The College of Optometrists pre-reg scheme is a well-structured programme with a continuing assessment element that depends upon each pre-reg gaining sufficient experience to be competent in a wide range of optometric skills, including record-keeping and communication.
There are many milestones to be reached along the way and opportunities to identify concerns so that things stay on track during the pre-reg year. This article will look at the overall year and highlight some important things to think about to get the most from the experience.
Supervisors
Establishing a good rapport with your supervisor is essential to success. They will be able to ensure you are progressing adequately, achieving all the requisite experience, check your work, discuss your evidence before you present it to assessors, and be on hand at each assessment to agree to any action plan implemented by the assessor. If all goes to plan, you will form a long lasting friendship – some of my past pre-regs are still regularly in touch with me.
Assessors
As a pre-reg optometrist, you have two assessors and their roles are quite different. Your stage 1 assessor will be in touch with you early on in your year and then visit for at least three, usually four assessments. They are likely to correspond in between, perhaps to check on progress or prompt you to prepare for forthcoming assessments.
They are responsible after each assessment in agreeing with you and your supervisor a plan of action to ensure you are on target or where you may want to focus or gain more experience. As such, you will likely get to know them quite well and, hopefully, you will find this a constructive and helpful process.
The stage 2 visit is much more like an examination and the second assessor is not allowed to offer feedback on the day about the assessment. This assessor will thus seem much more formal and distant. But if you are suitably prepared, this will not be a hurdle.
Competencies
Overall, there are 75 competency elements to be signed off at stage 1 and then be rechecked at stage 2. Most of these are assessed at visits 2 and 3. The elements fall into eight main units. These are will become very familiar and, even after qualification, will keep cropping up as you maintain your CET level. The eight units are:
1 Communication
2 Professional conduct – this includes legal and ethical responsibilities and management protocols such as referral and record keeping
3 Methods of ocular examination
4 Optical appliances – the dispensing one
5 Contact lenses
6 Ocular disease
7 Assessment of visual function – the refraction one
8 Binocular vision
Each element requires understanding of a specific area and a requirement to have been able to undertake whatever is involved to show this. For example, an element of unit 5 is ‘Chooses, fits and orders rigid lenses’. Your assessor requires specific evidence to be made available at visits before they can sign you off as competent in each of the elements.
Evidence
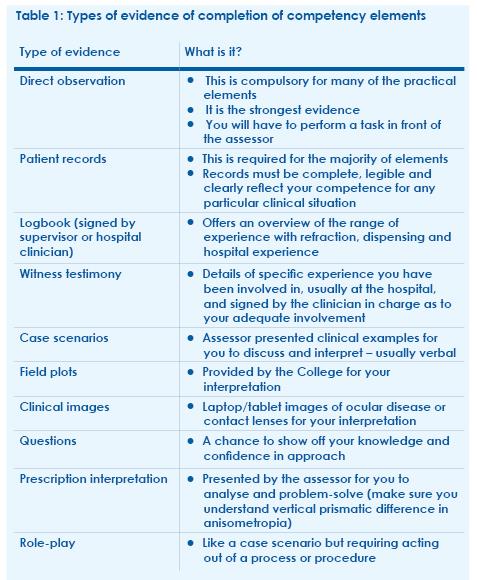
The individual forms of evidence required by an assessor varies with each element. The different types of evidence are summarised in table 1.
The assessor requires three bits of evidence for each element but also has some compulsory ones that must be met – these are in your logbook and I strongly recommend you get familiar with these right at the start of the year – you will be so glad you have.
Often, some evidence is simply not available to you by the time of the assessment – for example not having yet seen a certain ocular disease. If this is the case, your assessor will simply hold the element over till the next visit. Even though three visits are possibly all that is needed, it is almost always the case that a fourth visit is required before full sign off. Hopefully no more.
Patients
Success depends, like before, on good knowledge, but establishing a good rapport with a wide range of patients and developing good clinical decision-making relevant to the actual practice setting. This hopefully means that the modern pre-reg is much better prepared for practice life upon qualification.
