There are currently five accredited optometry programmes in Australia and one in New Zealand located in Adelaide, Brisbane, Geelong, Melbourne, Sydney and Auckland. Each programme is accredited by the Optometry Council of Australia and New Zealand (OCANZ) that performs a similar role to the General Optical Council (GOC) by monitoring and setting standards of education.
One major difference is that professional registration of student and practicing optometrists is overseen by a central government agency known as the Australian Health Professional Regulation Agency (AHPRA) that works with the national boards of registration such as the Optometry Board of Australia to ensure that optometrists meet the required professional standards. AHPRA performs this role with optometry along with several other health professions such as: doctors, dentists, nurses, occupational therapists, radiographers, pharmacists, psychologists and chiropractors. In this way, AHPRA is able to ensure that only health practitioners who are suitably trained and qualified to practise are registered.
Flinders University
There is a wide range of final optometry degree classifications offered by each program with courses running between 3.5 to five years at the different institutions depending on whether a two or three semester teaching pattern is used. At Flinders University, the program is five years and students graduate with a double degree of Bachelor of Medical Science (Vision Science) and Master of Optometry.
Upon completion of the university optometry program, all graduates are eligible to apply for registration with AHPRA having completed clinical and therapeutic training within the program of study. Optometrists are eligible to prescribe a range of therapeutics to manage ocular disease in Australia (table 1) which has similar scope to the range of therapeutics available to independent prescribing optometrists in the UK.
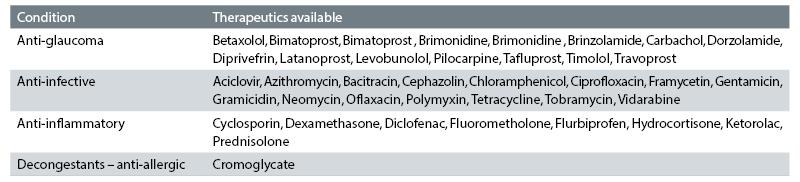
Table 1: List of therapeutics currently listed in the Optometry Pharmaceutical Benefits Scheme (accurate as of August 2017)
To provide clinical experience, Flinders University provides students with the opportunity to experience a wide range of clinical settings throughout Australia. Flinders has a network of placement partners that take students for periods of six weeks and encompass practices located in metropolitan and rural/remote locations with each student having the opportunity to experience independent, hospital and corporate environments.
The placement program is modelled on the pre-registration period for UK optometrists with students seeing approximately 500 patients across 18 months of the program. Students may also take placements in Nepal and China as well as Boston. Figure 1 shows Flinders students carrying out sight tests in Nepal as part of their clinical training. Their final clinical competence is assessed within the university and not by an external body such as the College of Optometrists in the UK.
Teaching and learning
The Flinders optometry program saw its first graduates in 2014 and the students have benefited from undertaking a program of study that was developed without the need for didactic lectures and instead incorporated a variety of teaching strategies to deliver teaching and learning. The main strategies involve a blend of on-line e-learnings that are able to deliver customised content relevant to the teaching area that the students can access in their own time.
Supplementing the e-learnings are case based learning, team based learning and inter professional education alongside self-reflection and peer review. Students also examine patients that present to Flinders Vision public optometry clinic as part of their clinical placements. Clinical episodes at Flinders Vision are recorded to enable the students to review and critically evaluate their interaction with the patient. Figure 2 shows the Flinders Vision Clinic.

Figure 2: Flinders Vision public clinics
Case based learning
Case based learning (CBL), also known as problem based learning, has been central to the program from its inception to deliver clinical case based scenarios from which the students learn to synthesise information and develop a differential diagnosis and management plan for each case.
The CBL tutor facilities the discussion of the case to small groups of students (typically seven to 10). The role of the tutor is not to teach but to act as a guide and ensure all students participate in the discussion across three tutorials per case. During the first three-hour tutorial students develop three key elements during the initial delivery of the case history:
- Hypothesis: What could this be? – The students develop a list of possible diagnoses based on the information presented about the case.
- Tests: The students develop a list of tests and further questions that they think will help them determine the most likely diagnosis.
