
In the Optometry Building. [Credit: Aston University]
The Optometry and Vision Science Research Group at Aston University includes within its main research focus visual development and myopia, the crystalline lens and ocular surface, vision and perception and vascular imaging.
The Group also has specialist expertise in the area of ophthalmic technology and associated devices. The Group interfaces with the College of Health and Life Sciences, where the School of Optometry provides undergraduate, postgraduate and Continuing Professional Development study modules linked to optometry.
The Group also has close links with the Aston Research Centre for Health in Ageing, the Aston Institute of Health and Neurodevelopment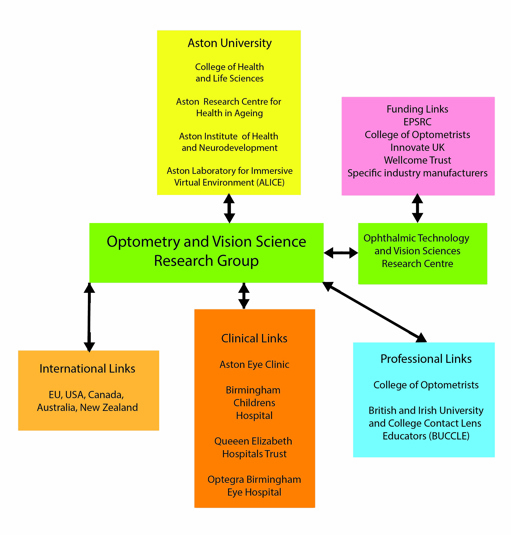 and the Aston Laboratory for Immersive Virtual Environments (ALIVE) research facility, which combines motion capture, virtual reality and electroencephalogram recording equipment.
and the Aston Laboratory for Immersive Virtual Environments (ALIVE) research facility, which combines motion capture, virtual reality and electroencephalogram recording equipment.
The key themes of research undertaken by ALIVE include high-level cognition, social cognition and social neuroscience, social vision and social virtual humans.
Key individuals within the vision research focus at Aston University include Professor James Wolffsohn and Professor Nicola Logan. Prof Wolffsohn is currently Pro-Vice Chancellor for Research Integrity. Prof Logan is currently Professor in Optometry and Physiological Optics and also director of the Optometry and Vision Science Research Group. Professor Shehzad Naroo has a key role of editor-in-chief of the publication Contact Lens and Anterior Eye.
The Ophthalmic Technology and Devices Research Centre
This centre draws upon a diverse group of specialist skills including biological science, photonics, medical pathophysiology, drug delivery, biomedical engineering, material science, imaging, sensor technology, informatics and software engineering to develop and make available innovative ophthalmic technologies and represents a partnership between academia, industry and the NHS.
While there has always been recognition of the adverse general health factors of deteriorating vision with age,1 the modern information era with its copious use of smartphones and tablets has further emphasised the need for good vision.
Funding for the Research Centre is derived from a range of sources such as the EPSRC, the College of Optometrists, Innovate UK, the Wellcome Trust, various manufacturers and the pharmaceutical industry.
A spin-off company from this Research Centre is Eyeoto, where a key development tele-optometry product called Theia (figure 3) is a remote digital slit lamp, which allows an emergency care practitioner to conduct a comprehensive anatomical health check of the eye while removing the need to have the clinician and the patient in the same location.
Figure 3: The Theia remote slit lamp system developed by Eyeoto. Photo credit: Eyeoto
 The technology allows professional eye examinations to be undertaken for patients in remote locations, meaning clinicians can provide eye care in practices where cover can be hard to source.
The technology allows professional eye examinations to be undertaken for patients in remote locations, meaning clinicians can provide eye care in practices where cover can be hard to source.
Aston Vision Sciences, working in association with Aston University, is developing the POVScope system to provide the functionality of several standard eye examination systems in a single portable non-patient contact device to enable fast diagnosis and triage.
The expectation is that the high standard of diagnostic information captured in specialist clinics can now be achieved with such novel technology.
As part of the green credentials of Aston Vision Sciences, use is made of the Escosia search engine where searches made count towards tree planting via advertisement revenue. Wolffson Research is another spin-off company that specialises in ophthalmic apps and software tools for clinicians.
Knowledge Transfer Partnership
A knowledge transfer partnership is in the process of being established between the Belfast-based Cathedral Eye Clinic, which is a eye healthcare facility, and a team of academics from Aston University to optimise principally the treatment of dry eye conditions using artificial intelligence (AI) methodology.
The main contribution of the team at Aston University will be to provide a combination of state-of-the-art ocular surface clinical assessment tools and AI skills to assist the Belfast clinic in developing diagnostic tools to optimise the treatment of dry eye – allowing effective treatments to be identified without recourse to specialist highly trained staff.