Graduates leave our optometry departments with a sound knowledge base but very limited patient experience. Gaining this experience is a key aim of the year, and a successful year offers access not just to healthy numbers of refraction, contact lens and dispensing opportunities, but to a wide range of patients requiring the widest range of management.
The College stipulates target numbers to be achieved before stage 1 can be signed off (usually two thirds through the year). These numbers are not difficult to reach (350 refractions, 250 dispenses, and starting this year, 20 contact lens fits and 40 aftercares). Indeed, if they are proving difficult, this is usually to do with practice management (staff failing to book patients for the pre-reg, the pre-reg not being proactive and so on) and this needs to be rectified early on. Often, a stage 1 assessor will instigate action.
In my experience, those who achieve higher numbers of patients tend to perform better (and more time-efficiently), both in practical exams and in real life. Bearing this in mind, everyone within a practice needs to be on board with this concept. I have heard all too often of practice managers giving preference to qualified staff and so reducing a pre-reg’s testing numbers.
I occasionally come across a pre-reg with low patient numbers where it is clear they have been less than proactive in seeing patients – staying in the consulting room ‘to revise’ when a patient does not show, or blaming others when no one has yet brought in any children or elderly for you to see are not options. It is essential to become involved in the practice team and make sure everyone knows your role and your requirements right from the word go.
One important note about patients – as you will be discussing the personal clinical information of patients with your supervisor and assessor, you must establish their consent and have available some documented evidence that consent has been granted – I know of instances where assessors have refused to continue assessments because there was no clear evidence of consent from the patients a pre-reg had prepared to discuss. This is all the more important since the introduction of the GOC Standards of Practice guidance.
Hospital experience
It is a requirement for you to attend an eye hospital department for a minimum of five days and for this to include some specific experience. This is detailed in your College logbook and needs to be completed before stage 1 sign off. Your assessor is responsible for setting up the sessions and this is best done as soon as possible.
It is also best to have completed the experience before visit 3 as some of the competency elements (for example, seeing a child under two years of age or assessing anterior chamber cells and flare) are often rarely achieved outside the hospital setting. You will be asked by your assessor at visit 1 if things have been sorted – every year some people leave it too late and then run into problems completing their stage 1 within the expected timescale. Don’t let this be you.
Some Top Tips for the Year
- Keep your log books up to date and for each patient episode, however unremarkable it may seem at the time, make a few notes about the patient and note any possible competency elements they may represent. Many find it a good idea to keep a separate notebook. This will save much angst later in the year when you might otherwise be scrambling around for patients to prepare. Remember your log book is important to show the range of experience – detail is good. A list of ‘single vision/varifocal’ will not show off your range of dispensing ability.
- Record Keeping – check records you are to discuss, discuss them with your supervisor and any other appropriate staff member, get people to ask you questions about the record, and check the records again. Remember, the record should show a stranger quickly exactly what happened and what you did. Pay particular attention to the ‘management’ part – writing ‘gave drops’ ‘pen to nose’ ‘lid hygiene’ is not sufficient.
- Make sure all the relevant documentation is available – field plots if relevant, information sheets given out, referral documents and so on. If you use electronic systems, be ready to print them out – most assessors ask for this.
- Be able to justify your actions – a really useful skill is to be able to verbalise why you did what you did. Assessors will expect you to be able to explain about any patient and then answer questions like ‘what did you do and why?’ This cannot be got from a book, and though it may sound a little eccentric, practising answering such questions out loud before your assessment will be really helpful. Do not come across as if you are thinking about the patients you have prepared for the first time at the actual assessment
The following are essentials:
- Careful planning.
- Familiarising yourself with the College handbook from the start – everything is in there.
- Gathering records from the start for future selection – better to have a few to choose from than only one for each element.
- Remember good records include ones that may cover a number of elements.
- Keeping on excellent terms with your supervisor.
- Ensure you meet your targets.
- Keeping your experience as varied as possible – 350 refractions of the full range of patient age and ability is better experience than 1,000 refractions of 22-year-old low myopes.
