The optometrist’s role is to undertake full eye examination, diagnose any ocular or visual disorder and, if necessary, refer patients for appropriate management. Nowadays with retinal cameras, OCT scanners and highly technologically advanced equipment available in general practice we are able to diagnose ocular conditions accurately.
OCT provides a rapid, non-invasive method to assess retinal tissue at a microscopic level. We are able, for example, to decipher microaneurysms due to diabetes, and cystoid macular oedema due to branch retinal vein occlusion for instance with much greater accuracy.
OCT-A
Fluorescein fundus angiography (FFA) was considered the gold standard in the evaluation of retinal vascular perfusion and diagnosis of ischaemia. Unfortunately, it is time consuming, costly and invasive so can lead to anaphylaxis. For optometric practices it is not a viable option.
Nearly three years ago, Optovue brought out its first OCT-angiography (OCT-A) instrument (the AngioVue) and I have been fortunate enough to enjoy the technology which has offered me a deeper understanding of the vascular pathology associated with conditions such as diabetic retinopathy, vein occlusion, wet AMD and glaucoma. OCT-A uses motion contrast imaging to obtain high resolution volumetric blood flow information from the retina and choroid, thereby generating angiographic images instantly and non-invasively.
Another difference between FFA and OCT-A is that FFA only works in nearly transparent structures so allowing good imaging of vasculature of the superficial capillary network of the retina but not the deep capillary layers. The OCT-A images both the superficial and deep retinal vascular plexi. Using colour-coded, mapping a perfusion density map with quantitative data is assembled.
Fresh from the optical battle field, I will report on a case of patient with branch retinal vein occlusion and the resultant capillary non-perfusion and retinal ischaemia.
More than the brain or any other body tissue, the retina is a tissue with highest oxygen demand and therefore needs a continuous supply of blood for nourishment. Vascular occlusion or capillary closure can lead to areas of non-perfusion.
This impairs nutrition of the neuroglial tissue in the retinal parenchyma and the resultant hypoxia increases the release of vascular endothelial growth factors (VEGF) which promote both angiogenesis and increased vascular permeability. The angiogenic response is formation of new vessels which can bleed easily into the vitreous.
Branch retinal vein occlusion (BRVO) is the second most common retinal vascular disease after diabetic retinopathy. Macula oedema is the most common cause of visual loss in BRVO. The current thinking postulates that the deep choroidal plexus normally helps remove interstitial fluid from the retina.
With deteriorating flow in the deep choroidal plexus, there is a build up of interstitial fluid and hence the macula oedema. Figure 1 shows diabetic maculopathy with central cystoid changes, as well as microaneurysms and exudates, but there is no capillary non-perfusion. Figure 2 shows OCT-A revealing a choroidal neo-vascular membrane in wet AMD.
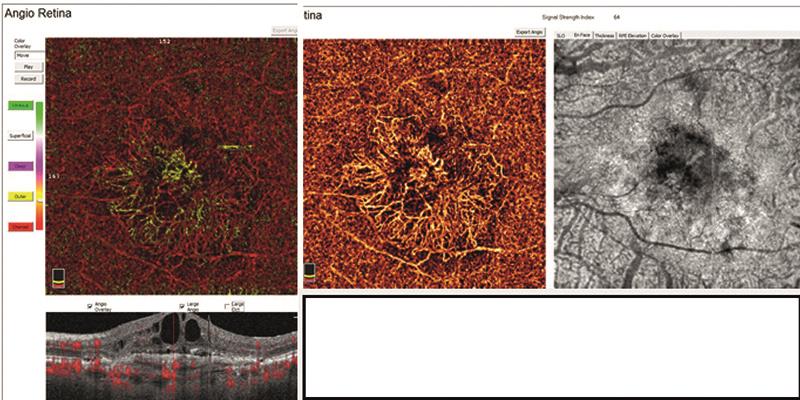
Figure 2: Type 3 choroidal neovascular membrane emanating from the choriocapillaris and extending into the outer retina causing retinal pigment epithelium detachment and cystoid maculopathy
Case study
A 63-year-old female, ES, attended for her first eye examination at the practice. She was using +3.50DS ready readers and complained that her left eye was blurred. She also reported a scotoma on the nasal aspect of her left eye. She was vague about her last eye test, possibly six months ago, and she had visited her local optician having noticed blurred left eye vision and problems with the ‘bottom part’ of her vision. She thought the optician had said all was well and no action was taken?
