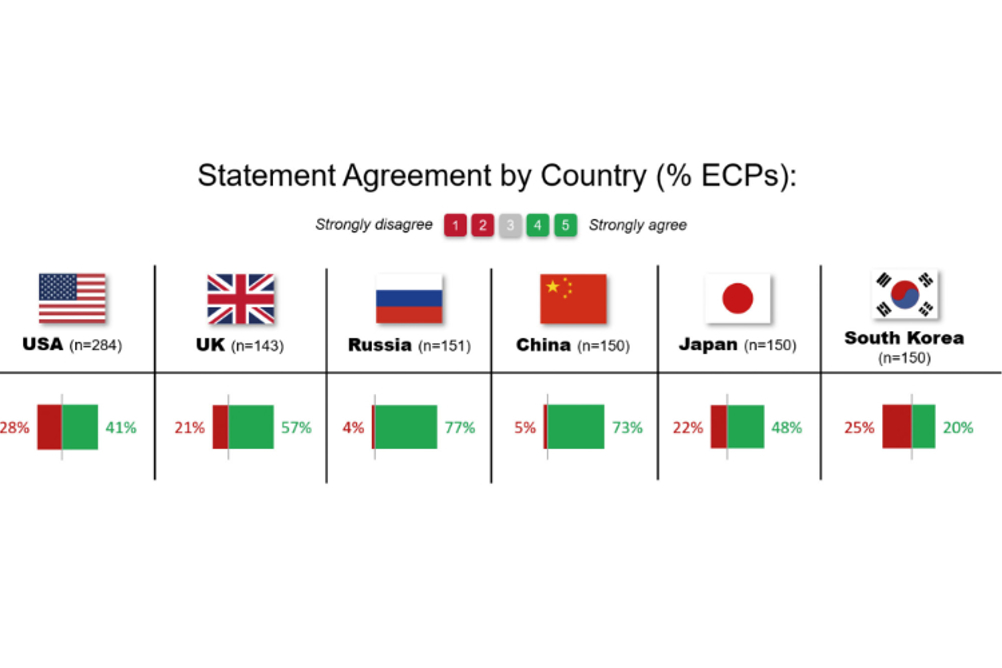
Figure 1: Results showing extent of agreement or disagreement with the statement ‘Any level of myopia is a risk factor for ocular disease.’ Data is from 2022 for all markets except Russia, which is from 2021
Myopia is increasing in prevalence globally and is estimated to affect 4.8 billion people by 2050,1 representing approximately half of the world’s population. The prevalence of high myopia is estimated to reach one billion by 2050.1
Every diopter increase in myopia has been shown to be associated with an increased risk of potentially sight threatening ocular diseases such as myopic macular degeneration, glaucoma, retinal detachments and cataract.2
In 2020, 30% of permanent vision loss was already attributable to myopia alone.3 The acceleration in myopia prevalence during the Covid-19 lockdowns4 highlights the urgency of addressing this public health issue.
Global eye care professionals (ECPs) surveys in myopia management conducted in 20155 and 20196 report there is a high level of ECP concern about myopia and its management. Despite this, the majority of ECPs (64%) are still prescribing single vision spectacles or contact lenses for myopia.6
Understanding whether practitioners are aware that even low levels of myopia increase the risk of ocular disease may be the initial step in addressing the reasons why myopia management is not being offered. This was the basis of a new global survey conducted by Johnson & Johnson Vision in 2022 in all markets expect Russia, which was conducted in 2021.7
Professional Belief Survey Results
Johnson & Johnson Vision conducted a global survey examining the professional beliefs of over 1,000 independent and retail ECPs across the US, UK, Russia, China, Japan and South Korea. On average, 47% of practitioners across all markets agreed with the statement that any level of myopia was a risk factor for ocular disease, while 21% disagreed.7
Variation was seen when stratified by country, with only 20% and 41% of ECPs in South Korea and the US agreeing, while this increased to 48%, 57%, 73% and 77% in Japan, the UK, China and Russia respectively (figure 1 - see top of article).7 This suggests there is an increasing awareness that every diopter increases the risk of myopia related ocular disease and permanent vision loss, but there is still more education and practice support required to make myopia management a world-wide practice.
What the Evidence Shows
Today, myopia is considered one of the largest global eye health threats of the 21st century.8-10 The World Health Organization (WHO) published a report recognising that myopia is not simply a refractive condition but a public health issue.11
The report provided definitions of different levels of myopia, the evidence for myopia management and recommendations for clinicians, researchers and population health surveys.