Research Focus
Key equipment items used within the Optometry and Vision Science Research Centre to diagnose and quantify the extent of dry eye syndrome in patients include systems such as the Oculus Keratograph 5M (figure 4) and the Medmont Meridia devices.
In addition to overall mapping of corneal topography, such systems can also quantify stability of tear film of the cornea as a measure of severity of dry eye condition. A novel feature of such systems is the facility of meibomian gland imaging where the exposed surface of the upper and lower eyelids can be viewed in infrared light.
Figure 4: Image of fluorescein staining of cornea using Oculus Keratograph system. Photo credit: Aston University

For the Oculus Keratograph 5M system this is generated by an infrared LED centred at 840nm. It is noted by Swiderska et al, however, that the greatest contrast for such images is produced by light centred at 750nm.2
A paper by Wang et al, with involvement of vision researchers at Aston University, describes the association of digital screen use with the development of dry eye disease.3 A subject sample of 446 participants was obtained from attendees at a Royal Society Summer Science Exhibition in 2008.
Tear film stability was determined using an Oculus Keratograph 5M system and a specific Dry Eye Questionnaire (DEQ-5)4 was used to provide a diagnostic score. In addition, a lifestyle factor questionnaire was administered.
The study indicated that for each hour of increased digital screen exposure there was a 15% increase in likelihood of dry eye disease. It is considered that this effect is prompted by suppression of normal blink pattern by cognitive loading associated with screen use.
The authors also indicate that ‘upgazing’ with a computer monitor use is likely to increase the exposed area of the cornea and contribute towards increased tear film evaporation.
Researchers within the College of Health and Life Sciences at Aston University investigated details of transient effects of smoking on the eye with a focus on dry eye parameters.5 Tear-break-up-time and mean lipid layer thickness were measured using the Oculus Keratograph 5M and the EasyTearView/Tearscope.
In addition, tear-break-up-time was determined with fluorescein viewing the corneal surface through a slit lamp and with results summarised in table 1.
Table 1: Values of tear-break-up-time (TBUT) and lipid layer thickness before and after smoking for identified measurement techniques5

Such findings indicate an immediate adverse transient effect on tear film stability and mean lipid layer thickness. It is relevant to note, however, the differences in values of tear film stability using the various measurement techniques.
An international multi-centre survey6 of patient reported experience of self management of dry eye, with involvement of Aston University, identified common trends between subjects in Canada, Mexico, New Zealand, Taiwan and the United Kingdom.
Where identified, the condition of dry eye largely affected both eyes equally and was more common in females (65%). In addition, less than 50% of subjects had consulted an appropriate health professional and the self treatment of choice was artificial tear eye drops, though it was identified that factors generally led to non-optimised treatment therapies.
A systematic review of the use and effectiveness of artificial tears by Semp et al at Aston University provides useful guidance on this facet of management of dry eye disease.7 A general consensus indicates that artificial tears will only work with around two-thirds of patients and where their effectiveness can be gauged after a month of directed treatment, usually of four applications per day.
There is an indication also that non-preserved or soft-preserved preparations should be used. The review also highlighted comparisons between different chemical formulations.
As indicated in the paper by Semp et al, numerous comparative studies of the relative merits of ‘artificial tears’ products exist.7
One such study,8 with involvement of Aston University, compared the relative efficacy of one product with a low concentration of Phospholipid (Ocuvers Spray hyaluron) and another with a high concentration (Tears Again Sensitive).
Use of the higher concentration product was found to significantly improve the non-invasive tear breakup time and also the ocular comfort score.
Contact Lens Evidence Based Academic Reports
The publication of the Contact Lens Evidence-based Academic Reports (CLEAR), as a focus of the British Contact Lens Association (BCLA), have been published as a series of papers in Contact Lens and Anterior Eye.9-18 Key papers in his sequence have direct involvement with the staff members within Aston University.
The CLEAR report on Anatomy and Physiology of the Anterior Eye9 provides a highly detailed profile of cellular structures and while the cornea is described in the expected high level of detail, so also are structures such as the conjunctiva, eyelids, lacrimal system and tear film.
In some ways, the high level of complexity of functioning of all of these systems together in a connected clinical system underscores the challenges of contact lens prescribing and the management of dry eye disease. From an evolutionary perspective, the eye had been a system that has, out of necessity, developed a highly complex system of cellular function to maintain a stable and effective vision system.
The BCLA CLEAR publication Evidence-based contact lens practice,18 with key input from Aston University, provides an in depth review of the methodology of determining good practice and also a detailed description of a framework for safe and considerate prescribing, fitting and aftercare of contact lenses.
