World Glaucoma Week draws to a close tomorrow, and I hope this annual event continues to spread information about this common cause of blindness by encouraging across the board activities spreading awareness. Over the past few weeks we have run several features looking at screening for ocular hypertension and primary open angle glaucoma, as well as an article summarising current medical management of the disease.
Over the past couple of years there have been two interesting and significant developments in glaucoma world, both with strong UK links. I thought it might be timely to offer a recap of these as, despite a brief flurry of interest in the national press, both since received little publicity despite their potential significance in future glaucoma prevention.
Early detection
All readers will be familiar by now with the various indicators that need to be established when deciding whether a patient is at risk of developing glaucoma. The slow and insidious nature of primary open angle glaucoma progression means the disease is very rarely self-reported as a problem and so early detection requires a careful evaluation of a number of factors. Then a decision needs to be made about closer monitoring or medical intervention to stop further disease. This management may hinder progression, but cannot (yet) rectify previous damage, and so the earliest detection and intervention is a major goal for clinicians.
It is a depressing thought that, at present, most established ways of screening for glaucoma are less than perfect. Visual fields assessment is the mainstay of most community practitioners, but it is worth remembering that this is a subjective response test and therefore inherently less than perfect. Worse still, it is well known that anything up to 40% of retinal nerve fibres are lost before repeatable field loss is detectable. Raised intraocular pressure is a glaucoma risk factor but tonometry is by no means diagnostic. OCT assessment of structural change is increasingly impressive but is still simply indicating established damage.
The fact that there are a number of risk factors of known significance (many of which are as yet non-modifiable – table 1) and a further list of clinical measurements (table 2) that may indicate glaucomatous disease has made it possible for some researchers to use a Bayesian algorithm in an attempt to make primary screening and secondary monitoring or management more efficient.1,2 I would expect such algorithm driven technology to soon impact in care pathway decision-making and this be reflected in better referral accuracy.
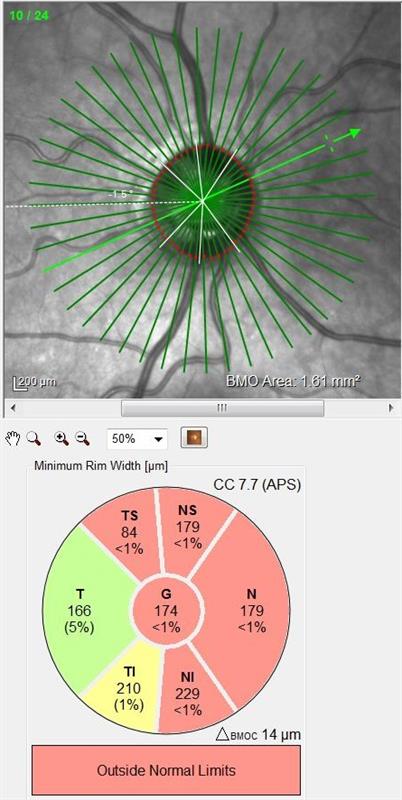
Figure 1a: OCT has improved the ability to detect disc changes
As outlined in the tables, an understanding of risk factor influence and accuracy of clinical data gathering has improved over the years, though there have been too few new techniques introduced for improved detection. That may change.
Detection of apoptosing retinal cells (DARC)
A new test is being investigated in research centres in London and centres around the detection of cell in the retina undergoing apoptosis – hence its rather catchy name, thankfully reducible to the catchier acronym DARC.
Apoptosis is a natural process that takes place in living cells and describes the pre-programmed sequence that terminates the life of any living cell. This helps establish a set lifespan of maximum healthy function and extinction before dysfunction occurs and limits the risk of toxic by-products affecting surrounding tissues. If degradation of cells over time, through the impact of intrinsic activity and the influence of external agents were not a concern, then the removal of apoptosis might lead to eternal life, though here I may be drifting off into science fiction territory.
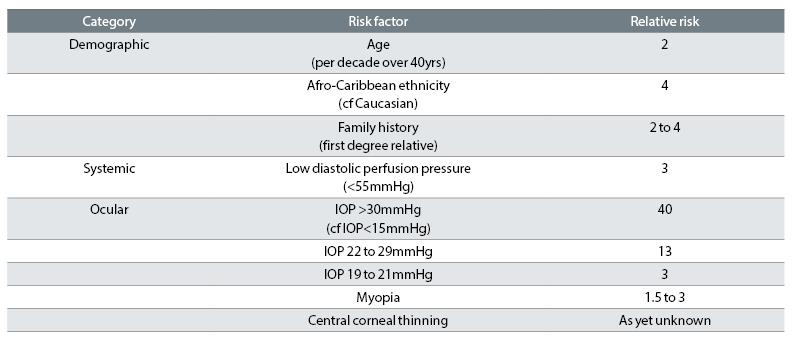
Table 1: Risk factors significantly associated with POAG3
Glaucoma is the leading cause of irreversible blindness worldwide and is attributed to the death of retinal nerve cells, specifically, retinal ganglion cells (RGCS). Indeed, it is the selective impact of apoptosis upon RGCs that is now considered to be the very first indication of glaucomatous neuropathy. Therefore, any way of detecting this process by means of a sensitive but practical test might allow clinicians to suspect the disease right at the start of its progression and before significant damage has occurred.
The DARC technique centres on the use of a dye, annexin 5, which can be injected into an eye and which then attaches to any retinal ganglion cells. Any RGCs to which the annexin has attached that are currently undergoing apoptosis will change the dye and cause it to fluoresce.4
The fluorescence of even single RGCs can be detected by confocal scanning laser ophthalmoscopy (something increasingly found in optometry practices) making this a sensitive and simple test. Even more significant, researchers are confident the dye will be available in a drop form in the near future. Surely this will impact on our profession and should see the focus of glaucoma screening move away from tonometry and fields. Might we be realistic in expecting pre-screening in the future to include the instillation of a drop before retinal imaging takes place?
