Every day many of us prescribe contact lenses to correct our patient’s vision. Although much attention is paid to assuring the lenses are a good fit and are comfortable for the wearer, optimal correction of the wearer’s ametropia and improvement of their visual performance critically hinges on harmonisation of the lens optics with the wearer’s own optics.
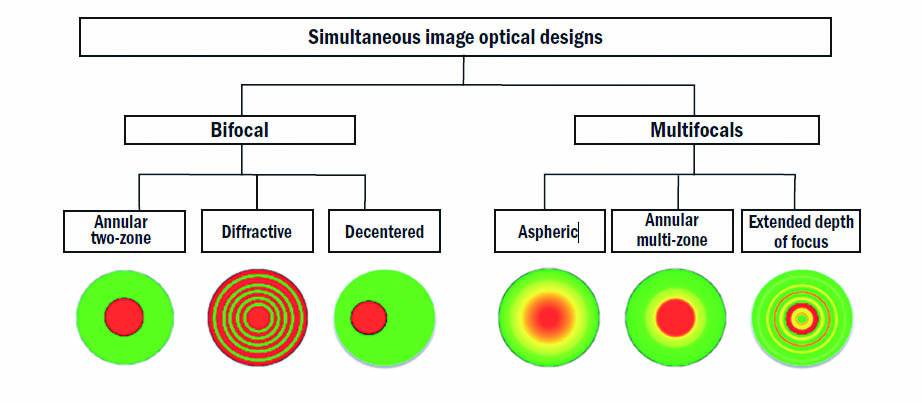
In Optician 04.11.22, Dr Nitya Murthy, Steve Newman and Professor Pete Kollbaum offered an overview of the BCLA CLEAR section relating to contact lens optics.1 The article covered the optics of the eye, including the need to consider higher order aberrations, such as spherical aberration and coma, which modern contact lens designs take into account along with the lower order aberrations such as myopia, hyperopia, and astigmatism. Contemporary lens designs were then discussed with a comparison of spherical and aspheric lenses and of multi-zone or advanced optical designs. Figure 1 shows a summary of different simultaneous image lens designs.
Figure 1: Simultaneous-image optical designs of contact lenses. Red, green and yellow colours represent the areas for distance, near and intermediate vision, respectively. The annular/zonal and aspheric designs illustrated here have a central distance correction: designs with centre near correction are also available
Some key points relevant to everyday practice include the following:
- Real world visual assessments should be considered rather than dependence on VA measurements alone.
- Patient-reported outcome measures are useful indicators of visual satisfaction and performance
- Centration of multifocal contact lens options is key for the patient’s quality of vision.
- Knowledge of contact lens optical design can help align the best design to a patient’s needs, and set patient expectations.
- Visual performance may improve with wear due to neural/blur adaptation.
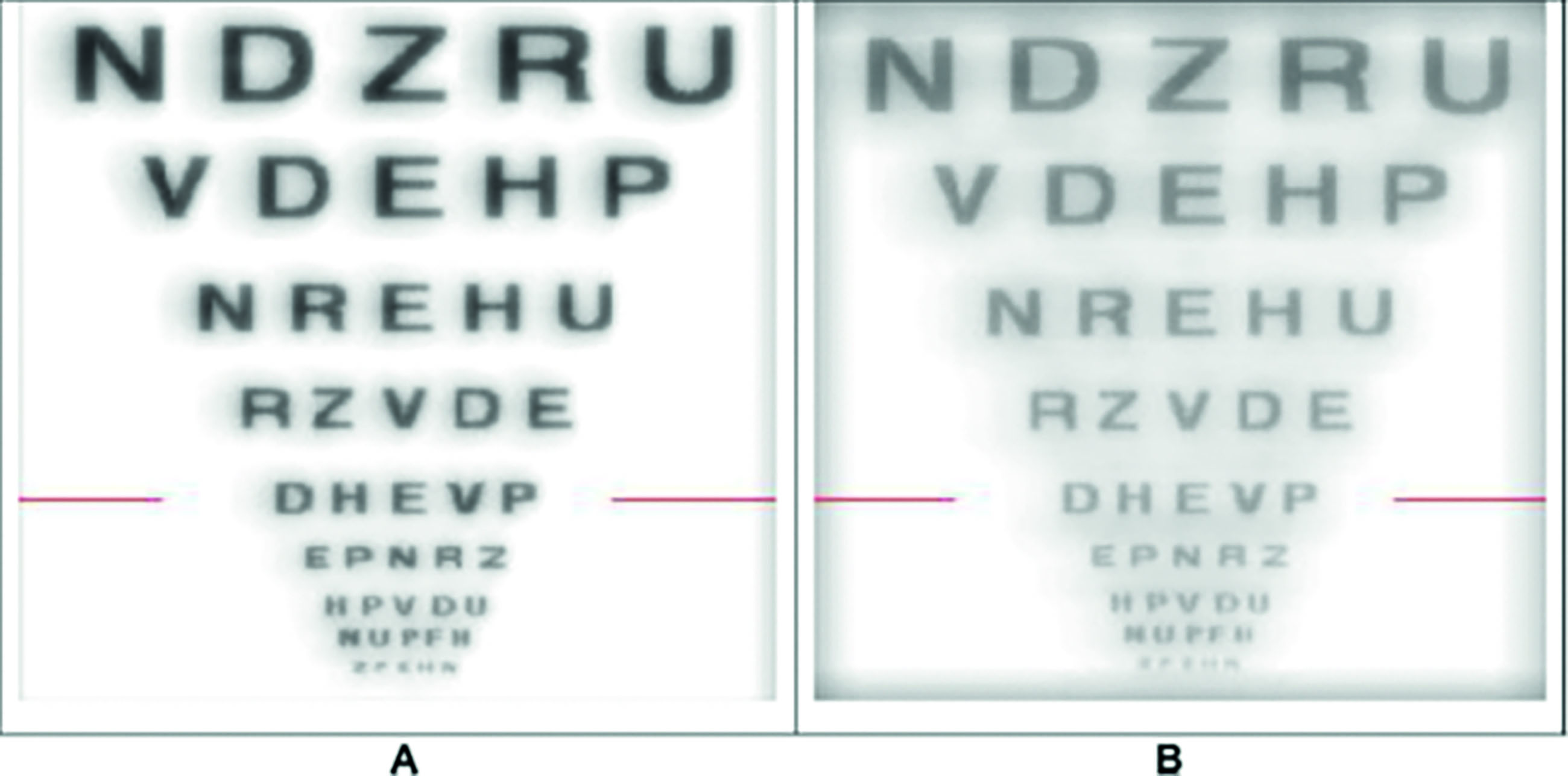
The overall conclusion was: ‘It is essential for us to fully understand these technologies and their underlying optics (figure 2). Accomplishing the goal to best help our patients will require knowledge and communication of lens optics and teamwork between manufacturers, clinicians and researchers.’
This article is now the source material for an interactive exercise that centres on the fitting of a presbyope for the first time with contact lenses. The case scenario to consider is designed to encourage consideration of both contact lens design and also the differences between contact lenses and spectacles in the way they influence the optical and binocular status of the eyes of the wearer.
Case Scenario
A 48-year-old patient attends your practice and asks about the possibility of contact lenses. They have the following spectacle refraction and binocular status:
- R: -4.75/-0.75 x 180 (6/5)
- L: -5.00/-0.50 x 180 (6/5)
- Add: +1.00DS (N6 R+L, range 1m to 20cm)
- Cover test:
- Distance: orthophoric with and without Rx
