An unseen, unyielding whisperer of blindness affects around 30% of the world’s population. That figure is expected to rise to 50% by 2050. Myopia’s relentless march poses a major health threat, and if steps are not taken to stop myopia turning into high myopia (ie requiring glasses with a prescription of minus five or stronger) then 10% of the world’s population will be at risk of blindness by 2050.1
Blindness and visual impairment due to myopia
High myopia increases the risk of pathologic ocular changes such as cataract, glaucoma, retinal detachment, and myopic macular degeneration (figures 1 a to d). Patients with myopic retinopathy in the USA, are on average registered legally blind, for 17 years (as opposed to five years for diabetes or age-related maculopathy).5
Are we doing enough to reduce these sight-threatening conditions?
Progressive myopia can increase in excess of one dioptre each year. Where it does, might it be appropriate to see our patients every six months? They may be unaware of the subtle change in visual acuity over the period, wherein schoolwork may suffer due to a blurring whiteboard.
Are we taking every opportunity to discuss treatment options with young progressive myopes and their parents? Are we telling them the disturbing truth that, for every increase in their prescription, there exists an exponential risk of sight-threatening conditions?
What is progressive myopia?
Emmetropisation is the development process that ensures a greater frequency of emmetropic eyes during the early growth phases of the eye. It co-ordinates the development of the various components of the optical system (eg axial length, refracting power of the cornea, depth of the anterior chamber, etc) to prevent ametropia.
The average axial eye length of a newborn is 16mm. Through infancy, this lengthens to about 19.5mm and ends at an average of 24.5mm in the adult eye, usually by the age of 13 years.
Progressive myopia occurs when the eye lengthens axially in excess of the length it would normally attain due to emmetropisation, and continues to do so over a period of years.
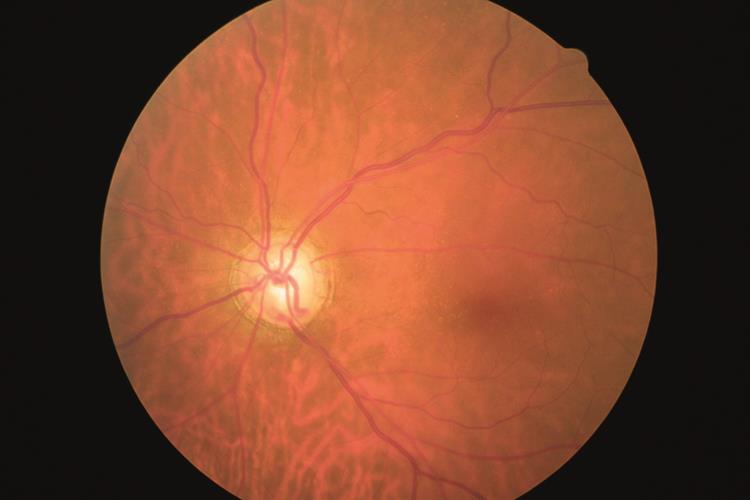
Figure 1b: Glaucoma is known to have an association with myopia
What causes progressive myopia?
The link between disrupted emmetropisation and excessive near vision tasking appears particularly overwhelming. Apart from the odd session of axe-head production and cave painting, prehistoric humans were not over-burdened with near vision tasks. Emmetropisation was therefore not troubled by the unknown mechanism which encourages axial elongation and causes progressive myopia. Myopes were probably rare, and where they did make it through the genetic pool, they might soon in their vulnerable haze be savaged by the local sabre-toothed tiger. In modern times, due to the advent of computers, iPhones and tablets, emmetropisation is frequently influenced.
