There are several sources of error in Goldmann applanation tonometry,1 but one which is readily minimised is misplacement of the probe on the corneal surface. Whereas the requirements for correct placement are well known, the magnitude of error thus avoided is slightly obscure in the literature. In this brief article I present results from a theoretical analysis of the two main types of misplacement error.
Displacement from centre
In use, the Goldmann probe (figure 1) slightly indents and applanates (flattens) a circular patch on a spherical cornea. The size of the applanated patch varies with the force applied by the probe. When the circle of applanation has a diameter of 3.06mm, the force applied by the probe is adjudged to be a measure of the eye’s intraocular pressure (IOP).
The ingenious design of the Goldmann probe allows an assessment of whether the applanation disc is more, less or exactly 3.06mm in diameter. It incorporates a pair of prisms which each displace half the image at the probe’s tip by 1.53mm in opposite directions. The probe is aligned so it bisects the applanation circle along its diameter and is seen, by virtue of the prismatic
displacements, as two semicircles. The force on the probe is adjusted until the inner edges of the semicircles coincide. At this point, the applanation disc’s diameter is exactly 3.06mm and a reading is made of the force applied by the probe. This reading (in grammes) is converted to an IOP measurement (in mmHg) by multiplying by a factor of 10.
The appearance at optimum applanation is shown in the upper portion of figure 2.
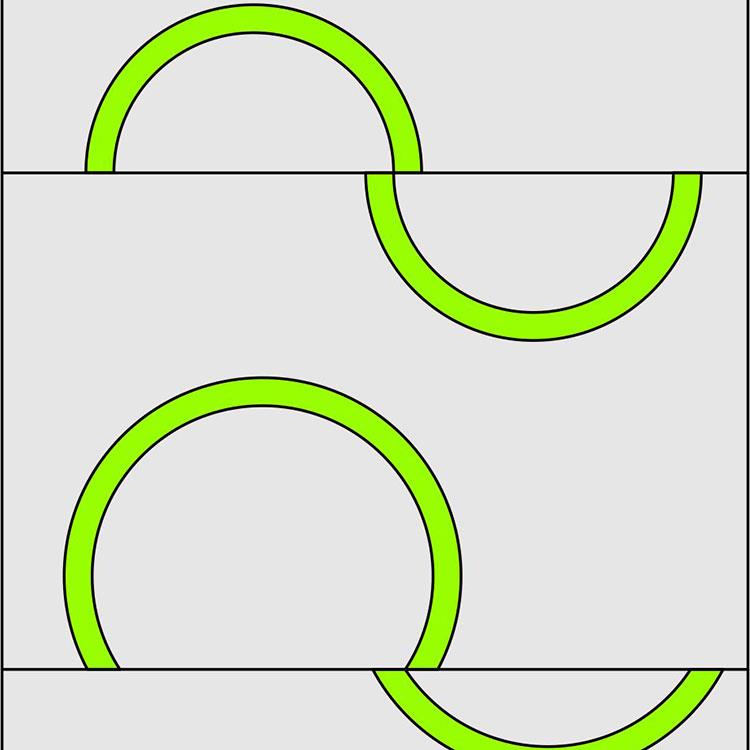
Figure 2 (a): View when correctly aligned at point of measurement. Displacement from centre to result in overestimated measurement.
However, if the probe is off-centre, it crosses the applanation circle at a chord smaller than the diameter. To align the arc inner edges in this situation requires an increase in the force applied to the probe resulting in an erroneous overestimation of IOP. Figure 2b shows the appearance of the arcs if the probe was off-centre by 1mm. It can be seen that the circle of applanation is obviously larger.

Figure 2b: Real-life view showing rings when too great a force is applied
The question is how much error is caused by incorrect centration of the Goldmann probe? The answer depends on how far the probe is displaced from the optimum position, the greater the displacement, the greater the error. This is illustrated in figure 3 which was calculated on the basis of applanation area being proportional to applanating force. A misplacement as poor as shown in figure 2a might, for example, deliver a reading of 27mmHg instead of 19mmHg on the same eye.