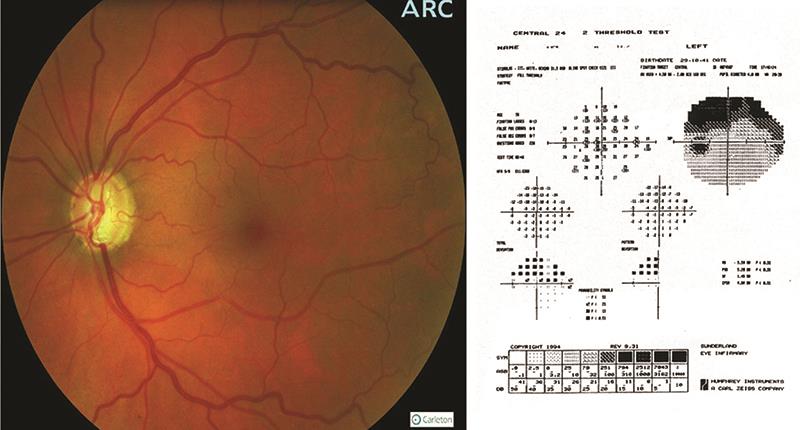
Figure 1b: Ophthalmoscopy and fields often detects disease after significant irreversible damage has already taken place
Further studies will now be carried out into DARC and how it could be used to detect other neurodegenerative conditions, such as Parkinson’s and dementia states, where increasing numbers of nerve cells are lost as the disease progresses.
Neuroprotection
As discussed, glaucoma involves the loss of retinal ganglion cells.
The demise of these RGCs involves a pathway of inflammatory processes which are only recently becoming clear to researchers. If this process was fully understood, then might it be possible to interfere with it in a bid to maintain RGC health and so halt glaucomatous progression?
This thinking has been at the heart of some exciting new research from a team based in research centres in Toronto and California, and including ex-Brit optometrist Professor John Flanagan. A key breakthrough in this area has been understanding the relationship between RGCs and astrocytes. Astrocytes are star-shaped cells (hence the name) found throughout the central nervous system and have a wide variety of functions ranging from axon guidance and synaptic support to the control of the blood brain barrier and blood flow.5
With relevance to glaucoma, astrocytes appear to have a neuroprotective role and help maintain RGC health and activity after insult, such as through injury or disease processes such as ischaemia. They are able to offer this protection as they surround the axons of RGCs where they are known to secrete lipoxins. Lipoxins are small pro-resolving lipid mediators found in the omega-6 inflammation pathway along with prostaglandins. Prostaglandins (or drugs analogous to them), as we already know, can play an important role of treating glaucoma. When there is insult to RGCs, as may be the case during early glaucomatous disease, the astrocytes cease to secrete lipoxins and so neuroprotection is lost.
Lipoxins are found throughout the body, and are found as either type A or B, and mediate in inflammation and protect neurones (neuroprotection). It has been found that type B4 lipoxin, which is secreted by astrocytes, has a more potent neuroprotective effect than type A. Furthermore, both endogenous and aspirin-triggered lipoxins have been shown to reduce inflammatory pain processing through effects on astrocytes, so implying the possibility that externally introduced lipoxin may promote neuroprotection.
The exciting research by Flanagan and co-researchers has looked at this neuroprotective mechanism in mice.6 Their results seem to confirm the neuroprotective role of type B4 lipoxin and its presence is able to maintain the healthy functioning of RGCs in conditions of chronic injury simulated by increased intraocular pressure.
Though much work needs to be done, and indeed extended to human eye models, this does seem to suggest the possibility of an externally introduced agent that may protect the RGCs and so stop glaucoma in its tracks. How wonderful it will be when the statement ‘at present, the mainstay of treatment is to lower intraocular pressure’ becomes out of date.
Table 2: Clinical data indicators
- Goldmann applanation tonometry
- Disc assessment:
- OCT disc analysis, ganglion cell complex analysis, RNFL analysis
- Stereo viewing and imaging of the disc
- Contact and anterior OCT pachymetry
- Corneal hysteresis analysis
- SITA fast 20-4 Humphrey visual fields analysis
- Gonioscopy and anterior OCT of anterior angle
References
1 JC Gurney, E Ansari, D Harle, N O’Kane, RV Sagar and MCM Dunne. Application of Bayes’ to the prediction of referral decisions made by specialist optometrists in relation to chronic open angle glaucoma. Eye, https://doi.org/10.1038/s41433-018-0023-5
2 W Harvey. Getting an intelligent second opinion. Optician, 08.06.2018, pp 32 to 33.
3 Spry P, Harper R. Essential Glaucoma Handbook. Edited; Harvey W. Optician Publications, 2010
4 Cordeiro M et al. Real-time imaging of single neuronal cell apoptosis in patients with glaucoma. Brain, 2017: 140; 1757–1767
5 Liddelow S, Barres B. SnapShot: astrocytes in health and disease. Cell. 2015;162(5):1170–1170.e1
6 Izhar Livne-Bar, Jessica Wei, Hsin-Hua Liu, Samih Alqawlaq, Gah-Jone Won, Alessandra Tuccitto, Karsten Gronert, John G. Flanagan, Jeremy M. Sivak. Astrocyte-derived lipoxins A4 and B4 promote neuroprotection from acute and chronic injury. Journal of Clinical Investigation. 2017;127(12):4403-4414.
