Sheraz Daya outlines a new approach to refractive surgery and describes his experience with the technique
IntraLase, the femtosecond laser in commercial use, is now available at Centre for Sight in the UK, one of only 166 of such lasers worldwide. It is futuristic technology that promises to revolutionise corneal surgery.
 |
| Figure 1. Raster pattern of separation commences at the hinge |
The IntraLase femtosecond laser has an extremely short burst duration - less than one quadrillionth (10-15) of a second. To put this in perspective, light, which can travel around the earth seven times in one second, would barely traverse a human hair in one femtosecond. This solid state laser operates in the infra-red wavelength range (1053nm) and, using a spot size of 3µm, (less than half the size of a red blood corpuscle) produces photodisruption at a precise and predetermined level within the corneal stroma. The laser produces cavitation bubbles consisting of water and carbon dioxide and these placed next to each other result in separation of the corneal stroma. Spots can be placed at any level in the cornea and using computer software these can be placed to achieve corneal separation in three dimensions. The laser treatment is delivered through a glass plate applanated on the corneal surface and held on the eye by a low-pressure suction ring. The spots traverse the cornea in one of two ways: a raster pattern, where spots travel in a horizontal line back and forth (Figure 1); or a spiral pattern, where the spots start centrally and spiral out (Figure 2). Presently the IntraLase femtosecond laser has three applications - flap creation for Lasik, corneal channels for Intacs and Ferrara intracorneal rings, and lamellar keratoplasty.
 |
| Figure 2. Sequential images showing a spiral pattern of separation commencing at the centre spiraling out (used in lamellar grafts) |
LASIK FLAPS
Flap creation is the most common use of the laser. A raster pattern is used to create a circle of separation horizontally at a predefined diameter and once accomplished a circumference cut is used, leaving a gap for the hinge. The location and width of the hinge, depth and width of the flap are all defined by the user.
The flap created by IntraLase differs from those created by keratomes in many ways. Keratome-generated flaps are highly variable in corneal thickness1,2 and on occasion a thicker-than-desired flap can occur, as demonstrated by the author's group.3 A thicker-than-expected flap not noticed by the surgeon can lead to corneal ectasia following Lasik. Flaps generated by keratomes vary in thickness and are lenticular in shape, being thicker in the periphery and thinner in the centre. Sometimes keratomes can produce buttonholes, especially in steep corneas. Steep corneas (>47.00D keratometry) are prone to prolapsing away from the blade centrally, resulting in no cut. This can lead to severe long-term problems, including irregular astigmatism, scarring and epithelial in-growth. The variability of keratome flap thickness can theoretically lead to induced astigmatism and some unpredictability in refractive outcome. This finding has been demonstrated in a comparative study.1
 |
| Figure 3. Lasik flap anatomy: Microkeratome vs Intralase. Planar cut confirmed on flap histology (Courtesy of L Probst) |
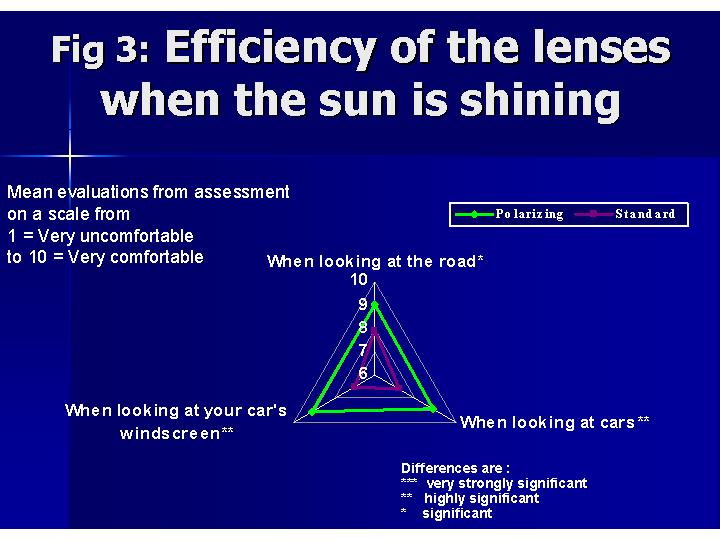
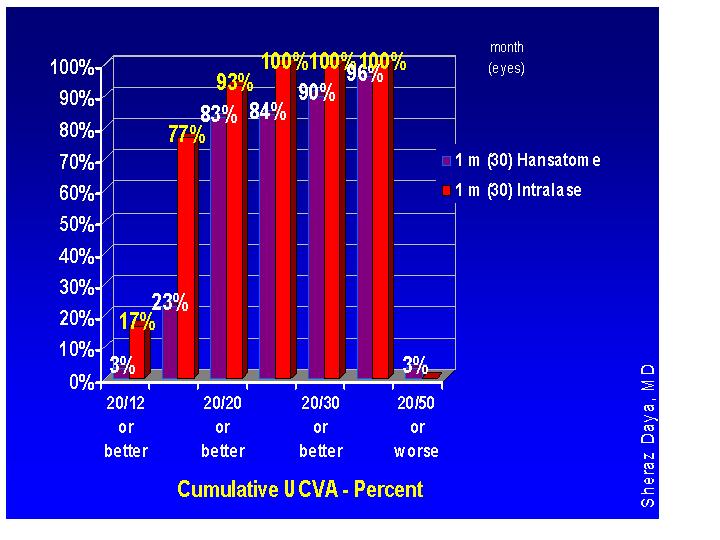
From August 2004, a total of 352 procedures have been performed at Centre for Sight and only two eyes have required an enhancement for regression. Initial nomogram changes had to be made as there was a tendency to very minor undercorrection. Refractive outcomes have improved dramatically, with 77 per cent of eyes with acuities of 6/5 unaided as compared to 23 per cent with a keratome flap using the same laser and software (Figure 4).
