Optometrists have a range of daily wear soft contact lens replacement modalities available, from daily disposable to reusable lenses with a two-weekly or monthly replacement schedule. Personality, lifestyle factors, and ocular health should all be taken into account when deciding which lens and which lens modality to prescribe.
The monthly wearer
Most practices prescribe monthly replacement lenses to one degree or another. But is there really such a thing as a ‘monthly personality’? Market research by Johnson & Johnson Vision Care Companies suggests that contact lens wearers with a strong preference for monthly replacement tend to be people who want to wear contact lenses every day as their primary source of vision correction. They are busy living life, and not particularly engaged in the contact lens experience. These patients want reliable and hassle-free contact lens wear and seek simplicity in their health care and product choices. They are value-conscious and seek to maximise their use of each pair of contact lenses.1
From the prescriber point of view, we want to make sure these patients have no significant ocular health issues, and have not experienced problems with contact lens comfort or visual performance in the past before recommending monthly replacement.
But once that decision has been made, how do we know monthly replacement was the right choice? Are these patients really extracting the value and performance they crave out of their lens wearing experience? The answer is no, probably not.
To determine whether a contact lens patient’s wear experience is relatively trouble-free, eye care professionals ideally want to know how the patient’s lenses are performing throughout the whole replacement interval. With monthly wearers, this can be quite challenging, because the replacement frequency does not coincide with the typical examination frequency.
Examination and after-care timing
In the typical scenario, the patient comes in for a contact lens examination and fitting, and diagnostic lenses are dispensed at that time. Eye care professionals then see the patient again five to 10 days later for a contact lens check. If everything is satisfactory, the patient orders a supply of the lenses. There may be no other scheduled appointments until the next annual visit, especially for an experienced wearer.
At the time of that initial contact lens check, a daily disposable lens wearer has replaced their lenses multiple times, and a two-weekly replacement wearer is at least halfway through and possibly nearing the end of the replacement cycle. But the monthly lens wearer is still very early in the replacement cycle. Potential issues with lens comfort and satisfaction tend to become much more noticeable after the second week.
Some eye care professionals schedule monthly replacement lens wearers to come in for their after-care visits at one month, giving them a better sense of their experience over the full replacement cycle. While they may have suspected that some were not fully satisfied, wearers often do not actively talk about it during their annual visits; by consistently seeing their monthly wearers at the one-month time point highlights that some patients experienced dryness in the last week or so of the replacement cycle.
Two surveys of current monthly contact lens wearers, conducted by independent market research firms for Johnson & Johnson Vision Care Companies, highlight the decline in comfort over the month is not unusual. In the first survey by Leger (Canada) of 758 wearers from the US, UK and Germany, nearly three-quarters of monthly wearers (73%) reported experiencing comfort-related issues (discomfort, lens awareness, feelings of dryness or irritation) during the month.1
The share of those saying they were very/extremely comfortable dropped by almost 20% between end of week one (68%) and end of week four (49%) according to a second study where 237 participants responded to a daily digital survey (Kadence, USA) over the course of a month of wear of a new pair of their habitual lenses (figure 1).2 Blurry vision also became more prevalent as the month went on. As a result, as patients approached the end of the replacement cycle, half the monthly lens wearers were either no longer satisfied or ‘neutral’ with their overall satisfaction of their contact lenses.
Compensating mechanisms
The return visit schedule typically is not set up to capture the full monthly experience. Patients who experience problems after the initial contact lens check would have to proactively contact their eye care professional to set up a separate follow-up appointment if they wanted to raise concerns about the experience. Most will not take that step. Instead, they try to carry on using compensating mechanisms (table 1).
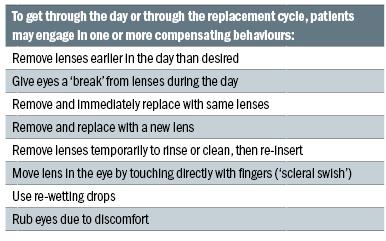
Table1: Patient behaviours to compensate for discomfort
According to the Leger study, 84% of those who experience comfort-related issues compensate with lens removal, rinsing, cleaning, breaks or rewetting drops at some point during the month.
