
Eye health rarely figures in the literature regarding the Covid-19 disease, but it is more than likely that we will see more and more ocular consequences of the disease and its treatment in the coming year. Here is a brief summary of what we currently know.
Transmission
One of the first providers to voice concerns regarding the spread of coronavirus in Chinese patients was Dr Li Wenliang, an ophthalmologist. He later died from Covid-19 and was believed to have contracted the virus from an asymptomatic glaucoma patient in his clinic. This, plus the high incidence of viral conjunctivitis in patients with Covid-19 (figure 1), initially led to some serious concerns about the risks both to the eye and to the eye care practitioner in terms of infection and infection routes. The subsequent confirmation of SARS-CoV-2 viral material being isolated in the tears further added to concerns about ocular risk and infection via ocular routes.
Since then, further findings have, to some extent, alleviated some of these worries. At the time of writing, it is safe to suggest the following:
- The presence of viral particles in tears makes it likely that Covid-19 might be caught through transmission in tear droplets. Statistics at present, however, suggest that the risk is likely to be low. That said, this has to be qualified with the familiar ‘additional studies are needed at this time.’ In the meantime, precautions should remain (figure 2).
- There is no increased risk of transmission of virus among contact lens wearers and their practitioners (see Optician 17.04.20 and 05.03.021).
 Figure 2: Transmission of SARS-CoV-2 via the ocular route is likely to be low risk, but further research is needed and caution prevails
Figure 2: Transmission of SARS-CoV-2 via the ocular route is likely to be low risk, but further research is needed and caution prevails
Eye Disease
It is difficult to isolate eye disease being caused as as a direct result of infection, a secondary impact due to increased risk of opportunist infections in a compromised patient, or as a result of the cardiovascular and inflammatory events triggered by severe disease. A useful overview was published by Hu et al earlier in the year.1
To explain this last point better, think about how cytomegalovirus infection of the retina is found in Aids patients, but HIV does not cause the retinitis itself. Similarly, microbial keratitis often triggers anterior uveitis, or cardiovascular perfusion compromise can cause stroke or retinopathy; but just because Covid-19 increases the risk of infections and can cause thrombosis, it would be simplistic to say that anterior uveitis, homonymous hemianopia or retinal haemorrhages (figure 3) are caused by Covid-19 infection directly. It is more important, as with diabetes, to think about the overall health of the patient and the severity and the duration of the Covid-19 disease and then understand the increased risk of associated eye diseases.

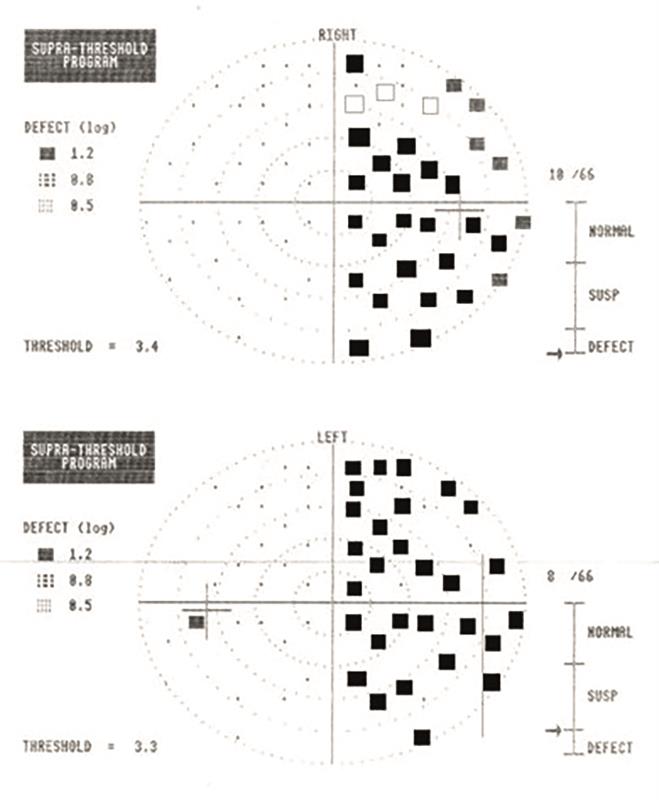
 Figure 3: Conditions associated with Covid-19. (top) anterior uveitis, (middle) homonymous hemianopia subsequent to stroke, (bottom) retinal haemorrhaging
Figure 3: Conditions associated with Covid-19. (top) anterior uveitis, (middle) homonymous hemianopia subsequent to stroke, (bottom) retinal haemorrhaging
Some key facts that have been learned:
