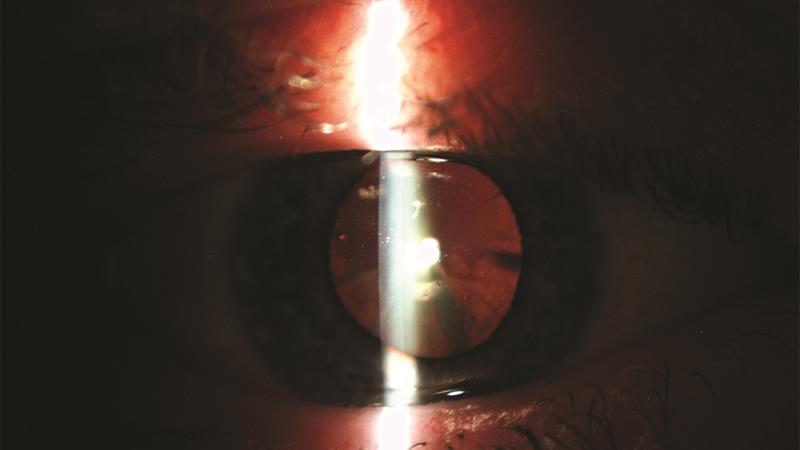
Cataract referral (C60317)
You were asked to discuss the advice you might give to a patient with early cataract and what might influence a decision to refer them.
Most responses reflected the importance of a clear explanation of cataract, the implications both at the time of assessment and in future, and any changes that might be considered to help the vision at this consultation.
One example of advice if referral was not deemed relevant included, ‘to try wearing tinted spectacle lenses for day time driving to improve comfort, and then to review at an interval of less than that between the previous two tests. We would advise that a nuclear cataract often develops quite slowly, but that the rate of growth is variable between individuals.
If the patient was a smoker we would recommend that he seek help to stop smoking. We would predict a very gradual deterioration in the patient’s vision over time, and explain that eventually cataract surgery might be required to keep his visual acuity within the legal driving standard, but we would explain that he was within the legal driving standard at the moment.’
With regard to referral your responses reflected well some of the variations in local protocols. For example, ‘If he was keen to have the surgery, I would refer him via his GP. I practice in Hampshire and have three local hospitals, which will all accept cataract referral, regardless of acuity, if the patient and optometrist have discussed this in detail and both feel that cataract surgery should be investigated further. I would then send a GOS 18 to the GP and give the patient a copy. The patient would then be advised to contact the GP and arrange referral over the phone or in person, depending on the individual GP. I always ask patients if they have private insurance, or whether they would like to go privately. This speeds up the whole process and also means there is a greater choice of lens implants. I discussed this case with an optometrist who practises in East Sussex. We agreed that we felt surgery would be the best option. However, her local protocols are different. She would suggest he went privately, especially if he had private insurance. She is not able to refer patients routinely to the NHS if their VA is better than 6/12. However, in this case, she would try an NHS referral as the cataract appears to be developing quickly and he is relatively young. To do this she would send a CAQ (cataract assessment questionnaire) to the GP stating her reasons for the referral. In summary, we would both refer, if that is what the px wanted but our referral processes would be different.’
More typical answers included: ‘Referral by the optometrist to the cataract surgery provider is via the GP and takes into account all visual symptoms, patient’s lifestyle and patient’s desire for surgery.’ Another stated: ‘The process for referral in my area is a points assessment where the patient is scored based on the visual acuity, clinical modifiers such as presence of posterior subcapsular cataract, or other ocular pathology. It also considers the impact the reduced vision has on the patient’s life and their ability/comfort driving. With this patient we discussed that the current VA would probably not qualify them for a referral but the other clinical and lifestyle impairments would certainly increase the score, we would offer this to the patient, if they still did not qualify we would monitor them on a six-month or one-year recall depending on how close they were to qualifying.’