A further advantage of IntraLase is the reduction of epithelial defects at the time of surgery compared with keratomes. This has been the experience of the author and others.1 Epithelial defects at the time of surgery can lead to inflammation, epithelial in-growth and unpredictable refractive outcomes.
IntraLase flaps have considerable advantage over keratomes in terms of both safety and refractive outcome. These are summarised in Table 1.
Figure 4. Keratome Lasik vs Intralase Lasik using same software (0 to -12.00D)
INTRACORNEAL RINGS
Intracorneal rings have been used for the correction of myopia and more recently there has been considerable interest in using this modality in keratoconus.4,5 While not always effective, it can delay corneal grafting by a reduction of both astigmatism and myopia enabling patients to tolerate contact lenses and spectacles again. Considering the relatively high incidence of keratoconus (1:2,000), this is a welcome option.
Problems with intracorneal rings have included infection, extrusion and induced astigmatism. These problems have resulted mainly from improper placement, with channels either too superficial or tilted (being deep at one end and superficial at the other). In the process of creating channels the cornea can also perforate.
The IntraLase laser has been used to insert rings and has the advantage of ensuring these are at uniform depth and accurately placed deep within the corneal stroma. The process of ring insertion is also more comfortable for the patient. The author has used the laser to create channels for insertion of rings and has found the process much easier (Figure 5). Whether there is a difference in refractive outcomes remains to be seen and is the subject of audit at Centre for Sight.
LAMELLAR KERATOPLASTY
 |
| Figure 5. Channels for Intacs created with Intralase. Arrow shows insertion point at the 12 o' clock position on the patient |
FUTURE APPLICATIONS
As with all technology, more applications will undoubtedly be developed to make maximal use of this femtosecond laser. Use of the laser to produce posterior lamellar tissue for deep lamellar endokeratoplasty is about to be investigated by the Corneoplastic unit in East Grinstead.
Preparation of the donor disc is a demanding task and if preparation using the laser is found to be safe for the endothelium, it would make the procedure simpler and more rapid. It is conceivable that donors can be made to order and distributed by the Eye Bank.
 |
| Figure 6. Femtosecond laser lamellar keratoplasty. Donor creation on an artificial anterior chamber |
The femtosecond laser is a new addition to the armoury of corneal and refractive surgery. Presently the technology is prohibitively priced and, as a result, subject to much criticism. The enhanced safety of the device, better visual outcomes and ability to perform other corneal procedures made this technology an obvious choice for Centre for Sight. This has resulted in added cost per procedure and this has been passed on to the patient. Is the added price worthwhile? The answer would be a resounding yes! When given a choice, over a two-month period, 100 per cent of all patients at Centre for Sight chose IntraLase rather than conventional Lasik. As a result, Centre for Sight has stopped performing conventional Lasik, opting for IntraLase in all cases except Lasik on corneal grafts.
References
1 Kezirian GM, Stonecipher KG. Comparison of the IntraLase femtosecond laser and mechanical keratomes for laser in situ keratomileusis. J Cataract Refract Surg, 2004; 30: 804-11.
2 Giledi O, Mulhern MG, Espinosa M, Kerr A, Daya SM. Reproducibility of Lasik flap thickness using the Hansatome microkeratome. J Cataract Refract Surg, 2004; 30: 1031-7.
3 Giledi O, Daya SM. Unexpected flap thickness in laser in situ keratomileusis. J Cataract Refract Surg, 2003; 29: 1825-6.
4 Colin J, Cochener B, Savary G, Malet F, Holmes-Higgin D. INTACS inserts for treating keratoconus: one-year results. Ophthalmology, 2001; 108: 1409-14.
5 Siganos CS, Kymionis GD, Kartakis N, Theodorakis MA, Astyrakakis N, Pallikaris IG. Management of keratoconus with Intacs. Am J Ophthalmol, 2003; 135: 64-70.
