
During nearly a year of practising in a pandemic, debate around remuneration of general ophthalmic services (GOS) in England has been constant.
Instead of being a topic that cropped up annually around fee negotiation time, GOS has become a subject of never-ending debate between the Optometric Fees Negotiation Committee (OFNC) and NHS England.
In April 2020, GOS fees in England were frozen by the Department of Health and Social Care (DHSC) for a fifth successive year despite the OFNC bidding for an increase of 2.4%, which it said was in line with wider investment in NHS care.
The DHSC cited the lack of evidence about any impact on NHS sight test numbers or optical businesses as its reasoning for freezing the fee again.
Covid-19 has raised questions over support for optical practices and many have considered ending GOS services, with the pandemic acting as the final push to make the move to private care only.
With a private eye care model in place, optical practices believe they can become more financially viable while providing a higher standard of eye care through more appropriate fees and patient care plans.
However, there are practitioners who believe the pandemic has created an opportunity for the profession to highlight its value to NHS England and capitalise on the urgent need to alleviate pressure on the NHS.
For some, GOS is the foundation to extended eye care services and closer collaboration with colleagues in ophthalmology, which leads to a better standard of care being provided to patients while maintaining access to NHS care.
Remuneration of services
In recognition of this divide, Optician decided to survey eye care practitioners to find out if they had considered ending NHS services at their practices and to establish what the future of GOS looks like.
A total of 1,641 optical professionals responded to Optician’s Future of GOS survey and results highlighted a clear majority over the importance of GOS and close results over whether to stop providing NHS services.
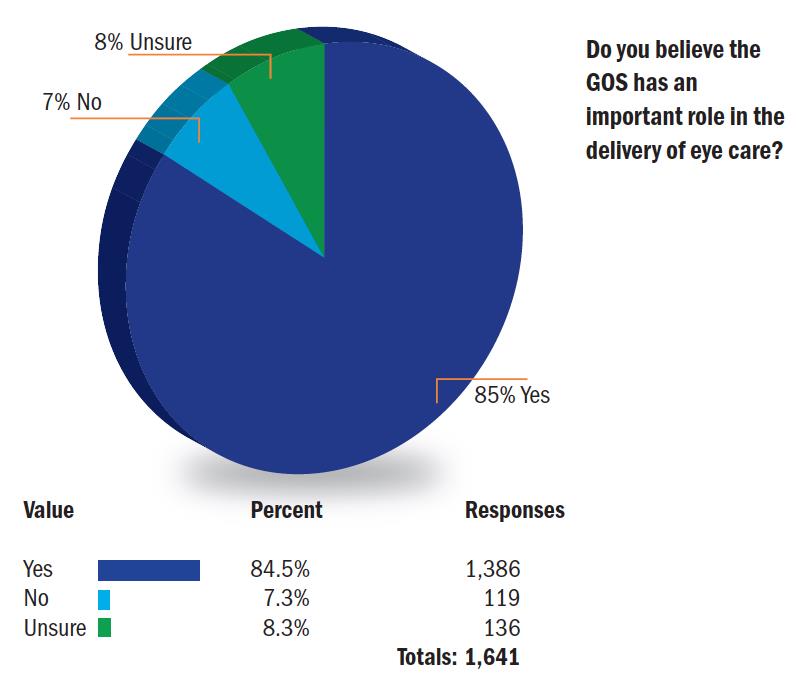
When asked if GOS had an important role in the delivery of eye care, a total of 84.5% (1,386) said yes, while there were more respondents who were unsure (8.3%, 136) than those who said no (7.3%, 119).
However, when asked if the level of eye care available through GOS adequately met patient needs, 60% (984) said no, 28.6% (470) of respondents said yes and 11.4% (187) said they were unsure.
Practitioners were predictably in agreement about remuneration of NHS services, with 87.5% (1,436) of respondents who said it was not sufficient, while 6.5% (106) said it was and 6% (99) were unsure.
A large majority (70.5%, 1,157) said that GOS required too much time and administration, with 20.5% (337) who said no and 9% (147) unsure.
