
The use of drugs to manage myopia presents a number of challenges. These include the potential impacts of long-term drug metabolism and excretion, concerns about adverse effects, issues related to compliance and accurate dosing, visual compromise during therapy, patient discomfort, and the possibility of rebound effects upon therapy cessation. However, the use of topical agents, in particular the anti-muscarinic drug atropine, has been found to be an effective way of limiting myopic progression and, in recent years, changes to the concentration, formulation, mode of administration, treatment protocol and the introduction of new drug therapies all indicate that a pharmaceutical approach is likely to be an important part of the practitioner’s approach to myopia management in practice.
Atropine
The use of atropine, especially in a low dose formulation, appears still to be the first choice myopia treatment among paediatric ophthalmologists.1 Though this is likely, at least in part, related to established professional approaches to disease, most argue the reason for adopting atropine is the impressive slowing of the myopic refractive error over time as shown in the first big studies of the treatment.
Atropine acts as a competitive antagonist at both peripheral and central muscarinic cholinergic receptors. In the eye, these receptors are found both on the ciliary muscle and the iris sphincter muscle, and are normally activated by acetylcholine under the control of the parasympathetic nervous system. Acetylcholine causes pupil miosis and ciliary contracture, so blocking the receptors with atropine results in cycloplegia and mydriasis.
Atropine, in the 1% and 2% concentrations used for cycloplegia, has a much stronger bond to receptor sites than other available anti-muscarinics, such as cyclopentolate or the weaker still tropicamide, and so its action takes several days to initiate and lasts for up to two weeks. Because of its potential toxicity, atropine has, for some years now, only been available to additional supply or independent prescribing optometrists in the UK.
That deep, prolonged cycloplegia helps in reducing myopia progression has been known for some time. Donders was the first to recommend atropine as a treatment for myopia when he suggested it for suspected spasms of accommodation in myopic patients, way back in 1864. In recent years, its usefulness as a myopic therapy has been focused upon the impact of using lower dose concentrations in an effort to minimise the significant, and potentially harmful, side effects of the drug. The two key studies to have heard of are:
- ATOM2; this concluded that atropine 0.01% eyedrops were more effective in slowing myopia progression with fewer visual side effects when compared with higher concentrations.2 It was also found that ceasing treatment resulted in a 60% rebound increase in myopia among eight to 10-year-olds, though the rebound decreased with increasing age at the point of cessation.
- LAMP; this study concluded that 0.05% atropine should be used, rather than 0.01%, as the lower concentration allowed unacceptable levels of axial length progression.3
To summarise, lower concentrations of atropine reduce the impact of mydriasis and cycloplegia upon vision during treatment and minimise systemic adverse responses. However, too low a dose, for example the 0.01% of ATOM, may show good refractive change but less impact upon axial length. LAMP shows us that 0.05% has better impact on axial length growth and so fewer myopia complications in adult life.
Measuring Success
The best predictor of future myopia is the refraction. That said, once myopia is suspected or confirmed, the best measurement for monitoring myopic progression is the axial length. For a clear explanation of this, I highly recommend a recent paper by Noel Brennan, available as a free download.4 Treatments that primarily influence the anterior anatomical structure, so atropine and orthokeratology, are found to have immediate impact upon slowing the myopic refractive error but this is not reflected in a corresponding reduction in axial length growth. This is also why these treatments show the greatest rebound upon cessation.

So, at present, it is reasonable to conclude that 0.01% atropine provides little more than a moderate slowing of refractive progression or, in effect, a partial correction. The same applies to alternative anti-muscarinic drugs known to have fewer side effects, such as 2% pirenzipine.5 The LAMP study, on the other hand, showed that doses higher than 0.01%, notably the 0.05%, had much greater impact upon the axial length (figure 1) and so this formulation still holds promise as a myopia therapy with good long-term benefit while maintaining a low adverse response profile.
Studies Currently Under way
It seems, therefore, that we need to know more about pharmaceutical impact based upon the impact of drugs upon axial length growth as this is now established as more relevant than refraction in monitoring the effectiveness of myopia therapies. So there are a number of studies currently under way which are worth knowing about and which do monitor axial length:
- CHAMP-UK; a multicentre study in the UK looking at 0.01% atropine over two years and the five-year impact based on cycloplegic refraction and axial length. Due to report in December 2021. A US-based CHAMP study, using a novel low-dose atropine preparation called NVK-002, is expecting results in August 2023.