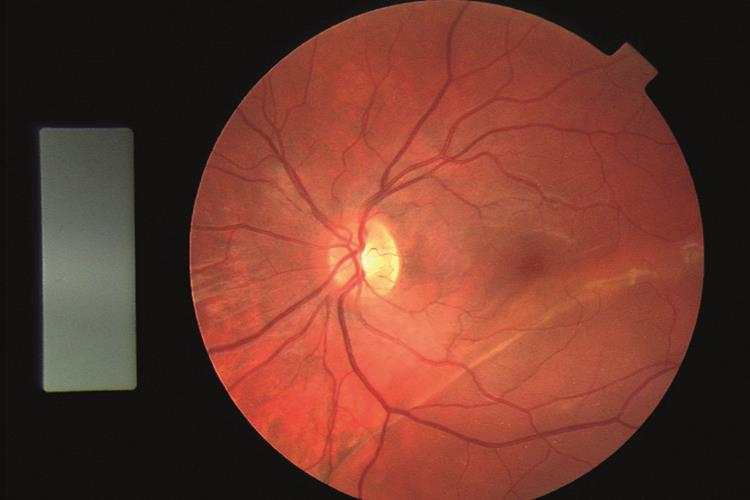
Figure 1c: Retinal detachment is linked with myopia
We are all aware that the human body is capable of reacting to a stimulus that it views as harmful. The outcome of this is almost always positive, but not always. Examples of detrimental changes that effect the eyes include the blood vessel growth in age-related macular degeneration and proliferative diabetic retinopathy which represent a natural response when tissues are starved of oxygen.
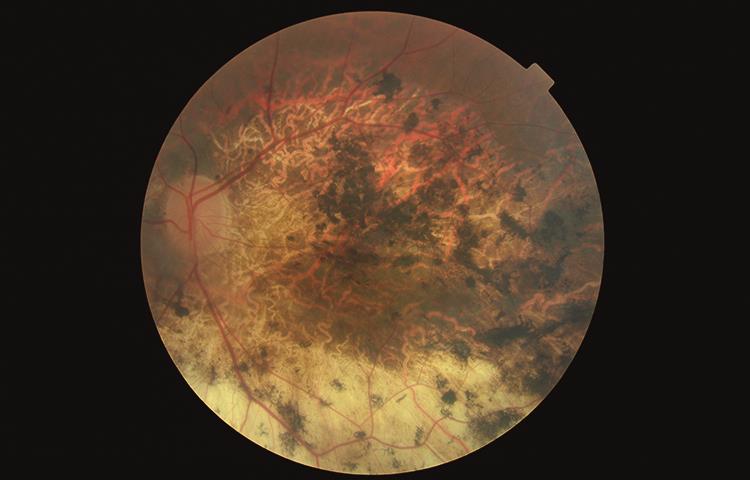
Figure 1d: Myopic retinal atrophy is know to have an association with myopia
Additionally, conditions exist where the body loses its ability to differentiate between foreign material and its own cells. These autoimmune conditions can also affect the eyes and include Reiter’s, Sjögren’s and Beçhet’s syndromes, Still’s disease (a form of juvenile arthritis), and systemic lupus erythematosus. Progressive myopia might be considered as another example of how nature can get it wrong in response to variation in stimuli.
Genetic or environmental?
Both genetic and environmental factors appear to contribute to progressive myopia. Familial studies show a definite genetic link for high myopia and a strong one for low myopia, while outdoor activity and reduced myopic progression clearly show a strong environmental association less related to genetic factors.
More on the modern obsession with near vision tasks
The eyes were not made for excessive and prolonged near vision tasks. Facebook, Snapchat and Twitter were never on the divine or evolutionary agenda. No wonder the miracle of human vision is losing its way.
Myopia is frequently associated with esophoria at near6 (a tendency for the eyes to move more inward than necessary when viewing a near object). Myopia seems more prevalent where a demanding educational system prevails, and near-work has been associated with myopia for more than 200 years.7
When a subject’s attention moves from a distant object to a near one, hyperopic defocus is created. This occurs where off axis peripheral light is focused behind the retina regardless of where the central focus is located. Increasing accommodation reduces the amount of hyperopic defocus. However, where the association between accommodation and convergence is abnormal, as in the case of a child with esophoria at near, the excessive hyperopic defocus remains – in this case due to under-accommodation in an effort to avoid diplopia.
The accommodative convergence/accommodation ratio (AC/A) is defined as the amount of convergence measured in prism dioptres per unit (dioptre) change in accommodation. Where there is an increased AC/A alongside myopia, there is an increased incidence of a rapid increase in progressive myopia. Importantly, there also appears to be a raised AC/A ratio in patients prior to the onset of myopia.