Some of these behaviours, especially when relied upon sparingly, are harmless. Although directly touching a lens while on the eye, or extra handling of lenses during the day, could introduce foreign bodies or microbes if the patient does not carefully wash their hands prior to any management. One recent study showed that symptomatic patients with a decline in comfort over the day actually got little relief from compensating behaviours (replacing lens with a new one, removing and reapplying the same lens or performing a ‘scleral swish’ after five hours of wear).3
That is troubling. If patients are removing lenses earlier in the day than desired, replacing them more often than intended due to discomfort, or taking breaks during the day, it is not hard to imagine that the ‘breaks’ may become longer, the wear duration shorter, and patients may eventually shift to part-time wear or drop out altogether with the progression of contact lens discomfort as depicted in figure 2.
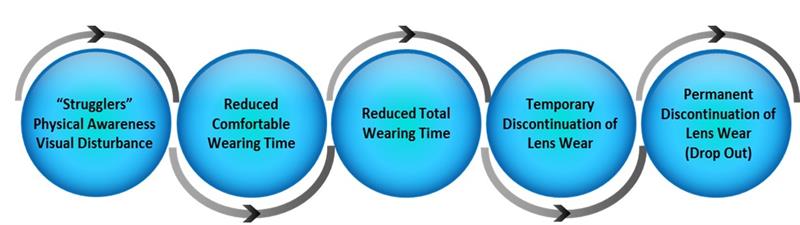
Figure 2: Progression of contact lens discomfort (adapted from Nichols J et al. TFOS International Workshop on CL Discomfort. IOVS 2013; 54 : TFOS7–TFOS13)
Suffering in silence
But if the contact lens experience is so uncomfortable for patients, why are these monthly replacement contact lens wearers not complaining?
More than eight out of 10 (82%) of the monthly wearers who experienced comfort-related issues said that made them feel annoyed, inconvenienced, or frustrated,2 with a similar proportion (84%) compensating for the comfort issues with lens removal, breaks or rewetting drops. However, the majority of these monthly wearers (73%) said they do not plan to tell their eye care professional about their comfort problem at their next visit as the majority of them believe comfort issues are ‘normal’ (85%).1
Why would that be? Some do not mention it because they are afraid their eye care professional will recommend they stop wearing contact lenses, but 61% of patients in the Leger study view declining performance over the month as normal and expected. By the time the next annual check-up rolls around, expectations for lens wear have been firmly established and compensating behaviours to deal with fluctuating performance become so routine, they may go unmentioned.
Some patients can keep this up for years, but we should consider them at increased risk of dropout. Eye care professionals often do not even know when it happens because that patient – who just wants something hassle-free - just stops coming back for annual check-ups and examinations. Most likely, they are not raving about their contact lenses or referring friends and family.
Improving the experience
We owe patients a better contact lens wearing experience.
Short of scheduling repeat follow-up visits, there are ways to dig more deeply into the wearing experience during annual examinations. Probing questions can help the eye care professional better understand whether patients are comfortable and satisfied for the entire month. Are they getting a comfortable, full 30 days of wear out of their contact lenses so that they feel like they have good value? Or are they ‘making do’ and becoming irritable about it, as the survey data suggest?
Good questions to get to the bottom of this may include:
- Are there times during the month when you need to take a break from your lenses?
- How often do you need to use re-wetting drops?
- At what time of the day do you start noticing your lenses and want to take them out? Does that happen earlier in the day towards the end of your replacement cycle?
Then, if the patient does seem to be struggling, it may be time to reset expectations. Patients need to hear from their eye care professionals that it is possible to enjoy more consistent contact lens performance, that it is not normal to be uncomfortable or to have to temporarily remove their lenses every day. Frequent eye rubbing or using eye drops do not have to be the price you have to pay for wearing contact lenses.
For these struggling patients, even if their lifestyle and physiology needs would seem to place them in a monthly replacement group, a shorter replacement schedule may be more appropriate.
A daily disposable lens is the ideal choice for patients who are struggling with a decline in lens performance over the wearing period. A fresh lens every day is the most convenient way to wear lenses and eliminates problems with solution compatibility as well. But it might be too much of a jump for the patient who seeks value and really wants to be a monthly replacement lens wearer.
Those patients may just be demanding a great deal of their lenses. Declines in lens performance have been associated with high levels of digital device use or having to perform in challenging environments. Patients with these types of high demands may do better with a shorter, two-weekly replacement period.