- Near:
With Rx (at 40cm): orthophoria
Without Rx (at 20cm): 4Δ XOP, good recovery
They are now struggling to read with their spectacles in place and find the working distance for reading too close when removing their spectacles. They have had multifocal spectacle options explained to them already, but are interested to know if their might be a contact lens alternative as, ideally, they would ‘love not to have to wear specs.’
For your discussions, consider the following questions:
- When a myope moves from spectacles to contact lenses, are there any optical considerations that might affect the binocular status?
- What might be your first-choice recommendation for a contact lens correction and why?
- What would be your priorities when first assessing the fit and vision through the lenses?
- What advice might you give to the patient before they first try your choice to maximise the potential for their adaptation to the correction?
Figure 2 (A) Simulated letter chart (red line denotes 0.3 logMAR) for an aberration-free eye wearing a low-add (for example, 0.3μm spherical aberration at a 5mm pupil diameter) aspheric multifocal lens. (B) Simulation of the same condition as (A) but with the lens decentred 0.5mm
Interactive CPD Instructions
In order to be able to log one provider-led interactive CPD point to your MyCPD account, this is what you need to do:
- Make sure you have read the article ‘BCLA CLEAR – Contact Lens Optics’ by Dr Nitya Murthy, Steve Newman and Professor Pete Kollbaum.
- Arrange a time to undertake a discussion on the subject with a similarly qualified registrant; another optometrist or dispensing optician.
- Read the case scenario and questions (above) and use them as the basis for the discussion with your colleague. Note, the discussion needs to address each of the questions outlined above and must be for longer than ten minutes
- When finished, you then need to send an email to ‘opticiancpd@markallengroup.com’ as follows;
- Subject box should state ‘CLEAR Interactive 5’
- Please state your name and GOC number
- Please state the name and GOC number of the person you discussed the matter with
- Please confirm you had read the source material
- Please include a summary of your discussion, explaining your views and thoughts on each of the three discussion questions
- Each submission will be read individually and, where needed, feedback will be given directly. Where the submission meets a required standard, you will receive an email confirming this which you can then use as evidence of completion allowing you to log one distance learning interactive CPD point.
- A summary of the responses and discussions will appear in a future issue of Optician with comment from the authors Neil Retallic is president of the BCLA.
Reference
- Richdale K, Cox I, Kollbaum P, Bullimore MA, Bakaraju RC, Gifford P, et al. BCLA CLEAR – Contact lens optics. Contact Lens and Anterior Eye, 2021;44(2):220-39. https://doi.org/10.1016/j.clae.2021.02.005