A retrospective study using the records of clinics at the Department of Optometry, National University of Malaysia, classified subjects into three groups: more than six prism dioptres of exophoria, zero to six prism dioptres of exophoria and any esophorias. The prevalence of myopia in the esophoric group was significantly higher than the other groups, suggesting that near esophoria might be an important factor in myopia development.8
Two studies9,10 showed a greater prevalence of myopia in Inuit children compared to their parents after the introduction of Western-style education. Goss hypothesised that the defocused retinal image might lead to an increased production of growth-inducing substances.11 If we can take something positive from the modern scourge of progressive myopia, Goss suggested, a return to a balanced visual day that does not over-excite the mechanism that causes axial elongation would halt progressive myopia in its tracks.
Current treatment regimes for progressive myopia
Several treatments designed to slow the progression of myopia have been advocated. Not all of these are effective. For instance, under-correction was once thought to slow myopia’s progression. However, most studies have determined that it has no effect, and one even showed an increase in the rate of progression.12
Likewise, distance correcting soft or rigid contact lenses are generally accepted to have no effect on the axial length of the eye.
Orthokeratology
Orthokeratology lenses are gas permeable contact lenses worn overnight to reshape the cornea. They work by moulding the cornea so that the peripheral image is moved closer to the retina, reducing the hyperopic defocus or indeed inducing myopic defocus. The patient is not aware of the visual change in the periphery as they will generally only be concerned with foveal vision.
Multifocal soft contact lenses
Centre distance multifocal contact lenses work in a similar way to Ortho-k, moving the peripheral image closer to the retina and reducing hyperopic defocus.
Bifocals and progressive addition lenses
Children with both esophoria and myopia showed a 25% reduction in progressive myopia when fitted with a bifocal correction compared to a control group fitted with single vision lenses.13
Atropine
Myopic progression was significantly retarded with the use of atropine (using a dose of 0.01%) and had minimal side effects (compared with dose rates of 0.1% and 0.5% while maintaining comparable efficacy).14 Despite the documented reduction in myopic progression, the mechanism by which this is achieved is still not fully understood.
7-methylxanthine (7-MX)
7-MX is a metabolite of caffeine. It increases the thickness of the posterior sclera, therefore resisting axial lengthening of the eye. A Dutch study of 107 children ages eight to 13 found that 400mg tablets qtd of 7-MX decreased myopia progression by 66% and reduced axial length by 44% compared to the placebo group, but the product is not commercially available and some have raised concerns about long term effects of dosing.15
A stroll in the park – daylight
Retinal dopamine is normally produced on a diurnal cycle, increasing during the day. It tells the eye to switch from rod-based, nighttime vision to cone-based, daytime vision. Some researchers believe that under dim (typically indoor) lighting, the cycle is disrupted, with consequences for eye growth. Studies found that around 30% of a group of six-year-old children who spent 40 additional minutes outdoors each day developed myopia as opposed to 39.5% who did not spend extra time outside. Those who spent more time outside also had less strong prescriptions.16
A study led by Professor Scott Read also surmised that increasing exposure to natural light is the key to reducing the myopia epidemic in children. It concluded that children need to spend more than an hour (preferably at least two hours) each day outside to help prevent myopia from developing and progressing.17
Similarly, a school in Taiwan compelled its children to spend their daily break time outside. After one year, doctors had diagnosed myopia in 8.41% of the children, compared with 18% at a nearby school who did not go out in their break time.18
Outdoor activities reduce the amount of near vision tasks and provide elevated levels of natural sunlight both of which may contribute to the reduction of progressive myopia.
