The use of preloaded intraocular lens (IOL) implants are on the increase. However, IOLs of lower or higher dioptric value and certain premium lens implants still need to be loaded manually. This study has been carried out to identify if touch marks have any adverse effects on visual function
Background
Marks on the optic of an intraocular lens can occur when loading the lens with forceps. Later, at post-operative assessment, patients may be misinformed by optometrists that they have a faulty lens. In some cases, this can result in the patient requesting explantation of the intraocular lens or lens exchange.
There is currently no information available to assess the outcome due to marks on the optic following loading, particularly relevant in new multifocal intraocular lens which rely on the refractive differences in the lens material between different parts of the optic.
There are previous case studies which assess deposits on acrylic lenses. One such study, where the visual outcome following cartridge injection of an acrylic lens with deposits was assessed, found these deposits did not seem to adversely impact upon the visual outcome and the patient was left with good vision.1
There have also been case reports of patients presenting with a crack in the optic of a single piece intraocular lens where good visual acuity (6/6 Snellen) was maintained following recovery.2
However, there is currently no information on the visual outcome on optic marks created when manually loading multifocal lenses. The aim of this study was to identify if physical contact with the optic of an intraocular lens while loading resulted in an adverse visual outcome.
Methods
This was a retrospective case series study. In total, 970 patients received cataract surgery over the study period. Twelve patients had a mark on the optic of the intraocular lens following their surgery. The patients with a mark on the optic were identified in the first post-operative visit (figure 1).
Figure 1: Post-operative marks on the IOL relating to manual positioning during surgery
Eleven of the 12 patients had undergone cataract surgery in both eyes (not simultaneously). Therefore, the fellow eye without IOL marks could be used as a control to compare vision and symptoms. One patient had had only one eye operated on. Glare symptoms were divided into three grades:
- Mild
- Moderate
- Unbearable
Results
Of the 12 patients identified on their first post-operative visit to have a mark on the optic of the intraocular lens, five were female and seven male. The average age was 53 years (range 46 to 64 years). Four patients had a mark from the forceps on the centre of the optic and eight patients had a mark on the paracentral axis. There were 10 fine vision trifocal intraocular lenses (hydrophilic acrylic IOLs) and two patients with the AMO Symfony multifocal lens implanted.
The pre-operative refraction range was -1.00DS to +2.75DS (figure 2) with a mean of 1.32DS and a standard deviation of 1.33DS. The post-operative results of these patients were good with a post-operative refraction range of -0.25DS to 0.00DS, with a mean of 0.03DS and standard deviation of 0.19DS (see figure 2).
The pre-operative best corrected visual acuity range was 0.5 to 0.0 logMAR with a mean of 0.1 and a standard deviation of 0.16 logMAR. The post-operative average acuity was 0.15 with a standard deviation of 0.11 logMAR (see figure 3). 66.7% achieved a visual acuity of 0.2 logMAR or better. All 12 patients achieved near vision of N6 or better.
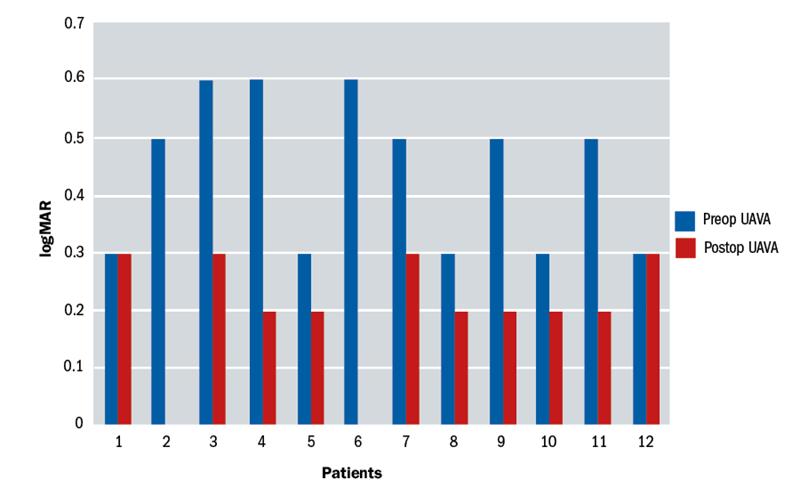
Figure 3: Pre and post-operative unaided vision (in logMAR)
One patient complained of dysphotopsia. However, the mark from the forceps was on the nasal aspect of the lens and this did not correlate with the symptoms described by the patient. All other 11 patients were asymptomatic. No patients had worse night time glare in one eye compared to the other.
Discussion
Calcification and opacities on the optic of intraocular lenses is well described and can occur due to manufacturing methods, surgical techniques and lens design variations as well as discolouration through dyes or silicone oils.3 There is currently only limited information to evaluate the effect of optic marks or opacities on multifocal lenses and their impact upon visual outcomes. This study showed that marks on the optic of intraocular lenses are uncommon, with a low incidence of 0.01 (12 out of 979). Furthermore, the overall post-operative visual outcomes were not adversely affected by these marks.
Patients may be told they have a mark on their IOL when reviewed post-operatively by an optometrist. However, these patients should be reassured that such a mark will not adversely affect their vision. It is important to manage patient expectations, and not to readily associate visual symptoms with a mark on the optic as there may be other underlying pathology resulting in decreased vision or visual symptoms.
Navpreet Dhillon is a Corneal Fellow at St George’s and Moorfields Eye Hospital and Balasubramaniam Ilango is Medical Director Optimax/Ultralase Clinics, UK and a consultant ophthalmologist, Wolverhampton Eye Infirmary.
References
1 Marcovich AL, Kleinmann G, Epstein D, Pollack A. The course of surface deposits on a hydrophilic acrylic intraocular lens after implantation through a hexagonal cartridge. Br J Ophthalmol. 2006 Oct;90(10):1249-51
2 Balasubramanya R, Rani A, Dada T. Forceps-induced cracking of a single-piece acrylic foldable intraocular lens. Ophthalmic Surg Lasers Imaging. 2003 Jul-Aug;34(4):306-7. PubMed PMID: 12875459.
3 Werner L. Causes of intraocular lens opacification or discoloration. J Cataract Refract Surg. 2007;33(4):713-726.
