Now more than two years in the making and about to enter a third and final public consultation, the Education Strategic Review (ESR) has stoked healthy debate throughout the profession. Changes, potentially ranging from therapeutic prescribing training to a more clinical practice, could be implemented by September 2020.
As optometry embraces more enhanced services and dispensing opticians take on more responsibility, the regulator has accepted that fast emerging education courses must move with the times.
GOC chair Gareth Hadley said: ‘It has been the elephant in the room for optics for some time. It’s not just that we’ve been trying to push the door open, there are also lots of people pulling from the other side.’
Council members at the regulator’s quarterly meeting this month were asked for their views on proposed new standards for providers and new learning outcomes for optometrists, dispensing opticians and contact lens opticians.
‘I think this is a really positive thing as it really affects people on the front line,’ said Dr Scott Mackie. ‘It is an exciting time and we are entering a new era.’
The overarching theme of the education review has been to better equip future professionals, beginning with universities but extending to CET. Moving towards a CPD model, therapeutic prescribing, and embedding clinical experience at an earlier stage has all gained strong traction in initial consultations.
Alistair Bridge, GOC director of strategy, said: ‘We want to ensure optical students are better prepared for their roles professionally as the optical professions change fast in the face of new technology, pressures on eye care changes and an ageing population.’
Council members were impressed last week by the amount of evidence gathered so far. This traced back to a call for evidence in late 2016, research into patterns and trends in health professional education in November 2017 and then perceptions of newly qualified practitioners in June 2018, all before a consultation on the concepts and principles before spring of this year.
A final public consultation has been earmarked for next month, following round-the-table feedback at 10 Old Bailey.
Dr David Parkins said: ‘The decision to spend more time developing this was the correct thing to do. This is going to be one of the most important consultations in the ESR process.’
Council member Selina Ullah added: ‘It’s not a done deal yet and this will allow people to provide their input once again.’
New learning outcomes
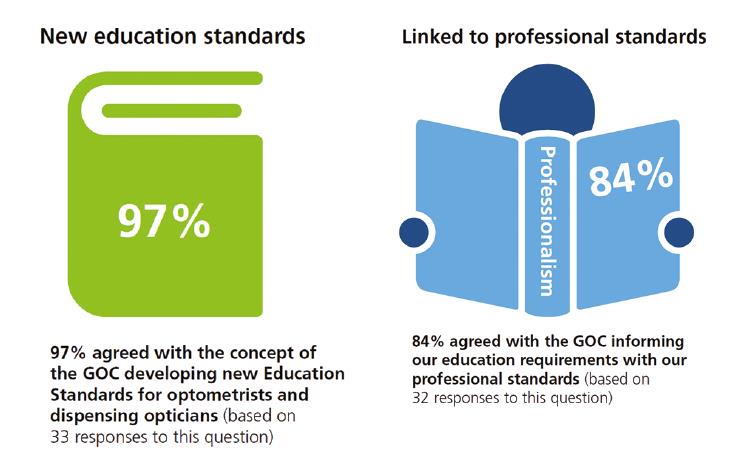
During the education review, the GOC has gained support for the development of new education learning outcomes which all optometry and dispensing optician education providers would be required to deliver.
It followed perceived deficiencies in the current, competency-based framework.

‘For a long time competencies have been the be all and end all,’ said optometrist Helen Tilley. ‘Optometrists need to know it isn’t a problem not to know everything and that they can use their mentors.’
Optometrist council member Josie Forte added: ‘We have seen a shift in people towards a lifelong learning approach, which is ever so important. It does make you wonder about the term “fully qualified” so there are some interesting side points.’
Multi-disciplinary learning was also flagged as having ‘significant value’ across different settings. Meanwhile, an expected move towards more clinical content within courses meant universities taking on more responsibilities for the end product. It was unclear what impact this may have on the length of undergraduate courses.
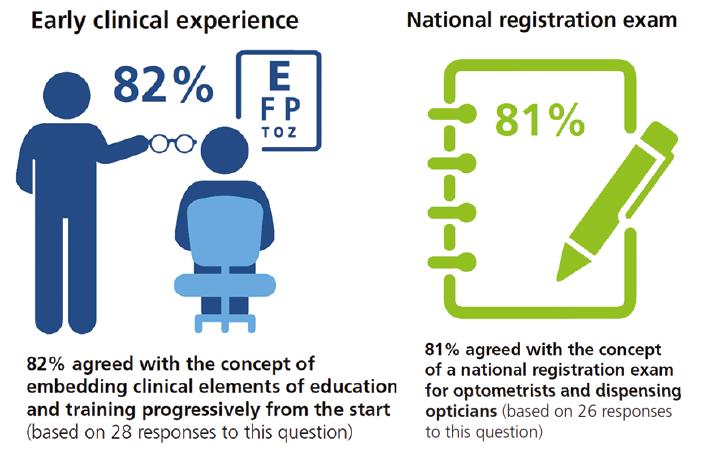
In the latest Perceptions of UK optical education report in June, the GOC found 60% of optometrists believed the amount of clinical experience gained during academic study was too little. It was often confined to the final year of study and ‘did not reflect real-life practice’.
Clinical skills and experience with patients and eye examination techniques were seen as most relevant. Nevertheless, a total of 89% of newly qualified practitioners surveyed felt prepared overall for professional practice when they started their first role.
The report, based on interviews with 35 newly qualified optical professionals, also found 84% felt prepared to practise autonomously and independently, 81% prepared to make confident clinical decisions, and 72% able to adapt to relevant, emerging and new technology.
‘Employer interviewees also highlighted their perception of a drop in the confidence of newly qualified practitioners following qualification, resulting in avoidance of clinical decision-making and a tendency to over-refer. However, some explained that this was to be expected initially and decision-making improved with experience. They encouraged their staff to check referrals with colleagues first to reduce false-referrals,’ it added.
New standards for providers
Prior to the council meeting, the GOC had met with providers to discuss how the review may help evolve standards. A focus on the quality of learning environment, the development of new programmes as well as teaching and development of sufficient supervisors all came to the fore.
Hadley said: ‘The onus will be on the providers to show us the ways they have set out to meet these standards.’
A more outcomes-based approach would provide education providers with flexibility about how to meet standards, and they would be asked to demonstrate how they have chosen to do so.
Bridge said: ‘The draft standards are focused on outcomes to allow greater flexibility for education providers and encourage innovation. They will need to be accompanied by a robust approach to accreditation and quality assurance but we hope this new flexibility will make it much easier for providers to prepare students to meet the demands of patients in the future.’
The draft standards for providers covered patient safety and professionalism, safe and accessible learning, access to early, frequent and varied clinical experience, developing and delivering curricula and delivering value for students, patients and employers.
Meanwhile, learning outcomes for optometrists covered three separate domains of ‘being a knowledgeable and skilful clinician and scientist’, ‘a trusted eye health and vision professional’, ‘safe and competent practitioner’, and a ‘collaborative and effective colleague and manager’. New learning outcomes for CET were also proposed.
A significant addition to these skills was to understand and apply knowledge of pharmaceuticals, pharmacology and microbiology to patient care, plus the principles of independent prescribing and the legislation relating to the use and supply of exempt and controlled drugs.
Council approved these outcomes, together with the proposals to adopt the Royal Pharmaceutical Society Competency Framework for all Prescribers.
‘This throws down some significant challenges for providers developing the final product,’ added Hadley.
Indeed, the final phase of the GOC’s education review has unveiled more detail but also identified the challenges to be resolved. With a firm resolution due by February next year, the education elephant is now well and truly making its way across the room.