The International Myopia Institute (IMI) published a series of white papers authored by over 150 experts in the field and has also recommended definitions12 to help standardise and support evidence-based management of myopia, along with clinical management guidelines13 and clinical trial guidelines.14
Recommended definitions for myopia, high myopia, pre-myopia and pathologic myopia
The WHO recommended definition for myopia is ‘a condition in which the spherical equivalent objective refractive error is ≤ –0.50 D in either eye’.11 The definition of high myopia is ‘a condition in which the spherical equivalent objective refractive error is ≤ –5.00 D in either eye’.11
The relatively new definition of pre-myopia was proposed by the IMI as ‘a refractive state of an eye of ≤ +0.75 D at age of six years and > +0.50 D in children where a combination of baseline refraction, age and other quantifiable risk factors provide a sufficient likelihood of the future development of myopia to merit preventative interventions.’12
This is very useful since detecting myopia early is most impactful from a public health perspective, with trials now under way examining interventions during this stage.
Pathologic myopia has been defined as ‘excessive axial elongation associated with myopia that leads to structural changes in the posterior segment of the eye (including posterior staphyloma, myopic maculopathy, and high myopia-associated optic neuropathy) and that can lead to loss of best corrected visual acuity.’12 Note that there is no minimum level of myopia for pathologic myopia.
Any level of myopia is associated with increased risks of ocular disease and vision loss
The prevalence of pathologic myopia is 1 to 19% in those with low myopia and up to 70% in high myopia.13-16 Myopic macular degeneration is potentially one of the most serious consequences of myopia for which there is currently no cure.2 Every diopter increase in myopia is associated with an increased risk of myopic macular degeneration of 67%.2
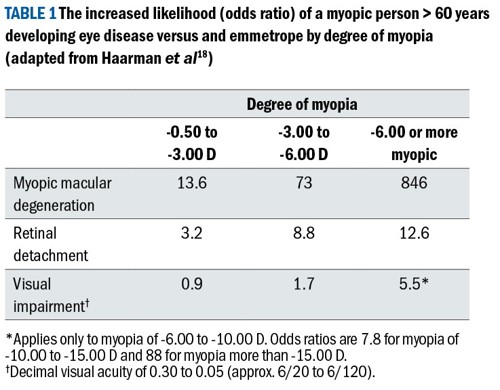
The risks of other conditions such as glaucoma, retinal detachment and cataract also increase by 20 to 30% with every diopter increase in myopia (table 1). Reducing myopia by 1D in an individual may reduce their risk of developing myopic macular degeneration by 40%.2 The latest evidence suggests that there is no safe level of myopia.8,17
Axial length measurement was once only in the realm of clinical trials, but is now being utilised more frequently in the clinic to monitor myopia progression given its direct relationship with eye growth, and the strong association with disease and vision impairment in excessive axial elongation.15
The ability to measure refractive error accurately means the lack of an optical biometer should not be a barrier to provide myopia management.
Myopia levels and quality of life
Myopia management may result in huge personal benefits for our patients. Even correcting myopia at the lower levels improves quality of life due to less visual disability.2,19
Correction with contact lenses in children and teens may improve self-confidence, participation in activities,20 and increase time spent outdoors,21 which all have benefits for overall physical and mental health. There may also be better outcomes for surgical myopia correction in later life by keeping myopia levels low.2
Conclusion
The evidence suggests that the potential benefits of myopia management far outweigh the risks.19 Every diopter of myopia matters – each diopter increases the risk of developing potentially sight-threatening complications later in life.2 The IMI states that evidence-based treatments have been demonstrated to slow myopia clinically.17
Offering myopia management to slow myopia as soon as a child develops it, along with careful and objective monitoring is advocated by the World Council of Optometry and other key professional associations.21,22
ECPs are well placed to educate and advocate for myopia management and should be part of a multidisciplinary approach that includes schools, general practitioners, pediatricians, government and industry. Clinicians are a key part of the solution in helping to reduce the huge global socioeconomic burden of myopia.23-25
- Dr Aman Mahil is a clinical scientist and education team lead at the Centre for Ocular Research & Education, School of Optometry & Vision Science, University of Waterloo.
- Dr Monica Jong is director of global professional education for myopia for Johnson & Johnson Vision Care, Inc.
References
- Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, Wong TY, Naduvilath TJ, Resnikoff S: Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 2016; 123:1036-42.
- Bullimore MA, Brennan NA: Myopia control: why each diopter matters. Optometry and Vision Science. 2019; 96:463-5.
- Jong M, Brennan NA, Bullimore MA: The Role of Myopia in 2020 Uncorrected Global Visual Impairment. Investigative Ophthalmology & Visual Science. 2022; 63:243–A0097-243–A.
- Ma M, Xiong S, Zhao S, Zheng Z, Sun T, Li C: COVID-19 home quarantine accelerated the progression of myopia in children aged 7 to 12 years in China. Investigative ophthalmology & visual science. 2021; 62:37.
- Wolffsohn JS, Calossi A, Cho P, Gifford K, Jones L, Li M, Lipener C, Logan NS, Malet F, Matos S: Global trends in myopia management attitudes and strategies in clinical practice. Contact Lens and Anterior Eye. 2016; 39:106-16.
- Wolffsohn JS, Calossi A, Cho P, Gifford K, Jones L, Jones D, Guthrie S, Li M, Lipener C, Logan NS: Global trends in myopia management attitudes and strategies in clinical practice – 2019 Update. Contact Lens and Anterior Eye. 2020; 43:9-17.