• Coronaviruses can cause severe ocular disease in animals, including anterior uveitis, retinitis, vasculitis and optic neuritis in feline and rodent species. However, ocular manifestations in humans are typically mild and rare.2
• A 2021 meta-analysis by Nasiri et al3 reported the prevalence of all ocular manifestations among 7,300 Covid-19 patients as 11.03%, with the most frequent ocular disease being conjunctivitis (88.8%). In the same meta-analysis, dry eye or foreign body sensation (16%), eye redness (13.3%), tearing (12.8%), and itching (12.6%) were among the most frequent symptoms reported
- Other reported ocular diseases in Covid-19 patients include:
- Episcleritis; very rare
- Anterior uveitis; in patients with multi-system inflammatory disease
- Retinopathy; reports include the finding of cotton-wool spots, retinal haemorrhages, dilated veins and vascular tortuosity. One interesting paper noted a good correlation between severity of Covid-19 disease and increased retinal vein diameter4
- Neurological disorders; both optic neuritis and papilloedema have been reported, though both are rare and the mechanism uncertain
- Diplopia due to nerve palsies has been reported. This is rare but may appear within a few days of the onset of symptoms
The incidence of stroke in Covid-19 patients has been found to be 7.6 times higher than that of patients with influenza and seems to occur in a far younger than average patient population without classic vascular risk factors.5 Obviously, homonymous field loss is a consequence of stroke.
Long Covid
I suggest that we will learn a lot more about the ocular consequences of long Covid. Many likely effects are intuitive; for example, we might expect the disease to cause dissociation of phorias or loss of accommodation control in the same way as, for example, hypothyroidism. As yet, this remains conjecture.
If a patient remains in respiratory distress long enough, as is likely among those having remained in intensive care, poor perfusion and oxygen deprivation are likely to have an impact on the health of the optic nerve or retina. Remember, however, that in this situation any eye damage would be caused by hypoxia rather than by the virus itself.
Corneal nerve damage has been associated with long Covid. It seems that a loss of short corneal nerve and an increase in dendritic cell numbers is likely.6 This may be of relevance to future contact lens practice.
References
- Hu K et al. Ophthalmic Manifestations Of Coronavirus (Covid-19). [Updated 2021 May 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556093/
- Seah I, Agrawal R. Can the coronavirus disease 2019 (Covid-19) affect the eyes? A review of coronaviruses and ocular implications in humans and animals. Ocular Immunology and Inflammation, 2020, Apr 02;28(3):391-395
- Nasiri N et al. Ocular manifestations of Covid-19: A systematic review and meta-analysis. Journal of Ophthalmic Vision Research, 2021 Jan-Mar;16(1):103-112
- Invernizzi A et al. Retinal findings in patients with Covid-19: Results from the SERPICO-19 study. EClinicalMedicine. 2020, Oct;27:100550
- Merkler AE et al. Risk of ischemic stroke in patients with coronavirus disease 2019 (Covid-19) vs patients with influenza. JAMA Neurology, 2020 Jul 02
- Bitirgen G et al. Corneal confocal microscopy identifies corneal nerve fibre loss and increased dendritic cells in patients with long Covid. British Journal of Ophthalmology, 2021 Jul 26, 319450
