This is a genetically determined, heterogeneous group of conditions characterised by failure of normal synthesis of melanin and reduced pigmentation in the skin, hair and eyes. Albinism has historically been classified according to the site and severity of melanin deficiency:
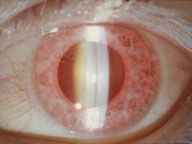 Oculocutaneous albinism - hair, skin and eyes are affected. Tyrosinase-negative oculocutaneous albinism is an autosomal recessive condition with complete absence of melanin. Tyrosinase-positive patients synthesise variable amounts of melanin. Their complexion varies from very fair to normal; eye involvement is also variable.
Oculocutaneous albinism - hair, skin and eyes are affected. Tyrosinase-negative oculocutaneous albinism is an autosomal recessive condition with complete absence of melanin. Tyrosinase-positive patients synthesise variable amounts of melanin. Their complexion varies from very fair to normal; eye involvement is also variable.
Ocular albinism - decreased ocular pigment only. The skin and hair appear essentially normal, although all albinos have some degree of hypopigmentation. Inheritance is usually X-linked recessive.
Register now to continue reading
Thank you for visiting Optician Online. Register now to access up to 10 news and opinion articles a month.
Register
Already have an account? Sign in here