- Johnson & Johnson Vision Care. Online survey of 1028 Eye Care Professionals across United States, United Kingdom, Russia, China, Japan, and South Korea. JJV data on file.; 2021 (Russia) and 2022 (other markets).
- Flitcroft D: The complex interactions of retinal, optical and environmental factors in myopia aetiology. Progress in retinal and eye research. 2012; 31:622-60.
- Resnikoff S, Jonas JB, Friedman D, He M, Jong M, Nichols JJ, Ohno-Matsui K, Smith III EL, Wildsoet CF, Taylor HR: Myopia–a 21st century public health issue. Investigative Ophthalmology & Visual Science February 2019, Vol.60, Mi-Mii.
For full references see online at opticianonline.net. - Brennan NA, Toubouti YM, Cheng X, Bullimore MA: Efficacy in myopia control. Progress in retinal and eye research. 2021; 83:100923.
- WHO: The impact of myopia and high myopia. Joint World Health Organization – Brien Holden Vision Institute Global Scientific Meeting on Myopia. Edited by WHO. Sydney, Australia, 2015.
- Flitcroft DI, He M, Jonas JB, Jong M, Naidoo K, Ohno-Matsui K, Rahi J, Resnikoff S, Vitale S, Yannuzzi L: IMI–Defining and classifying myopia: a proposed set of standards for clinical and epidemiologic studies. Investigative ophthalmology & visual science. 2019; 60:M20-M30.
- Gifford KL, Richdale K, Kang P, Aller TA, Lam CS, Liu YM, Michaud L, Mulder J, Orr JB, Rose KA: IMI–clinical management guidelines report. Investigative ophthalmology & visual science. 2019; 60:M184-M203.
- Wolffsohn JS, Kollbaum PS, Berntsen DA, Atchison DA, Benavente A, Bradley A, Buckhurst H, Collins M, Fujikado T, Hiraoka T: IMI – Clinical myopia control trials and instrumentation report. Investigative ophthalmology & visual science. 2019; 60:M132-M60.
- Tideman JWL, Snabel MC, Tedja MS, Van Rijn GA, Wong KT, Kuijpers RW, Vingerling JR, Hofman A, Buitendijk GH, Keunen JE: Association of axial length with risk of uncorrectable visual impairment for Europeans with myopia. JAMA ophthalmology. 2016; 134:1355-63.
- Ohno-Matsui K, Wu P-C, Yamashiro K, Vutipongsatorn K, Fang Y, Cheung CMG, Lai TY, Ikuno Y, Cohen SY, Gaudric A: IMI pathologic myopia. Investigative ophthalmology & visual science. 2021; 62:5.
- Németh J, Tapasztó B, Aclimandos WA, Kestelyn P, Jonas JB, De Faber J-TH, Januleviciene I, Grzybowski A, Nagy ZZ, Pärssinen O: Update and guidance on management of myopia. European Society of Ophthalmology in cooperation with International Myopia Institute. European Journal of Ophthalmology. 2021; 31:853-83.
- Haarman AE, Enthoven CA, Tideman JWL, Tedja MS, Verhoeven VJ, Klaver CC: The complications of myopia: a review and meta-analysis. Investigative ophthalmology & visual science. 2020; 61:49.
- Bullimore MA, Ritchey ER, Shah S, Leveziel N, Bourne RR, Flitcroft DI: The risks and benefits of myopia control. Ophthalmology. 2021; 128:1561-79.
- Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutiérrez-Ortega R: Myopia control with orthokeratology contact lenses in Spain: a comparison of vision-related quality-of-life measures between orthokeratology contact lenses and single-vision spectacles. Eye & contact lens. 2013; 39:153-7.
- Zhao F, Zhao G, Zhao Z: Investigation of the effect of orthokeratology lenses on quality of life and behaviors of children. Eye & contact lens. 2018; 44:335-8.
- https://worldcouncilofoptometry.info/resolution-the-standard-of-care-for-myopia-management-by-optometrists/. World Council of Optometry Resolution: The Standard of Care For Myopia Management by Optometrists.
- Jonas JB, Ang M, Cho P, Guggenheim JA, He MG, Jong M, Logan NS, Liu M, Morgan I, Ohno-Matsui K: IMI prevention of myopia and its progression. Investigative ophthalmology & visual science. 2021; 62:6.
- Fricke TR, Jong M, Naidoo KS, Sankaridurg P, Naduvilath TJ, Ho SM, Wong TY, Resnikoff S: Global prevalence of visual impairment associated with myopic macular degeneration and temporal trends from 2000 through 2050: systematic review, meta-analysis and modelling. British Journal of Ophthalmology. 2018; 102:855-62.
- Naidoo KS, Fricke TR, Frick KD, Jong M, Naduvilath TJ, Resnikoff S, Sankaridurg P: Potential lost productivity resulting from the global burden of myopia: systematic review, meta-analysis, and modeling. Ophthalmology. 2019; 126:338-46.