Tear Film & Ocular Surface Society (TFOS) Reports
Aston University has also participated in research promoted by the Tear Film & Ocular Surface Society (TFOS) based in Boston, USA. A significant international multi-centre review Lifestyle Challenges And Dry Eye Disease19 as part of this TFOS Lifestyle series and, with involvement of Aston University, includes over 500 references though the study extends beyond lifestyle challenges into a broad range of underlying medical/clinical issues.
While studies have identified a link between depression, anxiety and stress and dry eye disease, both the mechanisms of causation and routes of appropriate therapy remain unclear. There is a strong association between sleep disorders and dry eye disease but there remains a lack of clarity between the causation arising from physical lack of sleep and underlying psychosocial disorders.
In terms of obesity, there is some evidence for association with meibomian gland dysfunction and eyelid architecture. Several studies reference wearing of face masks as a factor associated in particular with evaporative dry eye disease and meibomian gland dysfunction.20
There is also solid evidence to support comorbidity between chronic pain conditions and dry eye disease though the study identifies the need to identify causation separately of evaporative and aqueous deficient subtypes.
The TFOS Lifestyle paper on Impact of nutrition on the ocular surface21 is a major resource reference in this field with almost 700 references and with input from the School of Optometry at Aston University.
A summary of findings is outlined in table 2.
Table 2: Summary of possible positive and negative impacts on the ocular surface due to nutrition.21 (DE = dry eye; INF = inflammation; OSI = ocular surface innervation, OM = ocular microbiome)

By far, the greater number of studies relate to the potential beneficial use of omega-3, though in this context, it is thought omega-6 has a potential negative effect on dry eye conditions. In terms of the involvement of alcohol, one study indicated a possible negative effect on females but a potential protective effect on males.22
However, with the dietary intake of individuals becoming more and more complex in western society, research is unlikely to be able to fully track the effect of this on the ocular surface. The existing available information has potential application in the development of AI tools. Many of the observed relationships, however, are identified without a basic understanding of the metabolic pathways involved.
The TFOS publication Impact of the digital environment on the ocular surface23 resourced with over 600 references and with input from the University of Aston, provides a useful resource for consideration of the effect of increasing interaction with screen-based technologies of various types.
Accommodating Intraocular Lenses
Wei et al describe evaluation of a synthetic material membrane derived from silicon rubber as a potential material for evaluating the function of prototype accommodating intraocular lenses where a degree of accommodation is retained via the compliant material of the implanted lens.24 The authors describe how the technique of finite element analysis provided a mechanism of validating test techniques.
Transcranial Magnetic Stimulation
Transcranial Magnetic Stimulation25 is a developed technology that generates an electric field vector used to stimulate nerve circuits in the brain and can be used to diagnose, for example, active and non-active neural pathways. Researchers at Aston University have experience of using Transcranial Magnetic Stimulation in association with functional magnetic resonance imaging (fMRI)26, 27 to map aspects of neural functionality within the visual cortex.
Summary
It is only possible to provide a brief summary of the research activity of vision science within Aston University. Significant strengths of such activity, however, include the wide range of research areas and the diverse and extensive links with academia, healthcare providers and industry within the UK and abroad.
References
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on Public Health Approaches to Reduce Vision Impairment and Promote Eye Health. Making Eye Health a Population Health Imperative: Vision for Tomorrow. Welp A, Woodbury RB, McCoy MA, Teutsch SM, editors. Washington (DC): National Academies Press (US); 2016 Sep 15. PMID: 27656731.
- Swiderska K, Blackie CA, Maldonado-Codina C, Fergie M, Morgan PB, Read ML. Development of Artefact-Free Imaging System for Accurate Meibomian Gland Reflectivity Assessment. Transl Vis Sci Technol. 2023 Feb 1;12(2):9.
- Wang MTM, Craig JP, Vidal-Rohr M, Menduni F, Dhallu S, Ipek T et al. Impact of digital screen use and lifestyle factors on dry eye disease in the paediatric population. Ocul Surf. 2022 Apr;24:64-66
- Chalmers RL, Begley CG, Caffery B. Validation of the 5-Item Dry Eye Questionnaire (DEQ-5): Discrimination across self-assessed severity and aqueous tear deficient dry eye diagnoses. Cont Lens Anterior Eye. 2010 Apr;33(2):55-60
- Latif N, Naroo SA. Transient effects of smoking on the eye. Cont Lens Anterior Eye. 2022 Oct;45(5):101595.
- Bilkhu P, Sivardeen Z, Chen C, Craig JP, Mann K, Wang MTM et al. Patient-reported experience of dry eye management: An international multicentre survey. Cont Lens Anterior Eye. 2022 Feb;45(1):101450.