And another, ‘I would ask whether his reduced vision is causing any further problems with his lifestyle, work, hobbies, etc. I would explain that his vision is still pretty good, and most surgeons would not be interested in operating at this stage and although a cataract op is very straightforward and causes very few complications there are still risks attached so I would not advise an op at this stage until or unless it got worse. I would ask if he was OK with this (99% would say yes). I would see him again in one year unless he noticed further deterioration in the meantime and in which case to come back sooner. For the 1% who say no and they say they really need clearer vision for their work or sport I would then refer. The procedure in Sheffield is direct referral and Sheffield has just set up a new cataract department in a different hospital – a one stop service that speeds up procedures and there is Spa Medica in Sheffield that does NHS cataracts and has only a two-week waiting list. I am an accredited post cataract op optometrist and can undertake their postoperative checks. If he was very keen for the op I would probably send him there as they would be more likely to operate at this stage. Without further symptoms I would not refer. I would explain it is likely to get worse but it can take a while to develop to the stage when it needs operating.’

A very few responses seemed to be confused about the role of NICE (‘we would not refer as he does not meet the new revised NICE guidance levels for referral’) and were asked for clarification on this.
Myopia Therapy (C60318)
For a six-year-old myopic child with both parents known to have moderate myopia, your were asked for your views on mentioning options for management other than spectacle correction and how you might explain myopia control to parents.
Most responses seemed very open and supportive of mentioning myopia control to the parents and child. Here are some examples of the discussion outcomes from participants.
‘At this stage, it would be an ideal time to suggest the option of myopia control with the parents. An obvious question from the parents will about future progression of their son’s myopia given that they are both moderate myopes which would make them sensitive and understanding to the condition. Correction is obviously required at this stage, with the option to try to keep it under control at this early stage as he is just at the ideal stage to intervene. I would suggest to the parents to look at the clinical evidence, maybe giving them some literature to support this. This is when I would suggest the contact lens option. I would tell them that myopia control is not a cure all but to help the correction progressing which I’m sure they will both appreciate. The parents may be already contact lens wearers themselves so if they are they will be aware of the practical benefits, if they are not, I would show them all a soft lens to give them an idea as to how they handle. I would give them the option of spectacles, and offer a free contact lens assessment with a discussion on the ongoing costs, which is an important consideration for them. The important thing is to keep and the explanation as simple as possible as regards myopia control and I would think if they are shown the research-based evidence I am sure this is an option they would consider as after all I’m sure they would probably have been grateful if it was available to themselves when they were children.’
Here is another, which begins with an honest declaration, ‘Up to date I have never mentioned myopic control to any patient/parent with the exception of increasing outdoor activity. Simply prescribing spectacles and reviewing usually every six months.’ They then continue: ‘Initially, I would discuss myopic control in as simple terms as possible. Given that mum and dad are both myopic I would relate their own experiences with the progression of myopia with the likely progression of their children’s myopia. I would then discuss the effect of outdoor light and explained that there has been a large amount of continuing research into what affects myopic progression. At this stage where the myopic control contact lenses would not be fitted and thus the decision for the parents would not be made on that day I would introduce the idea that ‘when their child was a bit older say two or three years’ time, they could consider contact lenses for their child which would probably be able to reduce the overall level of myopia for their child.’
A nice summary explanation of options was, ‘Myopia occurs when the eyeball growth is such that it increases in length front to back, and although standard spectacles/contact lenses can be prescribed to compensate for this, the process of elongation can continue if the spectacles/contact lenses cannot fully control the position of the images formed on the back of the eye, in both the central and peripheral area of the eyeball. As standard spectacles/contact lenses can only easily control image positions in the central part of the eyeball, it requires more specialised lenses (normally in the form of soft daily disposable contact lenses) to provide the correction in both the central and peripheral areas. These specialised contact lenses are a multifocal lens where the lens power changes from the centre of the lens to edge, to give the optical control required for the myopia control, but in every other respect the lenses can be handled like any other daily disposable soft contact lens. Other options to mention for myopia control would be to explain to the parents how the use of rigid gas permeable contact lenses worn overnight can modify the shape of the corneal surface and, in turn, control the myopia. Given the age of the patient it would be the soft daily disposable lens that would be recommended as a lens of first choice. Regular follow- up appointments would be scheduled to monitor the refraction initially two three-month check-ups, then six-monthly thereafter.’
Some important points emphasised included: ‘The most important part of the discussion in this situation is the active involvement of the child and parents in the discussion, and for the actions taken in correcting the child’s vision and managing their myopia are deliberate – not passive.’
Great responses and discussions all round.
