look out for as early indicators of hypoxic stress, surely a key part of any aftercare when seeing a patient wearing any lens for long hours and particularly one with a lower oxygen transmissibility. A couple of points are possibly worth making here. Quite a few reports seemed to imply that neovascularisation should be mentioned as an ‘early indicator’. I would disagree here and instead suggest that, were we to see limbal neovascularisation related to hypoxia, we have not been following the patient adequately.
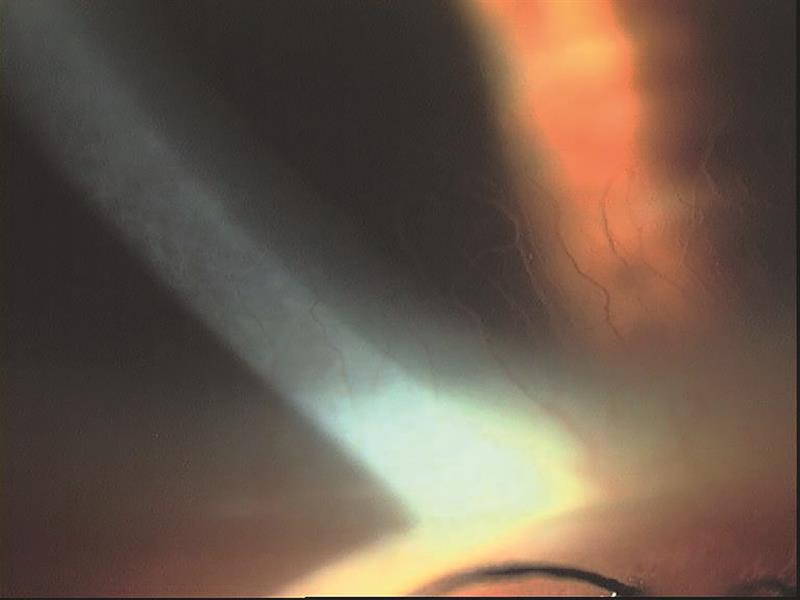 Neovascularisation
Neovascularisation
My second point is that, by asking about hypoxic stress first, I worry that this may have unfairly influenced the following discussion about management by implying a potential problem where one might not exist. Here are some of your responses.
An answer most representative of the feedback might be: ‘Signs of hypoxic stress to watch for would be corneal oedema, a significant presence of microcysts, conjunctival oedema, corneal neovascularisation and corneal infiltrates.’ Another implied that the latter might not be an expected change: ‘Possible signs of oedema, microcysts or neovascularisation that were not evident at the patient’s previous check would be indicative of hypoxia, although this would be unlikely if his wearing modality, general health and medication, if any, had not changed.’
Perhaps a more realistic answer, bearing in mind that I am sure few of us spend much time scanning the epithelium at high magnification for microcysts, might be this one which stated early hypoxia signs to look for being ‘dilation of limbal vessels especially if observed at an early in the day aftercare and in the absence of any possible solution reaction. Had pachymetry readings been available from prior to starting lens wear and a pachymeter available, then an increase might indicate the overall oedema associated with soft contact lens wear. A decrease in wearing time might also indicate reduced tolerance due to lack of oxygen.’ I like the mention of corneal thickness change and hope, one day, anterior OCT availability will make this an easy and integral part of any aftercare.
Finally, a few mentioned diffuse staining as a sign of hypoxic stress (a sensible point to make), while others mentioned stromal striae (certainly a hypoxic sign, but most unlikely in early hypoxic conditions).
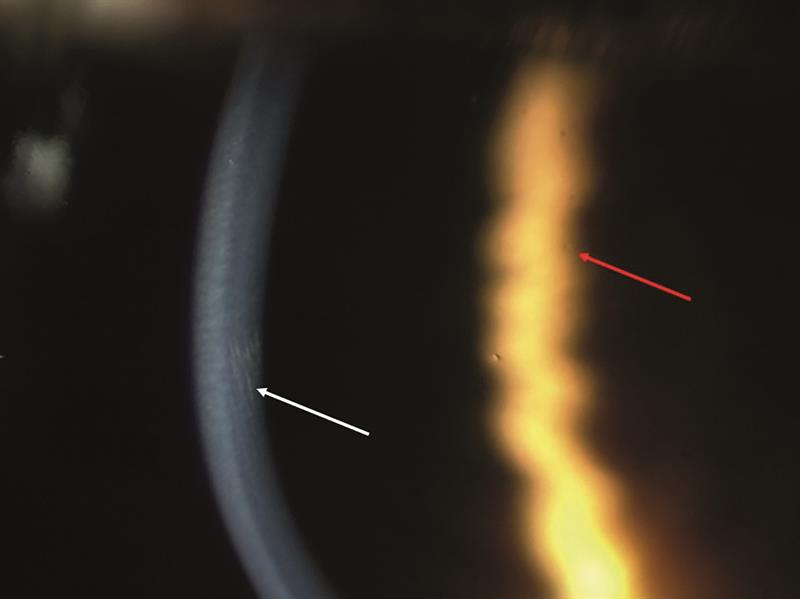 Striae (left) and microcysts (right)
Striae (left) and microcysts (right)
Management
To reflect the split in your views, have a look at these two responses.
‘We are always encouraged by the contact manufacturers to “upgrade” our patients with the newer products, and many of the sales reps do not comprehend the old phrase; “if it ain’t broke, don’t fix it.” Therefore, I would be quite happy to leave this patient in their existing lenses.’
‘I would definitely change the patient to a silicone hydrogel daily disposable lens. Of course, there would need to be checks on the tear film suitability and meibomian function, to ensure there were no other contraindications. However, I feel that, for patients wearing lenses on a full-time basis, the levels of oxygen are extremely important and it may be that there is subclinical hypoxic stress over many years. The difference in blood perfusion at the limbus is very obvious on the slit lamp between a SiHy and a hydrogel. I think it likely that this patient would have fewer problems in the future with the health of his cornea if the cornea obtained the maximum oxygen requirements possible. While one cannot say one structure of the eye is more important than another, the cornea, being avascular, may not have the same ability to recover from side effects of contact lens wear as perhaps the eyelids. Having worn soft lenses for almost 40 years and tried nearly every type of lens available, and also having experienced the serious red eye reaction from falling asleep in the original soft lenses of the early 1980s, I do feel my personal experiences have shaped the way I prescribe lenses.’
Patient Discussion
Not surprisingly, the approach to patient discussion reflected the 50/50 divergence in your management approaches. For every response like this: ‘I would discuss with the patient the benefit to the cornea of obtaining the maximum oxygen levels possible and how this may possibly allow him to wear contacts for more years without complications.’ There was another one like this: ‘I would inform the patient that their current lenses are performing well and their eyes are healthy. I would emphasise the need for regular aftercare checks, as the situation may change in the future.’
I suspect this debate has plenty of life left.
- Look out for further discussion and associated CPD exercises on each of the two interactive Essential Contact Lens exercises in the coming months
References
- Ruston D, Meyler J. Why hydrogels? There is more to contact lens performance than Dk/t. Optician, 06.09.2019, pp24-26
- Hogan C et al. Why Si-hi? Optician, 05.07.2019, pp28-32