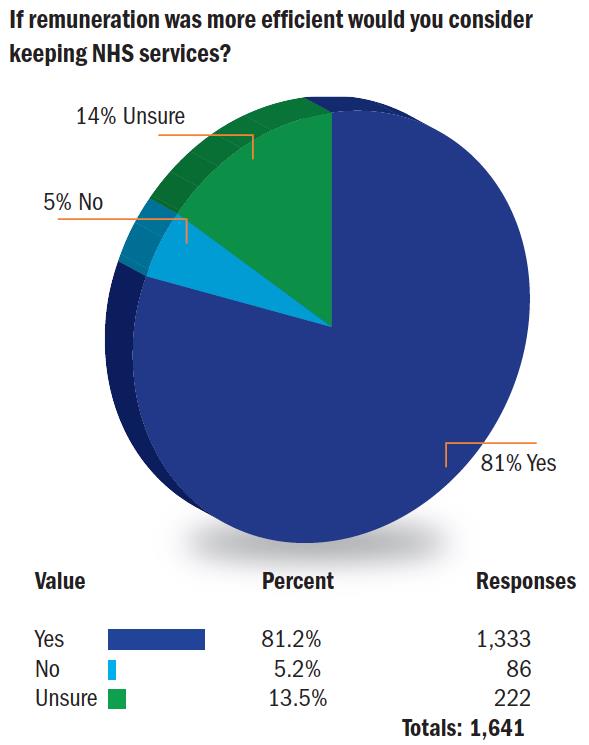
When asked if practitioners would consider keeping NHS services if remuneration was more efficient 81.2% (1,333) said yes, 5.2% (86) said no and 13.5% (222) were unsure.
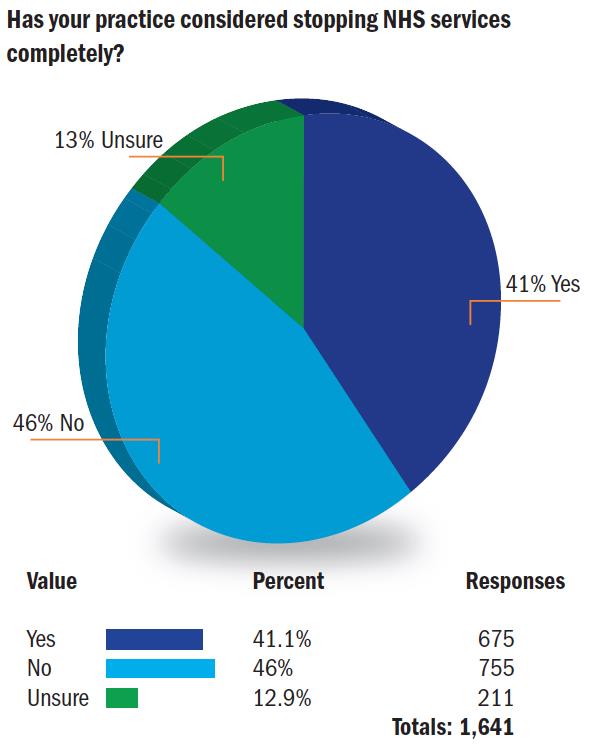
Respondents were relatively split when asked if their practice had considered stopping NHS services, as 46% (755) said no and 41.1% (675) said yes, while 12.9% (211) were unsure.
A total of 71.2% (1,169) said yes when asked if there would there be a brighter outlook for NHS eye care if more hospital services were delivered by community optometry practices – 17.3% (284) were unsure and 11.5% (188) said no.
When asked if a closer working relationship between primary and secondary care needed to be formalised, 88.4% (1,450) said yes, 7.6% (124) were unsure and 4.1% (67) said no.
Chronic underfunding
Optician shared the survey results with the OFNC and asked for its response to the findings, what it thought needed to happen to secure an increased rate of remuneration and how it expected practices to respond if the rate did not change.
