 Bausch+Lomb held two roadshows recently to teach practitioners how to fit their new acquisition, the Maxim CV lens. The first workshop was in Bradford and the second at City University, the one I attended. The Maxim CV lens, a semi-scleral in size, is from a US-based company called ACCU Lens and their CEO and president, William Masler OD, arrived to lecture and run a workshop ably helped by B+L sponsored personnel.
Bausch+Lomb held two roadshows recently to teach practitioners how to fit their new acquisition, the Maxim CV lens. The first workshop was in Bradford and the second at City University, the one I attended. The Maxim CV lens, a semi-scleral in size, is from a US-based company called ACCU Lens and their CEO and president, William Masler OD, arrived to lecture and run a workshop ably helped by B+L sponsored personnel.
Maxim CV
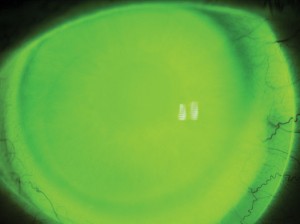
The lens is a custom scleral with a multi-curve/aspheric posterior surface produced in plasma-treated Boston XO2 material (Dk 141). The design is targeted at distorted corneas, in particular those caused by keratoconus. Due to lack of movement and the resting of the lens upon the conjunctiva, the main benefit to a patient is comfort.
Register now to continue reading
Thank you for visiting Optician Online. Register now to access up to 10 news and opinion articles a month.
Register
Already have an account? Sign in here