Scotopic light-gradient theory
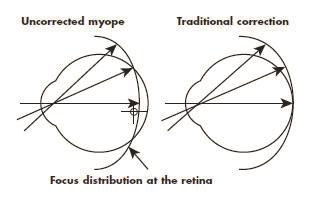
That the peripheral retina contributes to the axial lengthening of the eye is surprising. Perhaps more so is that the fovea has little to do with the process. That excessive and consistent levels of hyperopic defocus (figure 2) cause axial lengthening of the eye is generally accepted, but to suggest that there exists a mechanism by which the eye/brain recognises that an image received in the peripheral retina is behind it and decides to grow towards it is a huge leap. A number of research papers have reported a possible role for the peripheral refraction in the development and progression of myopia. In their review article, Charman and Radhakrishnan discuss these numerous studies and evaluate the interaction between peripheral refraction and the development of refractive error.19
When hyperopic defocus is present, the amount of light reaching the peripheral retina is substantially less than it would be if it were a sharply focused image. Hyperopic defocus reduces gradually towards the fovea, resulting in an increase in light and a corresponding light-gradient increase from the periphery to the fovea.
The concave form of myopia spectacle lenses also contributes to the light gradient, where the thinner centre allows relatively more light to the fovea than the thicker edge towards the periphery. Furthermore, when undertaking near vision tasks, the constriction of the pupils disproportionately concentrates light at the fovea as opposed to the periphery. These factors all favour a light-gradient biased towards the fovea and this may, through a mechanism involving the rods, cause the eye to axially elongate.
The rods are ideally placed to register this gradient. They are absent from the foveola, but a few degrees away their density rises and they are then found spread over a large area of the retina. The rods are responsible not only for scotopic vision but also act as a highly sensitive motion detector in our peripheral vision, each being linked with an increasingly large receptive field out to the periphery.
There are approximately 120 million rods as opposed to seven million cones. The rods are extremely efficient photoreceptors utilising the photo pigment rhodopsin and are more than one thousand times as sensitive as the cones to low-light levels.
Should the scotopic light-gradient theory, whereby light levels rather than image focus is the driver, have validity and be responsible for axial elongation, then an opportunity to stop or at least reduce myopic progression would, by the provision of a light-gradient opposite to the one described, be of some advantage. Equally, a reduction in hyperopia could be achieved by accentuating the light-gradient to encourage axial elongation.
Hyperopic defocus is the motivator for axial elongation and progressive myopia. A ‘reasonable’ amount of hyperopic defocus stimulus occurred in prehistoric man but not enough to upset the delicate process of emmetropisation. Twenty-first century man, by virtue of excessive near vision tasking, is overstimulating the mechanism, resulting in pandemic levels of progressive myopia. Both genetics and environment can contribute to the light-gradient. Progressive myopia is initiated primarily by the peripheral retina and not the fovea.
The mechanism which initiates axial elongation is caused by hyperopic defocus which produces a light-gradient, brightest at the fovea and disproportionately dimmer towards the periphery. Hyperopic defocus is increased for near vision tasks and exacerbated when esophoria at near is present. The constriction of the pupil on near vision tasking increases this effect, concentrating a disproportionate amount of available light on the fovea. Concave lenses contribute to the gradient.
The highly sensitive rods play a role in registering this gradient; where there is an excessive and persistent amount of hyperopic defocus, the mechanism causing axial elongation is turned on. A growth factor similar to that which grows new blood vessels may be implicated.
Orthokeratology, multifocal soft lenses and atropine all reduce the light-gradient to a degree. The first two move the image closer to the retina, decreasing the retinal blur and increasing the light falling on the peripheral retina. The latter (atropine) dilates the pupils, more evenly spreading available light to the periphery. Outdoor activities reduce the amount of near vision tasks and the light gradient is further reduced by more natural light levels.
The eyes may be encouraged to stay in an emmetropic state, or discouraged from increasing axial elongation and progressive myopia by utilising a device which produces a reverse scotopic gradient. Original ideas include +3 dioptre lenses which are occluded centrally and mounted in a round frame. A natural light source is placed so that a significant reverse light-gradient is delivered to the retina for a controlled period each day.
A soft contact lens with a centrally occluded zone would have the same effect, with the added benefit that, if fitted correctly, the fovea would always receive a reduced amount of light irrespective of small eye movements. Hyperopia could be reduced by utilising a device which accentuates the light-gradient, encouraging axial elongation. We await further research before this interesting theory is verified.
