 Bill Harvey and David Ruston describe some clinical presentations related to silicone hydrogel lens fitting and follow up, indicating both their interpretation and how best to record them (C1471).
Bill Harvey and David Ruston describe some clinical presentations related to silicone hydrogel lens fitting and follow up, indicating both their interpretation and how best to record them (C1471).
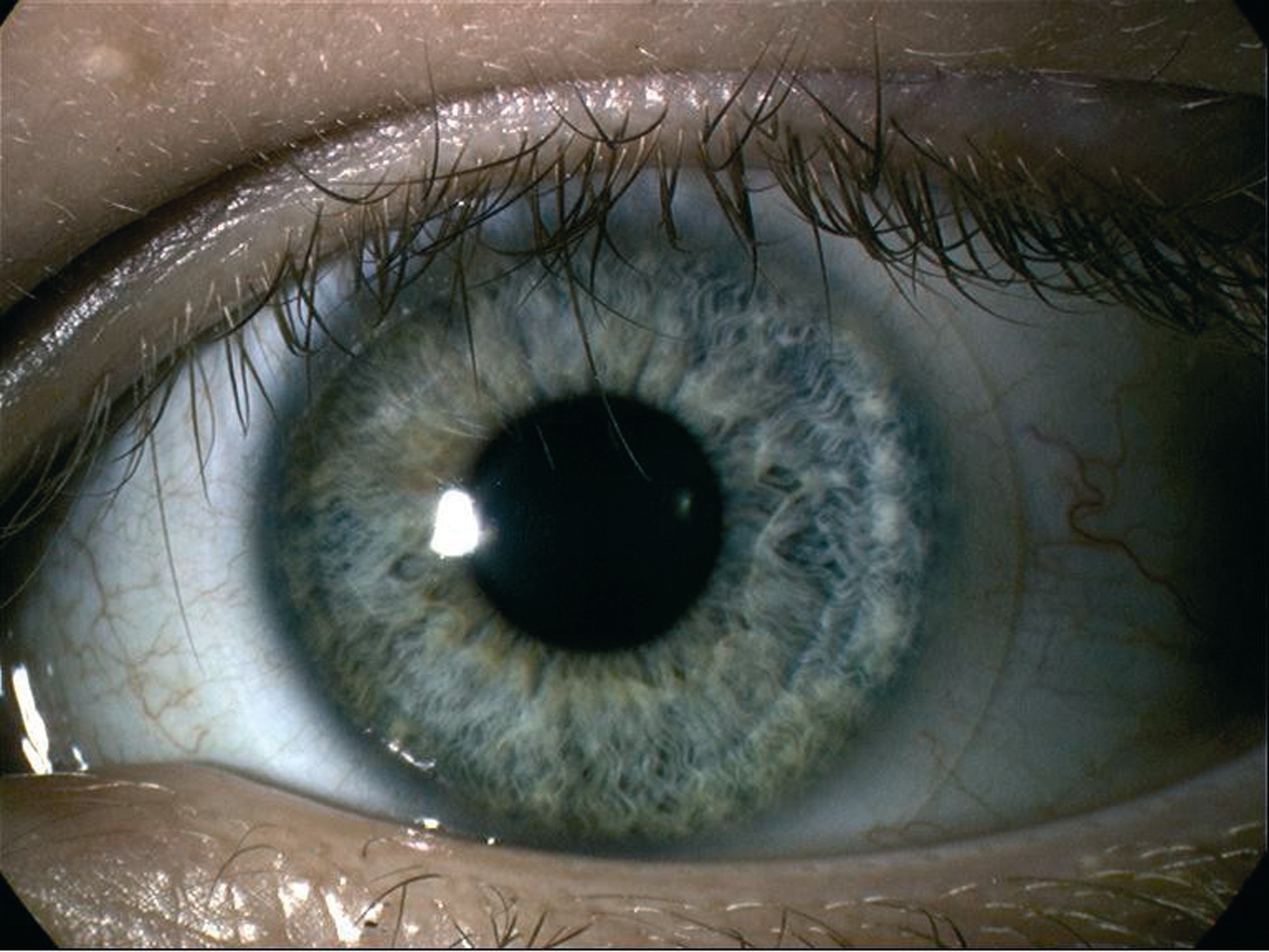
The increasing use of silicone hydrogel material contact lenses over recent years is related to a realisation of the excellent oxygen delivery properties of the lens resulting in a reduction in signs of hypoxia and serious keratitis. An immediate and impressive advantage is the apparent reduction in limbal and conjunctival hyperaemia seen with the material (Figure 1) as opposed to the more familiar hyperaemia seen with extensive wear of conventional hydrogels (Efron grade 1 trace hyperaemia in Figure 2 or grade 3 moderate hyperaemia in Figure 3).
Register now to continue reading
Thank you for visiting Optician Online. Register now to access up to 10 news and opinion articles a month.
Register
Already have an account? Sign in here
