Every day many of us prescribe contact lenses to correct our patients’ vision. Although much attention is paid to assuring the lenses are a good fit and are comfortable for the wearer, optimal correction of the wearer’s ametropia and improvement of their visual performance critically hinges on harmonisation of the lens optics with the wearer’s own optics. This paper summarises key concepts of the BCLA CLEAR paper on contact lens optics1 to aid eye care practitioners (ECPs) in applying this optical knowledge to their clinical practice in order to optimise their clinical decision-making built on a sound optical basis.
Overview of the optical design of the eye
Basic optical structure
Before discussing the optics of the lenses, it is imperative to first acknowledge the optics of the eyes themselves. Although often ignored, light first refracts through the tear film, a thin, fluid layer covering the corneal epithelium. If this layer is not smooth and uniformly thin it can have a dramatic impact on any resulting vision.2 Immediately posterior to the tear film is the cornea, which further refracts light. Refracted light from the cornea’s posterior surface travels through the eye’s entrance pupil, physical pupil and the posterior chamber, ultimately reaching the retina where it is imaged onto the eye’s photoreceptors.
If the light primarily focuses in front of the retina, the eye (or that local portion of the eye) is said to be myopic, whereas if the light does not yet focus on the retina but would come to a focus behind the retina, the eye (or that portion of the eye) is deemed to be hyperopic. There are other potential optical imperfections or aberrations that may be created by any of the components through which light passes, which may also impact vision in varying ways. Lower order aberrations such as myopia, hyperopia, and astigmatism are routinely addressed by contact lenses and other forms of correction. Certain higher order aberrations, such as spherical aberration and coma are more commonly included in overall contact lens optical designs but other aberrations such as trefoil, are not usually corrected. New research is being done to minimise their impact. This is briefly discussed in the lens design section later. These aberrations are called ‘monochromatic aberrations’ as they are wavelength specific. However, the eye also contains longitudinal chromatic aberration, whereby light of differing wavelengths are differentially focused; for example, blue wavelength light is focused anterior to red wavelength light.
Optical axes of the eye
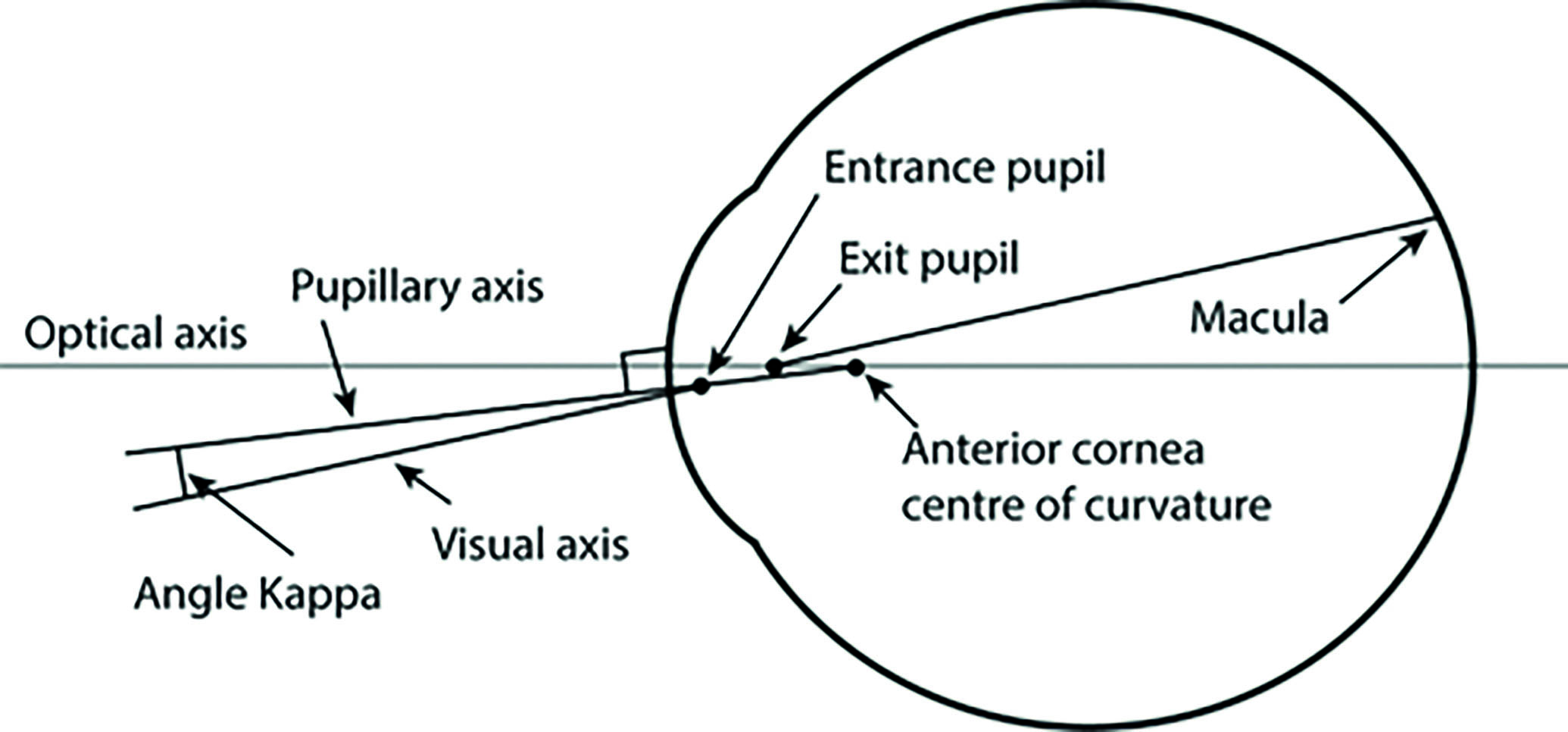