Myopia levels
- In East Asia, myopia has reached epidemic levels. 96.5% of 19-year-old males in Seoul are short-sighted.2
- In the United States, myopia increased from 25% to 42% in three decades.3
- In the UK, myopia has more than doubled in the past 50 years in children aged between 10-16 years.4
Conclusion
I hope this article enables you to discuss myopia with concerned patients with a good understanding of the various influences under study aimed at addressing the very high prevalence of the condition.
Edward Adams is a contact lens optician practicing in Wiltshire and has a special interest in myopia.
References
1 Report of the Joint World Health Organisation–Brien Holden Vision Institute Global Scientific Meeting on Myopia. 2015. www.brienholdenvision.org/news/item/77-new-report-on-myopia-and-high-myopia-released.html.
2 Jung SK1, Lee JH, Kakizaki H, Jee D. Prevalence of myopia and its association with body stature and educational level in 19-year-old male conscripts in Seoul, South Korea. Invest Ophthalmol Vis Sci. 2012 Aug 15;53(9):5579-83.
3 Vitale S et al. Increased Prevalence of Myopia in the United States Between 1971-1972 and 1999-2004. Arch Ophthalmol. 2009;127(12):1632-1639.
4 McCullough SJ, O’Donoghue L, Saunders KJ (2016) Six Year Refractive Change among White Children and Young Adults: Evidence for Significant Increase in Myopia among White UK Children. PLoS ONE 11(1): e0146332. https://doi.org/10.1371/journal.pone.0146332
5 Green JS, Bear JC, Johnson GJ. The burden of genetically determined eye disease. British Journal of Ophthalmology. 1986 Sep;70(9):696-9.
6 Goss D, Rosenfield M, (1998). Myopia and Nearwork (edited by Rosenfield M and Gilmartin B). Butterworth Heinemann.
7 Ware, J. (1813). Observations relative to the near and distant sight of different persons. Philosophical Transactions of the Royal Society, 103, 31-50.
8 Chung KM, Chong E. Near esophoria is associated with high myopia. Clin Exp Optom. 2000, Mar-Apr;83(2):71-75.
9 Young FA, Leary GA, Baldwin WR, West DC, Box RA, Harris E, Johnson C. The transmission of refractive errors within eskimo families. Am J Optom. 1969 Sep;46(9):676-85.
10 Morgan RW, Speakman JS, Grimshaw SE. Inuit myopia: an environmentally induced ‘epidemic’? Can Med Assoc J. 1975 Mar 8;112(5):575-7.
11 Goss DA, Wickham MG. Retinal-image mediated ocular growth as a mechanism for juvenile onset myopia. J Opt Soc Am A. 1988 Dec;5(12):2080-6.
12 Chung K, Mohidin N, O'Leary DJ. Undercorrection of myopia enhances rather than inhibits myopia progression. Vision Res. 2002 Oct;42(22):2555-9.
13 Fulk GW, Cyert LA, Parker DE. A randomized trial of the effect of single-vision vs. bifocal lenses on myopia progression in children with esophoria. Optom Vis Sci. 2000 Aug;77(8):395-401.
14 Chia, Audrey et al. Five-Year Clinical Trial on Atropine for the Treatment of Myopia 2. Ophthalmology 2016, Volume 123, Issue 2, Pages 391–399.
15 http://optometrytimes.modernmedicine.com/optometry...
16 Mingguang He et al. Effect of Time Spent Outdoors at School on the Development of Myopia Among Children in China; A Randomized Clinical Trial. JAMA. 2015;314(11):1142-1148. doi:10.1001/jama.2015.10803.
17 Read SA, Collins MJ, Vincent SJ. Light Exposure and Eye Growth in Childhood. Invest Ophthalmol Vis Sci. 2015 Oct;56(11):6779-87.
18 Wu PC, Tsai CL, Wu HL, Yang YH, Kuo HK. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology 2013;120:1080-5.
19 Charman WN, Radhakrishnan H. Peripheral refraction and the development of refractive error: a review. Ophthalmic Physiol Opt. 2010 Jul;30(4):321-38.
