
The assessments of visual fields in a low vision setting is an important part of assessing vision. No longer is the test aimed at disease detection, though obviously changes to visual fields are always a useful indicator of disease progression, but rather a way of assessing the potential impact of any loss of field upon function. It then makes it easier for the eye care practitioner to decide on any particular management strategy, such as help with mobility or addressing the way a person’s home environment is set up.
Furthermore, the loss of visual field is often a key factor in the decision as to whether a consultant ophthalmologist is likely to certify someone as eligible for registration as either sight or severe sight impaired. Unlike acuity values, where specific values are cited as guidance, the loss of field and the impact of significant glare or photophobia are left much more to the discretion of the clinician in deciding upon their likely impact upon life and therefore eligibility for certification. Bilateral hemifield loss is usually considered sufficiently severe to warrant registration, while major encroachment upon the inferior field of each eye is also thought to have a great enough impact upon mobility to also pass any requirement.
In many cases in low vision, especially on domiciliary assessments, gross perimetry has more often than not been the mainstay of assessment. Though the accuracy and sensitivity of using a small ball on a stick my not be great, often its portability, ease and speed of use and the ability to detect large areas of loss are more than enough to justify its use. Particularly when the main aim is to assess the extent of significant field constriction, or to identify whether any lesion with the potential to affect the visual pathway has affected vision.
Ocular or Visual Pathway
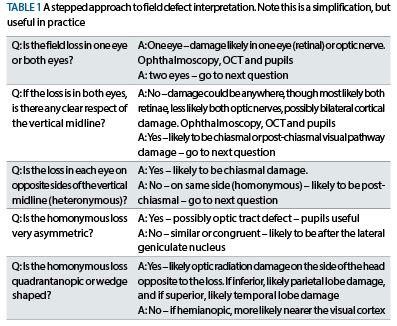
Though this subject was comprehensively covered in a recent CET article (see Optician 09.08.2019), it is always worth remembering a few basic rules regarding field defect interpretation as outlined in table 1.
Determining field loss relative to the vertical midline is essential in discovering the extent of neurological damage, and for this it is sometimes only gross perimetry that can be available. For example, a patient may have severe neurological deficit, say cognitive or learning impairment, or may have some element of confusion that makes a more in-depth approach impossible. It may even be a baby. Being able to direct attention to a target presented suddenly in one half field and not the other on repeated occasions can be a useful finding and is always worth trying.
I have been interested in seeing if the new Thomson Digital Visual Fields Screener (figure 1) has any benefit when assessing low vision patients in the domiciliary setting. Here are two recent cases where, previously, I would have relied solely on gross perimetry and where having a degree of increased accuracy offered by a computerised test paid dividends.
Case 1
A significant number of patients who suffer a cerebrovascular accident (or stroke) have field loss, most typically homonymous loss. Patient SC was a 62-year-old who had recently suffered a stroke and had been referred to our clinic by the stroke team for a home visit low vision assessment. As well as discovering an all-too-common level of uncorrected ametropia which immediately gave the patient noticeably improved vision of her surroundings, her mobility (observed as she negotiated her hallway and showed us to her living room chair) was slow, careful and unsteady. Some loss of left-sided motor function suggested left temporal lobe damage and this might also show itself in a left homonymous loss or reduction in vision.
Importantly, whenever gross perimetry was tried, SC was absolutely unable to maintain fixation on my face and here eyes darted around to wherever she thought the target might be, whether correctly or no.
When using the basic screening strategy of the Digital Visual Fields Screener, it soon became clear that there was some deficiency of her ability to see targets in the left side of her field in each eye. This appeared to be due to two factors which allowed me to achieve this result, albeit a less than fully reliable one.
• The fixation target for the patient when using the screener is initially a small white cross (figure 2a) which expands and so maintains attention with good stability.
• Once the cross changes to a small red cross (figure 2b), multiple stimuli are presented. When these were either side of the vertical midline, only one was seen on a significant enough number of occasions to warrant suspicion of hemifield loss. Though fixation was poor, and the patient was always tempted to move their gaze to the flashed light they had seen, the consistency of the side to which they moved their fixation was useful.
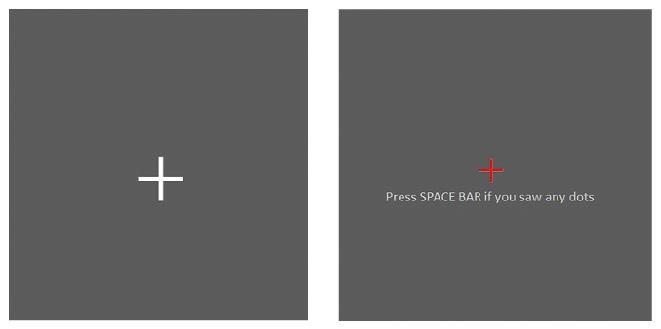 Figure 2 (a): Growing white cross followed by (b) red cross fixation target on the Digital Visual Fields Screener
Figure 2 (a): Growing white cross followed by (b) red cross fixation target on the Digital Visual Fields Screener
Along with the optical and ocular status report, a suspicion of the homonymous loss was also included in the report back to the stroke team and a future appointment at the hemianopia clinic was made.
As an aside, people with homonymous hemifield loss who read English-style text tend to be more greatly affected when their
loss is on the right-hand side as this is the direction they would normally scan into when reading. Often, a steady eye strategy approach is then indicated for future reading training. I have also noticed that an audio-signal text (as might be available on, say, a Kindle) also is useful in the first months of reading rehabilitation.
Case 2
Initial field defects in retinitis pigmentosa are often of an eccentricity (50 to 60 degrees) that fall outside the range of a typical central visual fields’ analyser. Greater encroachment, as might be expected in the case where this represents a major impact on viewing and might influence registration, should be detectable in the more central field.
Such a case presented recently where previously only gross perimetry had been performed. Most automated peripheral field analysis requires instrumentation unsuited to the domiciliary environment (such as the Goldmann or the Octopus).
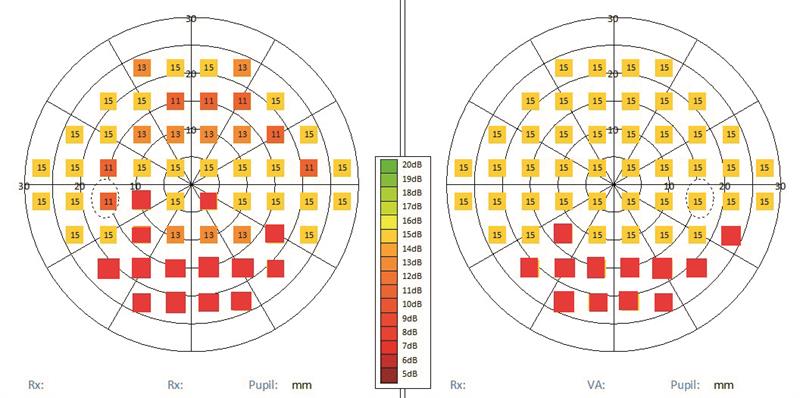 Figure 3: Simulated field loss showing bilateral inferior constriction and a left superior paracentral loss.
Figure 3: Simulated field loss showing bilateral inferior constriction and a left superior paracentral loss.
Being able to detect (albeit again with poor reliability) the extent of inferior loss while also assessing superior retinal fibre bundle defect loss in the left eye (as represented in the simulated field plot shown in figure 3) gives useful information for future monitoring of change in the home environment that gross perimetry might be too insensitive to detect.