When describing the optics of the eye, a contact lens on an eye, or how the eye aligns with any imaging system, it is necessary to describe alignment relative to some reference axes (figure 1). However, since the corneal surfaces, lenticular surfaces, and the retina are not rotationally symmetrical and may be decentred and/or tilted relative to each other, the eye cannot be described like most rigid optical systems where the optical and geometrical centres of their optical elements coincide along a common optical axis. The most commonly-used theoretical optical axes of the human eye are the following:
- Pupillary axis; the line perpendicular to the cornea that intersects the centre of the entrance pupil
- Primary line of sight; the line that connects the fixation point in object space with the centre of the entrance pupil and the centre of the exit pupil with the fovea.
Figure 1: Optical axes of the eye
Optical models of the eye
When representing the optics of the eye, simplified optical models are often used. The simplest optical models of the eye are paraxial in nature and assume the alignment of the optical surfaces and homogeneity of the optical elements. The simplest models contain only one refracting surface, but adding more refractive surfaces, building models based on clinical population averages, or individualised eyes all yield more realistic and valuable models, which may better aid lens design. Each may have their place depending on the modelling task.
Changes in the eye with age
When averaging across the population, most human eyes contain differing levels of varying aberration, some positive and some negative, so the population average of the majority of aberrations is perceived as zero. This is not true for defocus and spherical aberration. Spherical aberration has a population average of around 0.15 microns (6mm pupil).3 Additionally, aging becomes a factor that can affect the relationship between the ocular components in particular spherical aberration) of the eye, as the natural compensatory relationship of aberrations between the cornea and lens is diminished. In particular, spherical aberration becomes more positive with advancing age, increasing approximately 0.05µm (over a 6mm pupil) with every decade of life. Other higher order aberrations increase in the sixth and later decades of life, particularly with the refractile changes in the crystalline lens that accompany cataract formation. Of course, with age, the accommodative ability of the crystalline lens decreases due to a gradual stiffening of the lens fibrils, signalling the onset of presbyopia.