Paul Carroll, chair of the OFNC, said Optician’s survey results reflected matters that it had discussed with NHS England for some time.
‘The survey supports our argument to NHS England and DHSC that chronic underfunding of GOS services has put many practices under great financial pressure and risks reducing patient access to NHS eye care.
‘We have made these and other risks consistently clear to NHS England and the DHSC and continue to do so. The pandemic has shown just how vital primary eye care is in meeting eye care needs and keeping pressure off GPs and hospitals.’
Carroll added that the OFNC’s current priority was to support the sector through the pandemic and that it had worked with NHS England to secure grant funding for primary eye care to support services continuing in line with government requirements and to preserve the vital primary eye care infrastructure.
‘We continue to track the impacts of the pandemic and to make the case for further support where necessary. Alongside our work to secure Covid grants, the OFNC has continued to press NHS England on the absolute level of sight test fees in the context of 2021-22. We have put in a bid for an increase in GOS fees in 2021/22 and are waiting for a decision which ultimately lies with Ministers on the advice of NHS England,’ he said.
Vital eye care
When Optician shared the survey results with optometrist and chair of the Association of Independent Optometrists and Dispensing Opticians (AIO), Dr Christian French said he was not surprised by the findings as it has long been the case that the GOS has not properly remunerated optometrists in England for providing vitally important eye care services.
French commented: ‘What NHS England should take on board from the survey is that the clear majority of practices say the level of eye care available through the GOS is inadequate, but equally the NHS should be encouraged that the overwhelming majority of practices wish to continue to provide NHS services if these current short-comings and issues are addressed.’
He highlighted the AIO’s Covid-19 manifesto set out the approach that the profession should take with NHS England to reform the provision and delivery of primary eye care in England, complete with appropriate remuneration.
‘The current pandemic has highlighted the crucial role that community optometry can play in the delivery of primary eye health care and now is a unique opportunity in which to change the landscape for the delivery of eye care for the better; with greater efficiencies and utilisation of skilled workforces.
‘Being one of the few subjects where our profession seems largely of the same opinion, it behoves all representative and professional bodies to set aside any minor differences and competing interests to present a common and compelling proposition for NHS England to buy into.’
French added that the profession and the public only need to look at dentistry to see the alternative trajectory if nothing is done to address these issues. He said it would result in those in greatest need of NHS support struggling to find a provider and facing waiting times to become a patient in a two-tier system of services.
‘Good quality eye examinations should be available to all and NHS England must take stock of polls such as this and initiate the necessary changes now before the opportunity is lost. The AIO manifesto advocates a completely different approach. It is time for meaningful and reforming change,’ he concluded.
OFNC updates on GOS
‘We reported in our statement of January 8 that the OFNC was in urgent discussions with NHS England about potential additional support for optical practices affected by the new restrictions. We have proposed potential models for this to NHS England and discussions are ongoing.
This week NHS England were able to share with us the GOS claims data for January 2021, which are a combination of real-time eGOS claims and paper claims. Taken together they suggest slightly lower overall GOS activity in January 2021 than in January 2020. Although this is a broad-brush picture based on aggregate data, we accept that the trend over the 10 months since the pandemic hit does not provide a strong case for generalised Covid-19 support across all GOS contractors at this point.
However, many practices have contacted OFNC member bodies calling for help as they are suffering a sharp downturn in demand for face-to-face care. This is because of the current restrictions, the government’s strong ‘stay at home’ messaging and the prospect of vaccination encouraging people to postpone care. Some are reporting activity at 50% or less of the usual level for January.
We are therefore urging NHS England as a matter of urgency to put in place some targeted, short-term financial support for practices experiencing a significant downturn in face-to-face activity and struggling to remain operational. We will provide a further update as soon as we can.
In the meantime, we are pleased the Covid-19 vaccination roll-out for patient-facing staff in optical practices and domiciliary providers is making good progress. Any GOS contractor experiencing difficulty in arranging vaccinations for their staff should contact their Local Optical Committee for assistance in the first instance.’
