A 63-year-old male patient, had been under my care for routine diabetic screening as far back as 2003. His diabetes was best controlled with metformin and glimepiride. His other medications included doxazosin, amlodipine, and enalapril, (for hypertension) and lipitor for hyperlipidaemia. In late 2003 he was referred to an eye specialist with a central serous retinopathy (CSR) in the left eye. Subsequent recurrent CSRs left him with reduced vision in the left eye.
His spectacle prescription had been unchanged for 10 years and it was as follows:
R -0.75DS / -1.00DC X 105 (6/6) Near N6 unaided
L -0.75DS / -1.25DC X 85 (6/18) Near N12 unaided
Diagnosis
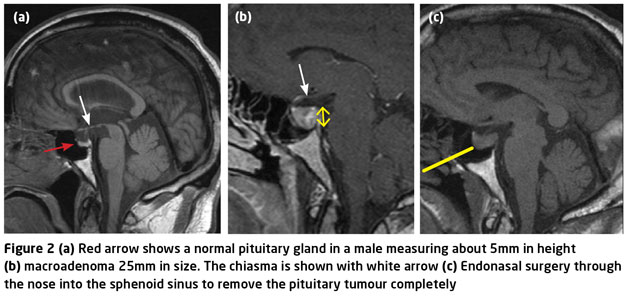
In 2009 he was seen by an endocrinologist because of proteinurea and this diligent endocrinologist looked at his face, then the hands and rightly suggested a diagnosis of acromegaly. He was referred to a neurologist and the brain scan confirmed the diagnosis. Further tests showed high levels of calcium in the body, but in the sternum it was particularly high suggesting an active thymus gland. The patient had been susceptible to recurrent kidney stones since the age of 18 yet acromegaly had never been suspected. This is because it is a condition rarely encountered in general medical practice. The cause of the kidney stones was the excessive calcium production due to the continuing growth of the thymus gland. An MRI scan of the pituitary showed a macroadenoma, a large neoplasm of part of the gland (Figure 1).
Treatment
In 2010 treatment commenced as follows:
? Cinacalcet – a calcium mimetic to treat hypercalcaemia
? Sandostatin injections – to prevent release of growth hormones
? Cabergoline – to suppress prolactin production.
In August 2011 trans-sphenoidal surgery was undertaken and 66 per cent of the tumour was removed (Figure 2).
The rest could not be removed due to its proximity to the optic nerve. Radiotherapy was suggested but the patient was reluctant to have this, although he is aware that radiotherapy would shrink the tumour further. There is still a risk that the tumour can regrow aggressively with no further intervention.
An unusual finding was a report by the patient of fat-like deposits in one of his legs. This is result of soft tissue deposition on his knee.
Observation in optometric practice
The following observations were made on our acromegaly patient (Figure 3):
? Physical signs included multiple folds on the forehead, large hands with sweaty palms, large feet, an enlarged nose
? The MRI image showed frontal bossing and widely spaced teeth
? Soft tissue thickening – seen in the image taken of the left leg which appear thicker than the right leg.
Other observations that have been mentioned in literature are:
? Protruding jaw
? Large tongue and enlarged lips
? Increase in skin tags, oily skin
? Soft tissue increase in the wrist leading to carpel tunnel syndrome due to compressions of the nerves
? Sleep apnoea is common (our patient did suffer from this), as is depression
? Impotence and loss of sex drive
? Interrupted menstrual cycle
? Production of breast milk
? Overdevelopment of the body (giantism)
Some readers may remember the actor Richard Kiel who played the villain Jaws in the James Bond movies Spy who loved me and Moonraker and was acromegalic.
The pituitary gland
An oval shaped gland that secretes hormones for growth and metabolism, the pituitary lies at the base of the brain and below the optic nerves in the region of the chiasma. A normal pituitary gland is 3-8mm in height and is larger in females.
Multiple acromegaly
The patient was diagnosed with multiple acromegaly, a rare and serious variation of the condition which leads multiple endocrine neoplasia. These are classed as:
? Thymus growth – the thymus usually stops growing in the third decade of life. The thymus gland is located below the throat and behind the sternum. It releases a hormone that stimulates the production of T-lymphocytes in the bone marrow
? Hyperparathyroidism – a tumour of the parathyroid gland leads to hyperparathyroidism. Over-production of parathyroid hormone leads to high blood calcium levels. There are four parathyroid glands located in the neck behind the thyroid gland
? Pituitary gland tumour.
Diagnosis of acromegaly
Clinical features mentioned above should alert the clinician to possible acromegaly. The usual test is to measure the blood IGF-1 level. The liver produces the insulin-like growth factor 1 (IGF-1) and its production is stimulated by growth hormone (GH) which is released from the anterior pituitary gland. The secretion has an important role in childhood growth.
Another test is the measurement of blood levels of GH after drinking a sugary drink. In normal people, GH levels are suppressed below 1µ/L and generally untraceable, though occasionally peaking to 30µ/L or so due to sporadic episodic secretions. In patients with acromegaly, the secretion is continuous so the levels of GH are high and never return to undetectable levels.
Treatment of acromegaly
Trans-nasal sphenoidal surgery (Figure 2) through the nose and into the sella turcica (a saddle-shape depression in the sphenoid bone) is an easy and effective way to remove and hopefully cure the tumour. Studies have shown long-term cure success in 80 per cent of patients with microadenomas, while only 50 per cent of patients showed long-term cure in those with macroadenomas. This was the case in our patient with macroadenoma.
Stereostatic radiotherapy is used in cases where surgery and medication cannot control acromegaly. This is thought to take around 18 months to lower the levels of GH and IGF-1. Sometimes the GH and IGF-1 levels can be elevated for 10 to 20 years following radiotherapy and medical supplementation has to be given.
Medical treatment
Most patients with acromegaly require both surgical and medical treatment to control the condition. The key drugs are as follows:
? Sandostatin – this is used in the interim period before radiotherapy becomes effective. It is a short-acting injection containing octreotide, a somatostatin analogue. Somatostatin prevents the release of GH and in turn reduces the production of IGF-1
? Cabergoline – this is a dopamine agonist. The pituitary gland produces the hormone prolactin. In normal patients the level of prolactin is around 20µg/L while in those with pituitary tumours it can rise to as high as 1,000-10,000µg/L. Dopamine, or an agonistic agent, travels down the pituitary stalk and inhibits prolactin production
? Hormone replacement – elevated prolactin in men results in low testosterone levels, loss of sexual interest and impotence. In pre-menstrual women it can result in loss of menstrual periods and pregnancy difficulties. Treatment employs hormone replacement of testosterone in men and oestrogen and progesterone in women
? Cinacalcet – this is used in the treatment of secondary hyperparathyroidism and works by mimicking the action of calcium upon target tissues. An increase in parathyroid hormone levels leads to bone fractures, often with severe pain, soft tissue and vascular calcification as well as cardiovascular complications.
Conclusion
I hope this article has given useful background into a very rare condition which presented in my practice. In the next part in this series we will be looking at a different presentation of pituitary adenoma.
Read more
Systemic disease: Heteronymous hemianopias
Systemic disease: Acromegaly and its diagnosis
Systemic disease: Vascular disorders with neurological consequence
Systemic disease: Vascular disorders with neurological consequence
Systemic disease in practice: Pontine haemorrhage and diplopia
Systemic disease in practice: Aneurysms, subarachnoid haemorrhage and headaches
Kirit Patel is an optometrist who runs an independent practice in Radlett, Herts