- Semp DA, Beeson D, Sheppard AL, Dutta D, Wolffsohn JS. Artificial Tears: A Systematic Review. Clin Optom (Auckl). 2023 Jan 10;15:9-27
- Pult H, Khatum FS, Trave-Huarte S, Wolffsohn JS. Effect of Eye Spray Phospholipid Concentration on the Tear Film and Ocular Comfort. Eye Contact Lens. 2021 Aug 1;47(8):445-448
- Downie LE, Bandlitz S, Bergmanson JPG, Craig JP, Dutta D, Maldonado-Codina C et al. CLEAR - Anatomy and physiology of the anterior eye. Cont Lens Anterior Eye. 2021 Apr;44(2):132-156
- Willcox M, Keir N, Maseedupally V, Masoudi S, McDermott A, Mobeen R et al. CLEAR - Contact lens wettability, cleaning, disinfection and interactions with tears. Cont Lens Anterior Eye. 2021 Apr;44(2):157-191
- Morgan PB, Murphy PJ, Gifford KL, Gifford P, Golebiowski B, Johnson L et al. CLEAR - Effect of contact lens materials and designs on the anatomy and physiology of the eye. Cont Lens Anterior Eye. 2021 Apr;44(2):192-219
- Vincent SJ, Cho P, Chan KY, Fadel D, Ghorbani-Mojarrad N, González-Méijome JM et al. CLEAR - Orthokeratology. Cont Lens Anterior Eye. 2021 Apr;44(2):240-269
- Barnett M, Courey C, Fadel D, Lee K, Michaud L, Montani G et al. CLEAR - Scleral lenses. Cont Lens Anterior Eye. 2021 Apr;44(2):270-288
- Stapleton F, Bakkar M, Carnt N, Chalmers R, Vijay AK, Marasini S et al. CLEAR - Contact lens complications. Cont Lens Anterior Eye. 2021 Apr;44(2):330-367
- Jacobs DS, Carrasquillo KG, Cottrell PD, Fernández-Velázquez FJ, Gil-Cazorla R, Jalbert I et al. CLEAR - Medical use of contact lenses. Cont Lens Anterior Eye. 2021 Apr;44(2):289-329
- Richdale K, Cox I, Kollbaum P, Bullimore MA, Bakaraju RC, Gifford P et al. CLEAR - Contact lens optics. Cont Lens Anterior Eye. 2021 Apr;44(2):220-239
- Jones L, Hui A, Phan CM, Read ML, Azar D, Buch J et al. CLEAR - Contact lens technologies of the future. Cont Lens Anterior Eye. 2021 Apr;44(2):398-430
- Wolffsohn JS, Dumbleton K, Huntjens B, Kandel H, Koh S, Kunnen CME et al. CLEAR - Evidence-based contact lens practice. Cont Lens Anterior Eye. 2021 Apr;44(2):368-397
- Galor A, Britten-Jones AC, Feng Y, Ferrari G, Goldblum D, Gupta PK et al. TFOS Lifestyle: Impact of lifestyle challenges on the ocular surface. Ocul Surf. 2023 Apr;28:262-303
- Azzam SH, Nama A, Badarni H, Asael H, Dahoud WA, Mimouni M et al. Assessment of dry eye disease in N95 versus surgical face mask wearers during COVID-19. Indian J Ophthalmol. 2022 Mar;70(3):995-999
- Markoulli M, Ahmad S, Arcot J, Arita R, Benitez-Del-Castillo J, Caffery B et al. TFOS Lifestyle: Impact of nutrition on the ocular surface. Ocul Surf. 2023 Apr 25;29:226-271
- Magno MS, Daniel T, Morthen MK, Snieder H, Jansonius N, Utheim TP et al. The relationship between alcohol consumption and dry eye. Ocul Surf. 2021 Jul;21:87-95
- Wolffsohn JS, Lingham G, Downie LE, Huntjens B, Inomata T, Jivraj S et al. TFOS Lifestyle: Impact of the digital environment on the ocular surface. Ocul Surf. 2023 Apr;28:213-252
- Wei H, Wolffsohn JS, Gomes de Oliveira O, Davies LN. Characterisation and Modelling of an Artificial Lens Capsule Mimicking Accommodation of Human Eyes. Polymers (Basel). 2021 Nov 12;13(22):3916.
- Silvanto J. Transcranial magnetic stimulation and vision. Handb Clin Neurol. 2013;116:655-69
- Strong, S., & Silson, E. H. (2022). Transcranial Magnetic Stimulation Mapping for Perceptual and Cognitive Functions. In D. Pustina, & D. Mirman (Eds.), Lesion-to-Symptom Mapping (pp. 271-288). (Neuromethods; Vol. 180). Humana Press.
- Strong SL, Silson EH, Gouws AD, Morland AB, McKeefry DJ. An enhanced role for right hV5/MT+ in the analysis of motion in the contra- and ipsi-lateral visual hemi-fields. Behav Brain Res. 2019 Oct 17;372:112060.