Common aberrations
Spherical aberration: gradual, radially symmetric power change from the centre of the pupil or lens to the periphery of an optical system. It is present naturally in the eye as well as in contact lenses and other optical devices, where it is manipulated to provide corrective power. The crystalline lens of the eye partially compensates for the spherical aberrations of the cornea.
Coma: results from misalignment of the main optical components of the eye, such as if the cornea and lens and the contact lens optics are tilted or decentred relative to the visual axis.
Trefoil: a third-order aberration triangular astigmatism with different amounts of optical power at three principal meridians. It is most prominent in larger pupils and when the primary aberrations (defocus and astigmatism) are corrected.
Longitudinal chromatic aberration: Wavelengths of light that correspond to different wavelengths are imaged at different distances with respect to the retina because the indices of refraction of different optical components of the eye vary with wavelength.
Contemporary contact lens designs
Spherical versus aspherical lenses
Spherical contact lenses induce spherical aberration via the lens curvatures needed for fitting alignment and refractive error correction. In particular, minus lenses induce negative spherical aberration and plus lenses induce positive spherical aberration, both of which increase in magnitude as the power of the lens increases. Although each individual eye will have its own level of spherical aberration, the level of negative spherical aberration manifest in a -7.00 DS soft lens (with a Young’s modulus that is similar to the cornea) is approximately appropriate for cancelling out the inherent positive spherical aberration of the eye found in the population average.
In fact, most commercially available aspheric (aberration management) lens designs currently aim to do just this and compensate for the population average positive spherical aberration by inducing an amount of negative spherical aberration within the lens across its power range. However, any eye which does not have the population average positive spherical aberration will have resultant eye+lens spherical aberration, which may preclude optimal image quality. Further, any physical decentration of aspheric or aberration managed contact lenses away from the pupil centre will induce other aberrations (such as coma) in direct proportion to both the amount of spherical aberration and decentration. This induced coma may negate the visual benefits otherwise gained. Most lenses, in fact, do decentre inferiorly temporally relative to the pupil centre.4 For this reason, some companies have created lenses with decentred optical zones in order to preserve the coaxial relationship between the ocular and optical axes.