- PEDIG; two-year US-based study looking at 0.01% atropine use and monitoring axial length. Due to report in September 2022.
- MOSAIC; Irish study using 0.01% atropine over two years followed by a one year wash out and including axial length measurement. Reporting in May 2023.
- STAAR; a large US study using another new atropine preparation with apparent greater stability known as SYD-101 and including axial length assessment.
Microdosed Atropine
At the American Academy of Optometry conference at the end of last year, further details were released of the CHAPERONE study (figure 2). This study from SUNY is using a novel microdosing atomiser developed by Eyenovia called the MicroPine. The hope is that the ease of use of this unit dosing spray will allow easy self-dosing by children, so improving compliance and allowing the use of 0.1% atropine (likely to have better axial length growth limitation) to be better regulated. The dispensers can be used with a Wi-Fi link to ensure continual data gathering and monitoring of patient behaviours. Definitely one to watch out for.
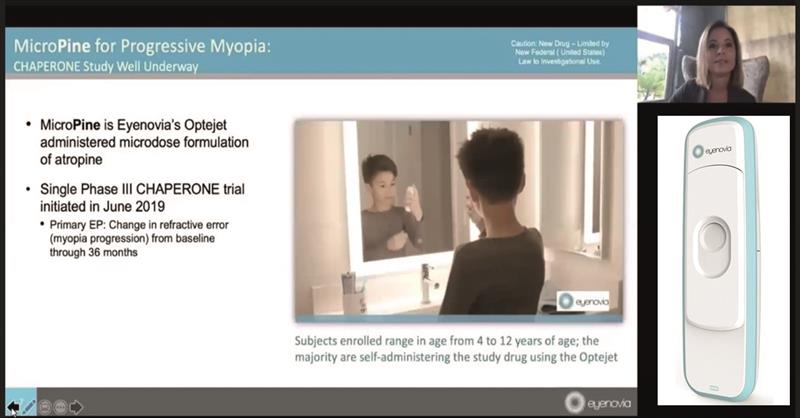 Figure 2: Online discussion of the MicroPine at the 2020 AAO online conference
Figure 2: Online discussion of the MicroPine at the 2020 AAO online conference
Other Drugs
A recent review of the many and various drugs that have been tried to limit myopia concluded: ‘Presently, only atropine, pirenzepine and 7-methylxanthine are shown to reduce myopia progression in human trials.’6 The paper is worth a look just to see the surprising number of drugs have been tried.
7-methylxanthine is an adenosine receptor antagonist and an intermediate metabolite in the synthesis of caffeine. It is interesting in that it may be administered orally but, so far, its myopic influence is mainly based on animal models. Might be one for the future perhaps?
Conclusion
The main conclusion regarding pharmaceutical approaches to myopia has to be that there is still much research to be completed. Initial excitement over the impressive response to atropine, and indeed orthokeratology, as measured by refraction have been somewhat tempered by reports of significant rebound after treatment ends. Also, the refractive impact of lower dosing is not reflected in axial length change, something now increasingly argued to be key parameter in monitoring success of treatment.
It is most likely that atropine becomes an adjunct treatment to complement existing therapies such as orthokeratology or contact lenses.
References
- Zloto T. et al. Current trends among pediatric ophthalmologists to decrease myopia progression—an international perspective. Graefe’s Archives of Clinical and Experimental Ophthalmology, 256 (2018), pp. 2457-2466
- Chia A et al. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (ATOM 2). Ophthalmology, 119 (2012), pp. 347-354
- Yam JC et al. Low-concentration atropine for myopia progression (LAMP) study: a randomized, double-blinded, placebo-controlled trial of 0.05%, 0.025%, and 0.01% atropine eye drops in myopia control. Ophthalmology, 126 (2019), pp. 113-124
- Brennan NA, Toubouti YM, Cheng X, Bullimore MA. Efficacy in myopia control. Progress in Retinal and Eye Research, 2020,100923
- Siatkowski RM et al. Two-year multicenter, randomized, double-masked, placebo-controlled, parallel safety and efficacy study of 2% pirenzepine ophthalmic gel in children with myopia. JAAPOS, 12 (2008), pp. 332-339
- Vutipongsatorn K, Yokoi T, Ohno-Matsui K. Current and emerging pharmaceutical interventions for myopia. British Journal of Ophthalmology, 2019 Nov;103(11):1539-1548