One study that looked at 112 ‘problem patients’¬ those who were struggling with frequent or constant discomfort or dryness, at least two hours per day of uncomfortable wear, or certain slit-lamp findings – found that being refitted with Acuvue Oasys contact lenses (senofilcon A) made a big difference.4 Eighty-eight percent of the struggling patients experienced a statistically significant improvement in comfort (p<0.0001) and 76% had more hours of comfortable wear (p=0.004). Additionally, Acuvue Oasys has still never been beaten in comfort by any monthly lens, according to trials reported in the clinical trials database (www.clinicaltrials.gov).5
Strategies for success with patients who have a ‘monthly personality’ but need to move to a shorter replacement schedule include emphasizing that getting the best value from their lenses means enjoying worry-free lens wear every day, not just the first week or two of the replacement cycle. Encouraging an annual supply is also an effective way to encourage compliance. Studies have shown that when patients have more lenses on hand, they are less likely to stretch out the replacement cycle and more likely to replace the lenses on time.6
There are patients who prefer a monthly replacement schedule and who may be able to maintain lens comfort and satisfaction throughout the month. However, many of them suffer in silence or resort to compensating behaviours, instead of telling their eye care professional about the negative aspects of their contact lens wear experience. Think about what you are doing now to head these problems off before your patient begins the ‘progression to contact lens discomfort and eventual drop out’ spiral.
Practices can truly benefit from improving the experience for patients. A large majority of the patients (80%) who reported comfort issues said that if their eye care professional switched them to a more comfortable lens, they would have a more positive opinion of that professional, recommend them to friends and family, and be more likely to return to the practice or make additional purchases.2
Your patients and your practice deserve a lens that can sustain excellent performance all month long, including weeks three and four. But that means a couple of things may have to change about how we evaluate our patients and new lens introductions moving forward.
- We need to give our patients the opportunity and ‘permission’ to tell us that their comfort is NOT okay at the end of the replacement cycle, or that they are having to do something extra to make it through their full month.
- When a manufacturer brings you a new monthly replacement product, review its data on performance at weeks three and four.
The Tear Film and Ocular Surface Society (TFOS) International Workshop on Contact Lens Discomfort indicated that one of the causes of contact lens discomfort could be related to lens dehydration.7 Therefore, in developing new lenses, the ability to resist dehydration would be a desirable quality. A new contact lens material, Senofilcon C, aims to combat lens dehydration by harnessing the power of natural lipids in tears, which act to prevent evaporation of aqueous from the ocular surface and to maintain corneal hydration.
Through integration of lipids within the structure of the lens, hydration can be maximised and maintained over the course of the day and indeed month, to help provide reliable, superior overall comfort, all month long.8
Cristina Schnider is director, global professional affairs, and Michelle Wales is manager, global strategic insights at Johnson & Johnson Vision Care, in the USA.
References
1 Data on file, JJVCC 2016. Online survey conducted in 2015 among 758 current monthly spherical SiH daily wear contact lens wearers in the US, UK, and Germany.
2 Data on file, JJVCC 2016. Online survey conducted in 2015 in which 237 US respondents who were current monthly spherical SiH daily wear contact lens wearers responded to daily surveys over a 30-day period.
3 Navascues-Cornago M, Morgan PB, Maldonado-Codina C. Effect of three interventions on contact lens comfort in symptomatic wearers: A randomised clinical trial. PLoS One 2015;10(8): e0135323.
4 Riley C, Young G, Chalmers R. Prevalence of ocular surface symptoms, signs, and uncomfortable hours of wear in contact lens wearers: The effect of refitting with daily-wear silicone hydrogel lenses (senofilcon A). Eye & Contact Lens 2006;32(6):281-6.
5 www.clinicaltrials.gov is a website maintained by the NIH. The 14 clinical studies evaluated subjective comfort as a primary or secondary endpoint for Acuvue Oasys with Hydraclear Plus Technology. Review conducted as of April 16, 2016
6 Schnider C, Jedraszczak AM. The ‘pantry load’ effect: Can it help drive happier patients and healthier practices? Paper, American Academy of Optometry, 2012.
7 Jones L, Brennan NA, González-Méijome J, Lally J, Maldonado-Codina C, Schmidt TA, Subbaraman L, Young G, Nichols JJ; members of the TFOS International Workshop on Contact Lens Discomfort. The TFOS International Workshop on Contact Lens Discomfort: report of the contact lens materials, design, and care subcommittee. Invest Ophthalmol Vis Sci. 2013 Oct 18;54(11):TFOS37-70
8 JJVCC data on file 2016; 30-day dispensing evaluation, monthly replacement DW study, n=533 SiH CL wearers in US. Superior CLUE & MR survey comfort scores vs 3 SiH monthly CLs overall across all time points (p<0.05).