Relevance to practice
- Aspheric lenses provide better spherical aberration control across lens powers.
- Aspheric lenses may be more beneficial to eyes with higher refractive errors or higher refractive errors combined with levels of spherical aberration of the same sign as their refractive error (eg myopic eyes with negative spherical aberration).
- If vision is unexpectedly poor with a spherical design, consider changing to an aspheric design (and vice versa)
Multi-zone and advanced optical designs
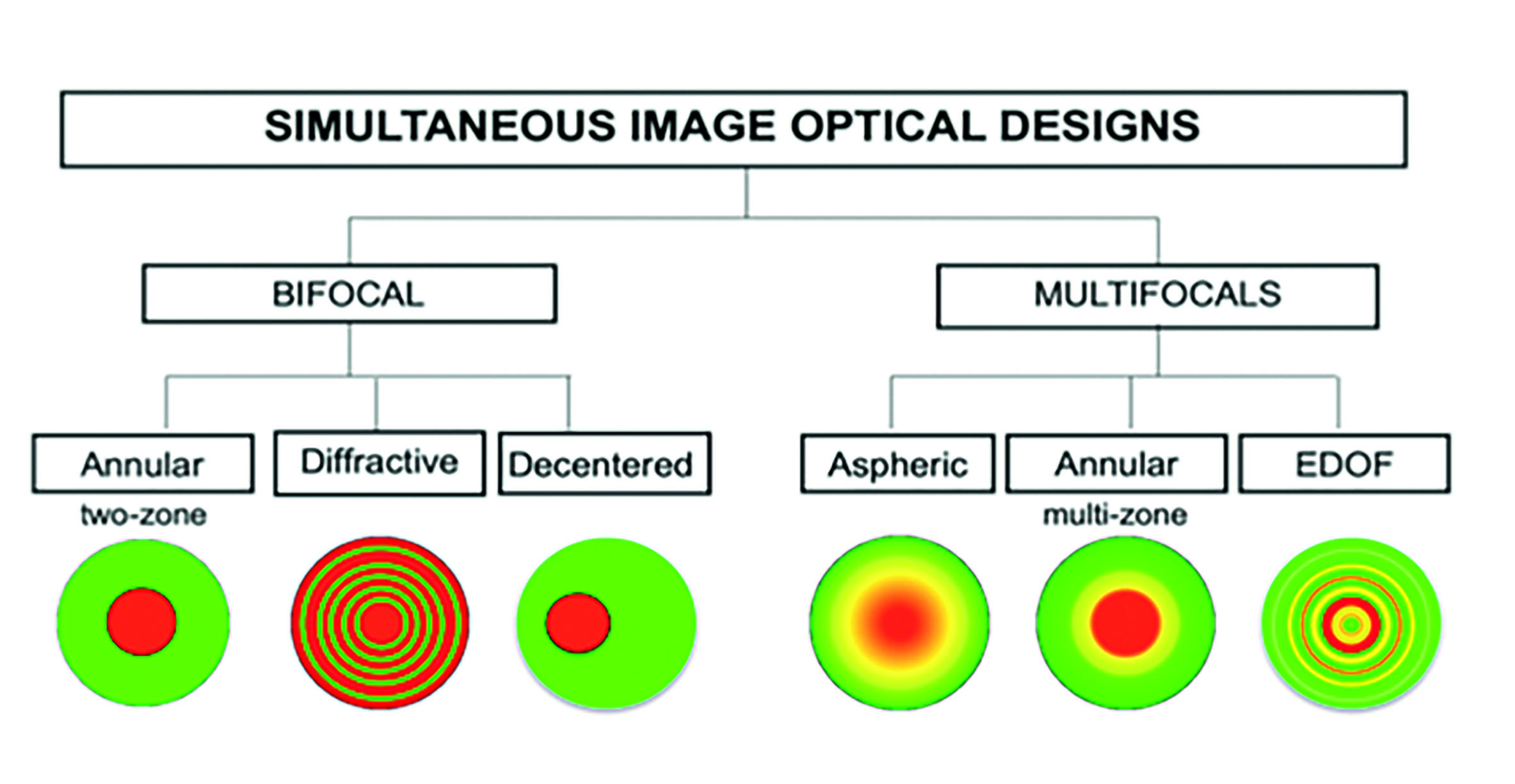
There are several clinical applications for which multi-zone or advanced optical designs are ideal. Most notably, for the correction of presbyopia and retarding progressive myopic eye growth. Although the aims of these designs are quite different, they share common features in terms of how their goals are achieved. In presbyopic designs, additional plus power is provided to supplement the eye’s declining accommodative system. Alternatively, myopic designs, aim to introduce myopic retinal defocus to retard axial eye growth. Theoretically, both of these aims can be accomplished by creating power gradients or zone(s) of varying optical powers. Later, we briefly discuss a sampling of design strategies, some of which are commercially available, whereas others may only be in developmental stages.
Non-rotationally symmetric designs, such as translating designs (where the lens contains distinct distance and near segments and must move on the eye relative to the pupil) can, theoretically, provide good vision as a single optic is in front of the pupil at one time. Such designs, however, are not currently commonly used due to fitting related issues, lack of availability and wearer comfort. Rotationally symmetric designs, therefore, dominate commercially available designs as well as those under investigation.
Rotationally symmetric designs can be of various forms:
Diffractive
Diffractive lenses are designed to specifically introduce half wavelength optical changes between zones, which create constructive interference. The major advantage of this design is that retinal image quality is not affected by variations in pupil size, since all parts of the optic zone contribute equally to both distance and near designs at all times. Disadvantages include reduced contrast sensitivity, dispersion induced halos, chromatic aberration and reduced transmission levels relative to refractive designs. Once available commercially as contact lenses, they are now mainly used in intraocular lenses due to better management of the aforementioned optical effects.
