Among all the lectures about retinal disease and technology developments at the annual conference of the British Association of Retinopathy Screeners held at the end of last year, one lecture from Adam Heritage (Imperial College, London) stood out. From his experience as a medical photographer, he felt that the issue of patient anxiety prior to an appointment had implications often forgotten and showed evidence that addressing this anxiety has clinical benefits.
Fear of the unknown
A study a few years ago on patients attending for MRI assessment, funded by Siemens, reported that 63% of them would rather not know than be told they had a treatable illness. This rather shocking statistic (which becomes less shocking when you think about it) underlines the problems faced by clinicians in terms of patient attendance and also, indirectly, with compliance with any management plans.
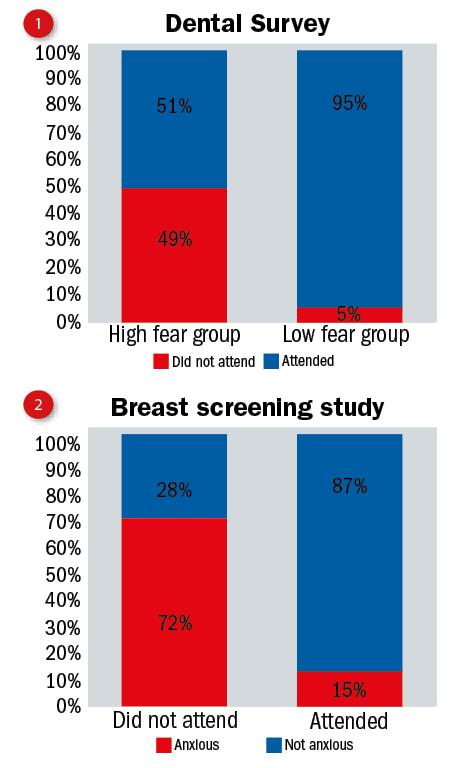
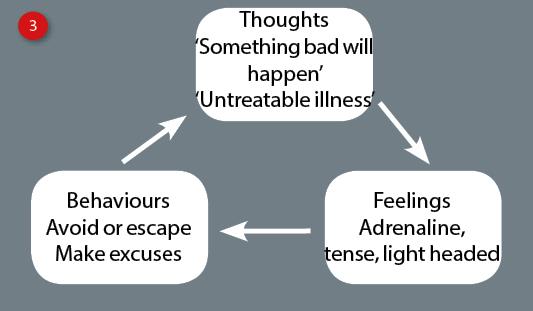
Anxiety about what is involved in any clinical appointment or what might be found subsequently has been found to be a major reason for non-attendance, for example, at dental appointments (figure 1) and for breast screening (figure 2). There is similar evidence that some fear attendance of eye checks, not just for financial worries about having to fork out for expensive spectacles, but about being told they have some threat to their sight.
The implications for such non-attendance are significant, both in terms of the cost of wasted appointment time, but also in the long term impact upon health status of the population, with less early diagnosis and management of disease for example.
Reasons for anxiety
Through questionnaire and record analysis, the team at Imperial have highlighted the main reasons cited for anxiety prior to an appointment (in this case specific to dilated retinal imaging). These were:
1 Confusion – not knowing what was being done at an upcoming appointment was the commonest cited reason for anxiety.
2 Fear of outcome – would the appointment result in bad news to the patient?
3 Bad information – confused or unclear instruction about what was happening, where and when and why.
4 Lack of control – in this case this was mainly the patient being told they should be driven to and from the appointment and so had less autonomy over the day.
5 Waiting times – particularly a fear of being left in waiting rooms for long periods, though often this is perceived as being more time consuming than is actually the case.
Among the many other causes cited alongside these main ones were specific fears about individual procedures, such as use of needles, drops or physical contact.
Vicious cycle of anxiety
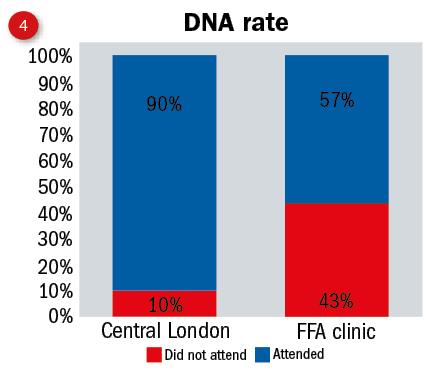
These anxieties all feed into a vicious circle (figure 3) and steps to break this would improve patient and financial outcomes. NICE guidelines are, according to Heritage, less than helpful and simply suggest the importance of respecting the patient’s concerns and independence.
Imperial have addressed this advice by, prior to an appointment, adopting the following;
- Making instructions clearer, for example how to get to a clinic
- Regular review of what is sent out
- Appointment reminders
- Easy access to staff
- Avoid hospital induced cancellations
Once the patient has arrived;
- Ensure clinicians introduce themselves and explain their role
- Make relevant information easily available – how long are waiting times, ask for questions, explain what and why and so on
Found to be particularly detrimental to a patient’s anxiety state are emotive or jargon-based comments, such as the use of abbreviations and statements such as ‘you have nothing to worry about’, and ‘just try to relax.’
Imperial has found that offering patients something to do while waiting, for example during dilation, patient anxiety scores are significantly reduced. Indeed, a lack of activity in the waiting room was one of the three top patient complaints, the other two being;
- Lack of realistic information about waiting times
- Poor waiting room facilities
Putting it into practice
As common sense as much of this may seem, it has only been over the past couple of years that this area has been addressed with any sort of formal approach and figure 4 shows the significant impact this has had in improving attendance rates at the Imperial clinic.
Heritage finished his presentation by asking everyone to begin by thinking of just one change they might make to improve their patients’experience.