Refraction:
R Unaided (6/12) +1.50DS (6/9) ADD +2.00 (N5)
L Unaided (<6/60) Count Fingers at 1metre
Ocular examination:
- Anterior examination revealed no corneal abnormalities except for mild, early cataracts in each eye.
- Normal intraocular pressures at 18mmHg R & L.
- Fundus examination revealed no abnormalities of the right fundus.
- Left fundus revealed a superior temporal branch retinal vein occlusion, an epiretinal or fibrous membrane, a macula hole and blot hemorrhages in the periphery. Inferiorly there was also a sign of venous nipping.
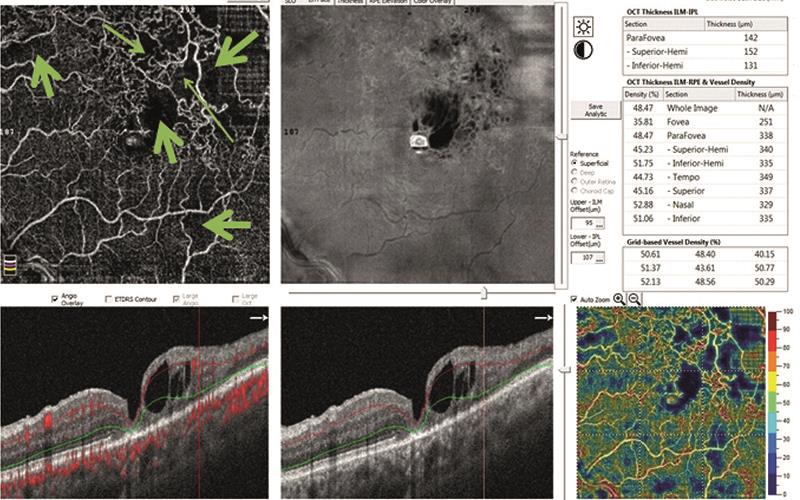
Figure 3: Superior BRVO with capillary loss (non-perfusion identified by green arrows), collateral vessels. And haemorrhages cascading from the superior fundus to the macula where cystoid maculopathy is present. Lamellar (partial thickness) macular hole is visible. The far right image shows blood flow density with large areas of non-perfusion (indicated by blue arrows)
OCT examination:
The OCT was much more conclusive (figure 3) and the observations were as follows:
1 Lamellar (partial thickness) macula hole.
2 Cystoid macula oedema centrally.
3 >50 micro-aneurysms superior and temporal to the fovea.
4 Superior temporal deep and superficial capillary loss and capillary non-perfusion.
5 Collateral vessels seen between the capillary loss areas.
6 Density map showed no flow areas superior temporal and superior nasal.
7 Angiography montage of superior and deeper capillary plexus showing capillary loss in both layers (figure 4).
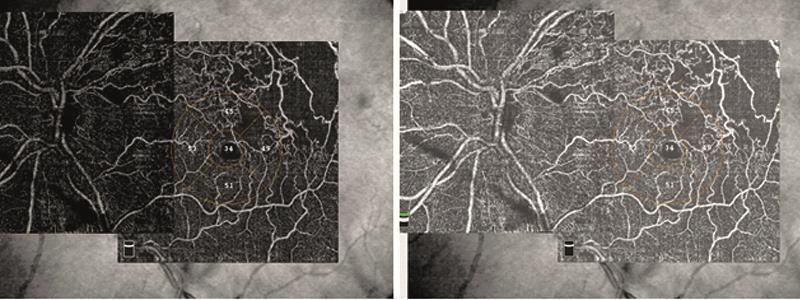
Figure 4: Superior capillary plexus (left image) and deeper capillary plexus (right image).
Clinical decision
It was explained to the patient that she had suffered a superior branch retinal vein occlusion. It was likely to have been a few months old, as she had not noticed any inferior field problems some 6 months earlier, but with the capillary loss on the temporal aspect she had noticed a nasal scotoma.