Annular or concentric ring
Annular or concentric ring design lenses consist of alternating concentric zones or rings, which are intended for either distance, intermediate or near vision. These designs are common to some presbyopic correction multifocals as well as myopia control designs. The resulting optics of these lenses is highly pupil-dependent, so centration and pupil size are key.
Aspheric
Aspheric designs provide a gradient power change from the centre of the lens to the edge. Most typically this asphericity is in the form of primary and/or secondary spherical aberration. They can have centres aimed at correcting either distance or near vision. Most presbyopic designs contain a centre near optics and accordingly contain negative spherical aberration (with increasing negative power emanating from lens centre to periphery). A distance centre aspheric design has also been tried for myopia control,5 but no such approved and marketed design is currently commercially available specific to myopia control. Regardless of their application, these aspheric designs typically contain aggressive levels of spherical aberration in order to achieve the required power shifts within reasonable pupil sizes, so as discussed above, are particularly sensitive to physical decentration and can induce high levels of coma into the optical system if not fitted well.
An important note about aspheric designs when being used for presbyopia is that the positive spherical aberrations that are typically present in older patients’ eyes, may somewhat counteract the negative spherical aberrations in the design of centre-near aspheric multifocal lens designs. Therefore, the efficacy of these lenses may be mitigated by the eye’s spherical aberration and may then vary from person to person.6
Extended depth of focus
Extended depth of focus (EDOF) lenses constitute a somewhat ambiguous category of lenses because all multifocal lenses aim to accomplish this outcome. However, this category broadly encompasses lenses that may contain non-monotonic, non-aspheric, and/or aperiodic profiles. In some instances, these designs are broadly similar to aspheric lenses, utilising alterations of spherical aberration to generate their multifocality, but more purposefully including other multiple higher order spherical aberration terms (for example, EDOF and conical surfaces that create axial focus called ‘axicons’). Other designs being explored have unique angular optical elements.
