Last month, in a CET article looking at advances in intraocular pressure measurements, Dr Daniela Oehring explained how being able to measure intraocular pressure continuously over a 24 hour period ‘allows the eye care specialist to assess the effectiveness of any prescribed glaucoma treatment, allowing both the patient and the doctors to benefit from individually tailored therapy. It has been shown that 24-hour IOP monitoring results in an immediate treatment change in approximately 40% of the patients and a general clinical management change in about 80% of cases.’1
Traditionally, continuous IOP monitoring (or phasing) required a patient to repeatedly visit or stay within a clinic facility to allow measurements to be made. Obviously, this had implications of cost, convenience and compliance. More recently, three devices have been introduced that allow phasing to be undertaken remotely, so avoiding these problems.
The iCare Home
The iCare Home is a rebound tonometer (so requiring no anaesthetic) that has been available in the UK for around four years. The instrument is held before the eye by the patient (figure 1) and presses a button to fire the probe at the cornea either as a single or cluster of six firing mode. The IOP data calculated is then stored and can be accessed remotely by the clinician.
A 2017 study2 compared iCare Home measurements undertaken by 130 glaucoma patients with those of an ophthalmologist using either the device or Goldmann Applanation Tonometry (GAT). With training, 98% of patients were able to use the iCare properly. The investigators found that the iCare Home tonometer demonstrated a tendency to capture higher IOP values than GAT overall, but deemed it feasible for self-monitoring IOP.
Obviously, there were significant gains in convenience and reduced clinic access demands. However, many experts argue that for accurate phasing, IOP should be monitored over the entire 24 hour period, including periods when the patient is asleep and in a supine position. This is not possible with this instrument.
The Sensimed Triggerfish
The Triggerfish contact lens sensor is a soft, single-use contact lens available in three base curves (8.4, 8.7, and 9mm), measuring 14.1mm in diameter and 585µm thick in the central zone (figure 2). The system incorporates two strain gauges, a microprocessor, and single-use adhesive that fits around the patient’s orbit and holds a receiver antenna. There is also a disposable recorder sleeve for the microprocessor. Fitting requires two appointments, one to apply the Triggerfish and one to remove it, usually after a wearing time of at least 24 hours.

Figure 2: The contact lens component of the Sensimed Triggerfish
Normal daily activities are encouraged during the period of wear, though anything causing excessive sweating can loosen the adhesive holding the antenna in place. The most commonly reported side-effect is a red eye and slightly blurry vision as the contact lens has no optical correction. Artificial tears can be used if the eye feels dry or scratchy, and most reports suggest that the contact lens is well tolerated by the patient during the monitoring period, accepting the expected levels of discomfort and awareness from such a device.
The Triggerfish lens captures 30 seconds of data at five-minute intervals over each 24-hour period of wear. During this time, the contact lens is not actually measuring IOP as such. Instead, it acts like a strain gauge and is able to detect and measure differences in strain at the surface of the eye. So, rather than an IOP value in mmHg, the Triggerfish records levels of fluctuating strain of the eye in millivolts. For this reason, some authorities have dubbed the technique ‘strain tonometry’.
Many studies in recent years have evaluated the device. One, back in 2016 showed that IOP-related measurements from the Triggerfish correlated well with the progression of glaucoma in a group of patients being treated for the disease.3 The contact lens measurements were able to predict the relative rate of progression of the disease for the patients which would be useful in tailoring ongoing treatment. The researchers pointed out that, because the Triggerfish is measuring more than just the eye’s internal pressure, these measurements may be a more accurate reflection of the susceptibility of an eye to suffer from glaucomatous progression in the future.
A more recent study has concluded: ‘The Triggerfish can detect changes in patterns resulting from IOP-lowering interventions beyond daytime GAT IOP. This device could potentially be used to assess treatment efficacy in glaucoma.’4
One study of note has used the Triggerfish in people undertaking a range of yoga positions and found that there are significant spikes in IOP for certain positions where the head is held downwards.5 This has led clinicians to advise glaucoma patients against specific yoga positions, though how big a target group this is I am not sure.
The Eyemate
Recently introduced in Europe, the Eyemate is an implantable device intended for continuous, long-term IOP monitoring. A flexible, ring-shaped sensor 12mm in diameter is designed for sulcus implantation at the time of cataract surgery through the surgical incision (figure 3). The Eyemate is positioned in front of the intraocular lens and behind the iris and, according to the manufacturer, has minimal impact upon vision.
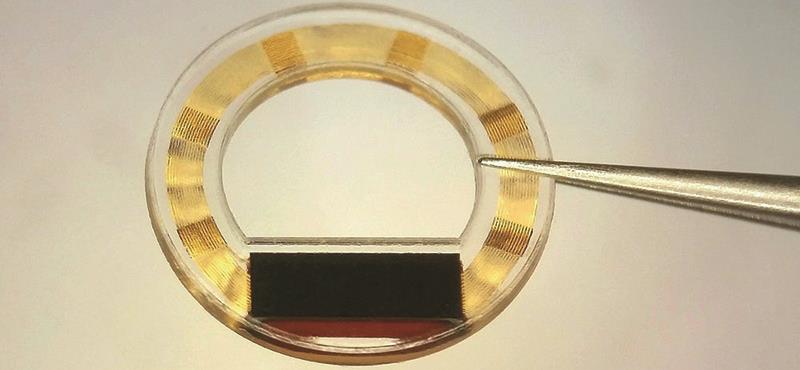
Figure 3: The implantable Eyemate IOP measuring device
The data measured within the eye by the implant is transmitted to a small hand-held mesograph periodically held by the patient close to the implanted eye. The mesograph, which is about the size of a small smart phone, displays IOP measurements and stores them. When fitted with a GSM module, the Eyemate can also transfer measurements to an internet database to share round-the-clock records with the ophthalmologist.
The first Eyemate was successfully fitted in 2018 as part of the ARGOS-SC01 clinical study which is currently being extended across Europe and the results of which are keenly anticipated by the glaucoma community. The manufacturers have about five years of data showing that the device stays in the eye, is well tolerated, and is safe over the long term.
The future
The results from each of these devices, different as they are, confirm that continuous monitoring of IOP is now a realistic prospect. I believe it will not be too long before eye care practitioners in the UK will have access to such data and that this will prove a real boon for glaucoma monitoring.
References
1 Oehring D. Advanced examination techniques for the anterior eye – part 2. Optician, 01.02.2019.
2 Takagi D, Sawada A Yamamoto T. Evaluation of a new rebound self-tonometer, Icare HOME: Comparison with Goldmann applanation tonometer. J Glaucoma 2017;26:7:613-18.
3 De Moraes CG, Jasien JV, Simon-Zoula S, et al. Visual field change and 24-hour IOP-related profile with a contact lens sensor in treated glaucoma patients. Ophthalmology 2016;123:4:744-53.
4 Cutolo CA, De Moraes CG, Liebmann JM, Mansouri K, Traverso CE, Ritch R; Triggerfish Consortium. The Effect of Therapeutic IOP-lowering Interventions on the Twenty-four Hour Ocular Dimensional Profile Recorded with a Sensing Contact Lens. Journal of Glaucoma, January 2019. www.ncbi.nlm.nih.gov/pubmed/30640804
5 Jasien, JV, Jonas JB, de Moraes CG, Ritch R. Intraocular pressure rise in subjects with and without glaucoma during four common yoga positions. Plos One 2015; https://doi.org/10.1371/journal.