She was advised to consult her general practitioner to rule out hypertension, diabetes, hyperlipidaemia and blood dyscrasias (increased viscosity) as the underlying cause. She was also referred to an eye specialist to confirm the diagnosis and, perhaps, to undertake an FFA to rule out ischaemia. This would determine whether she would require pan-retinal photocoagulation or anti-VEGF treatment.
Technology practice of the year

The staff from Radlett Opticians accepting their technology Practice of the Year Optician Award
Team Radlett Opticians set the foundation 26 years ago by investing in technologically advanced equipment to ensure that their patients had the best eye care available on the high street and were empowered with eye care knowledge.
‘This has culminated in our tiny, semi-rural practice achieving a total of four Optician Awards (in 2006, 2012 and finally in 2017). Patients travel far and wide to visit the practice and, through their recommendation and experiences, patients help spread the word.’ The practice aspiration has always been to provide high standards of care and accurate diagnosis with cutting edge technology.
‘The 2017 technology award was a truly remarkable award and our winning was helped greatly by the effort of our young trainees, dispensing optician Rebecca Cooper and optometrist Aaran Patel, who picked up the baton and pushed the practice over the line.’
Optometrist Kirit Patel, who for so long has been a pioneer in embracing new ideas, helped develop the young team. The design of the practice presents a modern yet friendly environment and, notably, there is an open glass lift for disabled patients.
Rebecca Cooper has been instrumental in designing bespoke spectacles by Tom Davies and relishes using the Visio-Office digital dispensing platform as well as the iPad to dispense tailor-made varifocal lenses.
She is fully trained on the E-Eye (high energy pulse meibomian gland dysfunction therapy unit) and able to administer the series of intense regulated pulses of light to patients. Similarly, Aaran has been participating in this new and exciting treatment and it is this teamwork between the two that promotes effective treatment of the patients.
Why has Radlett Opticians won three technology practice of the year awards in 11 years? ‘Patients have commented at every visit that there is something new when it comes to their eye test, and children find it particularly amazing that we write our notes on a Samsung tablet.’ Phoropters, topographers, an Intuitive Colorimeter, slit-lamp and fundus cameras have all been used at the practice for nearly 20 years.
Over the past 10 years, the OCT and Daytona ultrawide field scanning laser ophthalmoscope system have superseded the traditional digital fundus camera, and the knowledge that Kirit Patel has acquired over the years has been passed not only to the patients, but also to his trainees.
Readers will also know that he has also spent a good deal of his time writing for Optician on interesting clinical case studies, and he has also regularly given lectures on subjects as varied as glaucoma, dispensing dilemmas and use of the OCT.
Has the investment stopped there? ‘Oh no. This year marked the arrival of the Eye Tracker system to help monitor both children and adults with reading difficulties. The original Daytona was recently replaced with the Daytona Plus which offers high resolution images for diabetic retinal examination and its advanced software provides unique support in interpreting changes on the retina.’
What is the limit for modern optometry? ‘The eyes and the brain are intrinsically linked. The retinal cells respond to a visual stimulus and this then tracks from the optic nerve to the visual cortex. We now have a unique ability to assess retinal cell function with the use of pattern electroretinography (ERG) and visual evoked potential, and we can record the time taken for the retinal cell response to travel to the visual cortex.
This can be then be recorded as a unique pattern. Radlett Optician now has invested in the DiopSys ERG system which has advanced the monitoring of glaucoma, macular degeneration and patients with optic nerve dysfunction.’
What is the feedback from patients? Thank-you letters adorn the consulting room walls and words such as ‘vigilant’, ‘skilful’, ‘spending extra time’ and ‘dedicated’ are found throughout. One letter from a 13-year-old who had suffered a hyphaema says it all: ‘Thank you for being such a brilliant optician and seeing me after hours and getting my vision back to normal. I am grateful for your care and concern.’
Should other practices apply for the awards? ‘An emphatic ‘yes’, especially if you are true to your clinical skills and patient care. Then all the hard work and dedication pays dividends in the long run. Achieving the awards gives the practice a certain kudos and offers all the staff a moral boost, invaluable when you run busy clinics. To use a sports analogy, you have to put in lots of training and the rewards only come in that one moment or one night!’
Kirit Patel is an independent optometrist with a practice in Radlett, Hertfordshire.