Relevance to practice
- Centration of multifocal contact lens options is key for the patient’s quality of vision.
- Knowledge of contact lens optical design can help align the best design to a patient’s needs, and set patient expectations.
- Visual performance may improve with wear due to neural/blur adaptation.
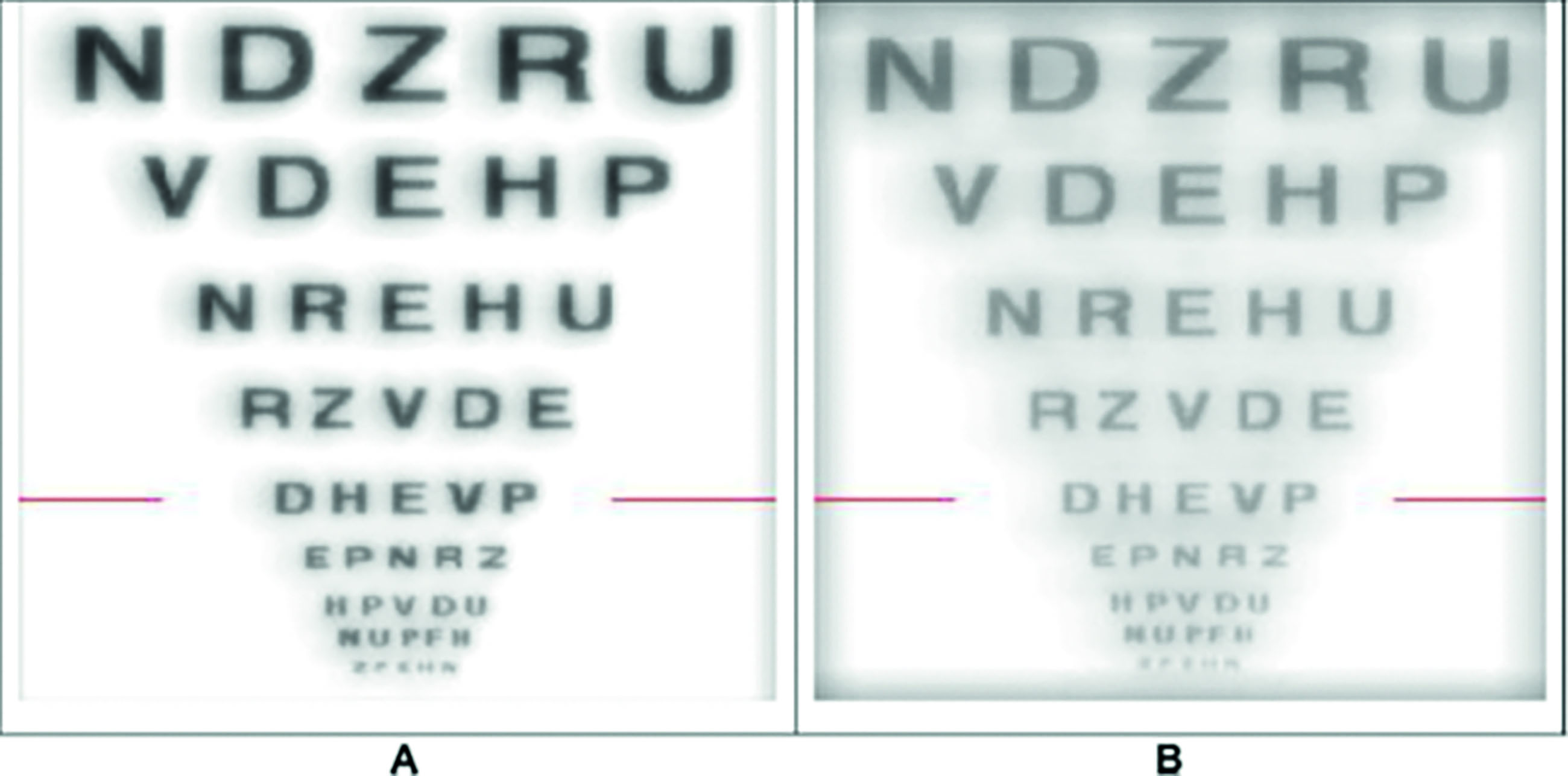
Many of the multi-zone lenses produce multiple images for the wearer (figure 3). In a perfect condition, all the ghost images will be hidden behind the wearer, who may be able to read the smallest letters on the chart. However, most of the lenses decentre from pupil when on-eye. In these instances, the ghosted image will no longer stay behind the focused image and will reduce image quality.
Figure 3: (A) Simulated letter chart (red line denotes 0.3 logMAR) for an aberration-free eye wearing a low-add (for example, 0.3μm spherical aberration at a 5mm pupil diameter) aspheric multifocal lens. (B) Simulation of the same condition as (A) but with the lens decentred 0.5mm
Contact lens metrology
On-eye accuracy is predicated on the valid manufacturing of lenses. Off-eye measurements to verify accurately manufactured lenses can be accomplished in several ways. Simple methods include optical focimeters or the knife-edge technique. These methods only describe limited aspects of the lower order optics and suffer relatively poor sensitivity. Several interferometric techniques are possible to more completely inform about the lens optics (for example, Mach-Zender interferometer, Twyman-Green interferometer, and Moiré interferometer).
Commercially, another interferometric technique, deflectometry, has been implemented in the Nimo TR1504 and has been widely used to measure lenses off of the eye. A very high resolution ptychographic technique (a computational method of microscopic imaging) has also been employed in a device called the PhaseFocus Lens Profiler. Photoacoustic microscopy (PAM) and optical coherence tomography (OCT) are other techniques being explored in laboratory settings. Shack-Hartmann aberrometry has also been employed in several commercially available devices (such as the ClearWave Contact Lens Precision Aberrometer, Omnispect and Optocraft systems). These have become commonly utilised, and have shown good accuracy and repeatability.