- Learning Objectives (LOs): Students will be presented with terms or questions for which they do not know the answer during the case delivery. These unknowns become the LOs and the basis for their self-directed learning that the CBL tutor highlights. In order for the students to solve the case, they must find answers and understand concepts by themselves. In this way, the students are motivated to learn as they can see the relevance of the information for helping them to manage and understand the clinical presentation.
During the second three-hour tutorial the students report back on the preceding LOs developed in the first tutorial and the case develops further leading to more questions and LOs for the students to find answers to. In the final tutorial, the students again report on the second set of LOs and the case is closed by the tutor.
By using a real-life case with relevant clinical findings to present clinical, legal, therapeutic and optometric tests as a cohesive interactive unit, the students learn to think in a cohesive manner rather than learning in a modular style. A typical case might be a 20-year-old myopic female patient who presents complaining of dry eye and difficulty seeing at night. The case results in an exploration of inherited retinal dystrophies with discussions around retinal physiology, visual electrophysiology, genetics and counselling. The dry eye symptoms are secondary to the use of the contraceptive pill.
Team based learning
Team based learning (TBL) has been recently introduced to the Flinders Optometry program. This style of teaching randomly places students in small teams of five to six students for the duration of the topic. TBL involves ongoing assessment in which the individual and team performance counts and this motivates the students to learn for themselves and ‘for their’ team.
Students are given some preliminary reading and/or e-learnings, which they study ahead of the TBL session. When they arrive in class they perform an individual test based on the preliminary reading they have been set. Then the team takes exactly the same test but this time they can discuss their answer within the team. However, each incorrect attempt is penalised and as each individual in the team gets the final ‘team score’ for this component it encourages discussion about why some students chose perhaps answer A and others answer B.
There is also peer on peer evaluation of each individual’s performance within the team that contributes to the students’ final grade. This encourages students to be an active part of the team through contributions to the team quiz and/or problems in class.
The remainder of the class is spent providing the teams with problems to solve that may last 10 minutes. Teams present their findings and can be challenged by other teams, which provides an opportunity to discuss concepts and understanding of the material. TBL aims to develop teamwork and helps students learn to be a part of a team to solve a problem.
Evidence based practice
Central to the core teaching values at Flinders is for students to appreciate the quality of evidence to enable them to practice according to the best evidence. Students present summaries of systematic reviews for discussion by their peers in their final year as part of their research project. In the third year of the programme students have weekly debates on contentious optometry topics and critically analyse the recent literature to help them understand that sometimes the answer is not black or white and that being a critical thinker and being able to appraise the value of evidence is an essential aspect of professional life.
Inter-professional education (IPE)
The model for IPE is formed around the development of a patient case that involves the care and management of multiple professionals. In optometry two scenarios, being developed with the support of allied health professionals that focus on an elderly lady who has a fall due to her spectacles and fractures her hip requiring input from paramedics, occupational therapists, optometry, and nursing to manage the patient’s care and rehabilitation.
The second scenario involves an Aboriginal woman who has a car crash and delivers a pre-term infant away from her native land which develops retinopathy of prematurity and consequently provides the scope for the involvement of a wide range of professionals to manage the mother’s and child’s physical and psychological wellbeing. This mode of teaching removes students from the lecture theatre and tutorial room and is presented by actors and through on-line resources to the students from the professions. The main aim of IPE is to develop the students understanding of the role and expertise in managing a patient.
Australia versus UK
The optometry graduates from Flinders are exposed to a greater range of clinical cases and are expected to be able to manage cases using therapeutics. Diagnostic techniques, such as binocular indirect ophthalmoscopy and gonioscopy, are a part of the core clinical training.
There is undoubtedly a greater emphasis on students, undertaking self-directed learning through CBL and TBL exercises rather than material being delivered by lectures. The development of greater autonomy on patient management in Australia is partly driven by the need to provide eye care across a large area where ophthalmologists are sparse. Consequently, optometric graduates need to be ready to work independently and with confidence in their clinical decision making as part of a team.
The Flinders optometry program has grown with help from allied health professionals and using CBL and TBL has encouraged students to work together on problem solving and also the independence to search and appraise the value of evidence in order for them to develop as professionals who are lifelong learners.
Dr Paul A Constable is senior lecturer, Flinders University, and a former lecturer at City University London.