Both manufacturers and practitioners also want to know the detailed optical effects of lenses on-eye to know if the desired user optical goals are actually being realised. Although this is commonly clinically done with over-refraction, on-eye optical metrology measures provide significantly more information.7 In particular, the Shack-Hartmann technique has been commercially applied to several instruments, including the Complete Ophthalmic Analysis System (COAS) aberrometer. It was found to have good accuracy, repeatability and dynamic range, and has been successfully applied to many contact lens measures, both on-axis and off-axis. Pyramidal sensing combines images from multiple prisms into one to quantify lens optics. This high-resolution technique has been employed into the Osiris aberrometer and reported to have excellent accuracy and repeatability.
A third alternative for on-eye lens measures is based on ray tracing, or the principle of isolating ray bundles to measure optical deviation. These types of measures have also been found to be accurate, but of lower within-eye repeatability.
As lens designs and the methods to manufacture them become more sophisticated, metrology also needs to advance and expand. Ideally, manufacturers can work to provide clinicians information on the power of their lenses, the assumptions used for verification and the higher order aberration structure of the lenses. Such comprehensive information would allow the clinician the opportunity to enhance their clinical decision-making with regard to the optical designs.8
Simultaneous-image optical designs of contact lenses. Red, green and yellow colours represent the areas for distance, near and intermediate vision, respectively. The annular/zonal and aspheric designs illustrated here have a central distance correction: designs with centre near correction are also available
Relevance to practice
- Focimetry is a simple off-eye method that can be utilised to verify back vertex power, if done with some care (only relevant in low add or simple optics).
- In practice, over-refraction is typically utilised, which is limited to lower order optics.
- In research and manufacturing, more sophisticated equipment helps provide a more comprehensive understanding of lens optical design.
Clinical assessment of optical design efficiency
Visual acuity remains the gold standard technique for clinical assessment of lenses, with logMAR acuities usually performed in research settings. Variable contrast sensitivity testing may offer a more comprehensive assessment of visual performance than just visual acuity, but is often more time consuming, more difficult for the patient, and accordingly less repeatable.
Through-focus or depth-of-focus curves provide a more comprehensive description of visual performance than just a single or a few measures at different viewing distances. They are especially important for understanding presbyopic lens performance. Other measures, such as reading performance or patient-reported outcome measures may also provide further information regarding lens on-eye optical efficacy and allow comparisons over time or between lenses.9 Patient-reported outcome measures should ideally be validated and anchored in some way or otherwise acknowledged that they may provide predominantly patient-specific relative information. More recently, much work has involved gaining insight of the eye’s peripheral refraction with the goal of slowing myopic eye growth. While this technique began primarily as a laboratory-based technique, due to the time, care and equipment required to capture and analyse/interpret these measures, it is being adopted more commonly in the commercial field of myopia management.
Relevance to practice
- Real world visual assessments should be considered rather than dependence on VA measurements alone.
- Patient-reported outcome measures are useful indicators of visual satisfaction and performance.
- Additional tests conducted in research studies may include contrast sensitivity, depth of focus curves, reading speed and aberrometry measurements.
Conclusions and future directions
Technology now allows contact lens optic designs to be manipulated with the aim of achieving several specific goals, ranging from correcting a simple refractive error to optimising vision through aberration management. Such design flexibility is facilitating the creation of lens designs for the retardation of myopic eye growth and allowing an afocal presbyopic eye to see at multiple viewing distances. As we begin to prescribe these lenses, it is essential for us to fully understand these technologies and their underlying optics. Accomplishing the goal to best help our patients will require knowledge and communication of lens optics and teamwork between manufacturers, clinicians and researchers.
- Nitya Murthy, MS, OD is an associate clinical research optometrist at the Borish Center for Ophthalmic Research at Indiana University. Her clinical practice and research interests include myopia control, specialty contact lenses, ocular surface disease and optometric education.
- Steve Newman is Executive Officer, Global R&D & Chief Technical Officer of Menicon Co Ltd. He has more than 40 years of experience in the contact lens industry, particularly in the area of manufacturing and lens design. He holds numerous contact lens-related patents and is interested in smart devices and AR technology, especially regarding how they may impact visual development and functionality.
- Pete Kollbaum, OD, PhD, FAAO, FBCLA is Professor, Associate Dean for Research, and Director of the Borish Center for Ophthalmic Research at Indiana University. He is also Professor (by courtesy) at the Weldon School of Biomedical Engineering at Purdue University. His teaching and research interests include lens design, optics, myopia, presbyopia, eye fatigue and predictive modelling.
- The full report and supplementary information can be accessed at https://doi.org/10.1016/j.clae.2021.02.005
- The BCLA CLEAR Summary report is a short bite-size evidenced based practical guide for clinicians, bringing together the key findings from the report. Accessed via CLEAR (bcla.org.uk)
- The editors for this series are Neil Retallic and Dr Debarun Dutta
Acknowledgements
Acknowledgement and recognition to Kathryn Richdale, Ian Cox, Pete Kollbaum , Mark A Bullimore, Ravi Bakaraju, Paul Gifford, Sotiris Plainis, Curt McKenney, Steve Newman, Erin S Tomiyama and Philip Morgan who were the paper’s authors and the educational grants from Alcon and CooperVision.
Original paper: Richdale, K; Cox, I; Kollbaum, P; Bullimore, MA; Bakaraju, RC; Gifford, P; Plainis, S; McKenney, C; Newman, S; Tomiyama, ES; Morgan, PB. CLEAR - Contact lens optics. Contact Lens & Anterior Eye. 2021, 44 (2):220-239.
References
- Richdale K, Cox I, Kollbaum P, Bullimore MA, Bakaraju RC, Gifford P, et al. BCLA CLEAR – Contact lens optics. Contact Lens and Anterior Eye 2021;44(2):220-39. https://doi.org/10.1016/j.clae.2021.02.005.
- D’Souza S, Annavajjhala S, Thakur P, Mullick R, Tejal SJ, Shetty N. Study of tear film optics and its impact on quality of vision. Indian J Ophthalmol 2020;68(12):2899-902. https://doi.org/10.4103/ijo.IJO_2629_20.
- Thibos LN, Ye M, Zhang X, Bradley A. Spherical aberration of the reduced schematic eye with elliptical refracting surface. Optom Vis Sci 1997;74(7):548-56. https://doi.org/10.1097/00006324-199707000-00024.
- Erickson P, Robboy M. Performance characteristics of a hydrophilic concentric bifocal contact lens. Am J Optom Physiol Opt 1985;62(10):702-8. https://doi.org/10.1097/00006324-198510000-00006.
- Cheng X, Xu J, Chehab K, Exford J, Brennan N. Soft Contact Lenses with Positive Spherical Aberration for Myopia Control. Optom Vis Sci 2016;93(4):353-66. https://doi.org/10.1097/opx.0000000000000773.
- Pettersson A, Jarkö C, Alvin A, Unsbo P, Brautaset R. Spherical aberration in contact lens wear. Contact Lens & Anterior Eye: The Journal of the British Contact Lens Association 2008;31:189-93. https://doi.org/10.1016/j.clae.2008.05.005.
- Dorronsoro C, Barbero S, Llorente L, Marcos S. On-Eye Measurement of Optical Performance of Rigid Gas Permeable Contact Lenses Based on Ocular and Corneal Aberrometry. Optometry and Vision Science 2003;80(2):115-25. https://doi.org/10.1097/00006324-200302000-00007.
- Papas E, Wolffsohn JS, Jones L. Innovation in contact lenses: basic research and clinical science. J Optom 2010;3(3):123-4. https://doi.org/10.1016/S1888-4296(10)70017-0.
- Tilia D, Munro A, Chung J, Sha J, Delaney S, Kho D, et al. Short-term comparison between extended depth-of-focus prototype contact lenses and a commercially-available center-near multifocal. J Optom 2017;10(1):14-25. https://doi.org/10.1016/j.optom.2016.04.003.