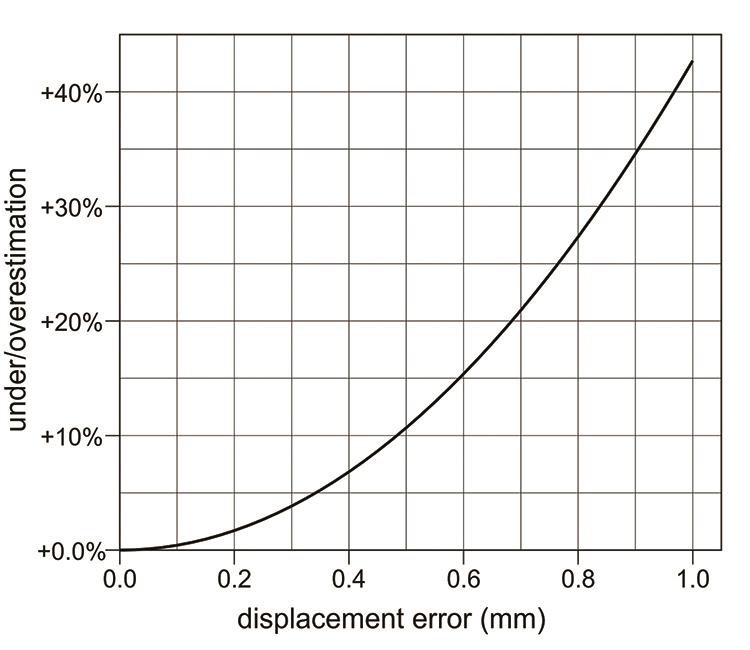
Figure 3: Error induced by displacement from centre
Corneal astigmatism
Goldmann tonometry is predicated on applanating a corneal area equal to a circle of 3.06mm diameter. However, in corneal astigmatism the applanated region is an ellipse and its diameter ranges from greater than 3.06mm along the major axis to less than 3.06mm along the minor axis. However, there is an intermediate meridian orientated between the major and minor axes along which the diameter does equal 3.06mm and the Goldmann probe should be aligned with it to ensure accurate measurement.
This is explained in Haag-Streit’s manual for the Goldmann tonometer:2
‘The choice of meridian is of significance, however, when measuring eyes with corneal astigmatism greater than three dioptres, since the flattened area is not circular but elliptical. It has been calculated that, in cases of greater corneal astigmatism, a surface of 7.354mm2 (ø 3.06mm) is applanated if the measuring prism is at an angle of 43° to the meridian of the greatest radius.’
Thus, to eliminate, or at least minimise this source of error, the angular orientation of the Goldmann probe is offset by an angle of 43° from the flattest corneal meridian before taking an IOP reading. To aid correct alignment a secondary axis line is marked on the probe holder. This is usually labelled with the letter ‘A’ or marked as a red line (figure 4). Aligning this with the axis graduation on the probe body ensures the correct offset.
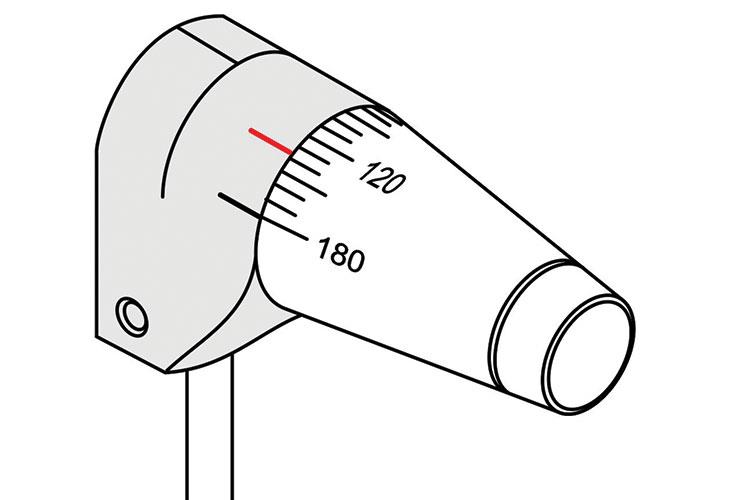
Figure 4: Mounted Goldmann probe showing 43° offset marker (red)
What magnitude of error is engendered if the 43° offset is ignored? The worst case scenarios occur if the probe is aligned along either the flattest or the steepest corneal meridians. In the former case the measurement of 3.06mm spans the longest axis of the applanation ellipse but the applanated area falls short of 7.354mm2 resulting in an underestimation of IOP. In the latter case exactly the opposite occurs.
How large the measurement error is in those situations will vary with the degree of corneal astigmatism. To calculate this I have modelled corneas based on an ‘average’ 7.80mm corneal curvature such that the same indentation (0.15153mm) applanates the same area (7.3542mm2) whatever the degree of astigmatism. The derivation of the equations used for this exercise can be found elsewhere.3
The results are shown in figure 5. It can be seen there is an almost perfect linear relationship between the degree of corneal astigmatism and the amount of under or over-correction. Although significant, the measurement error is not large being less than ±8% over the range considered.
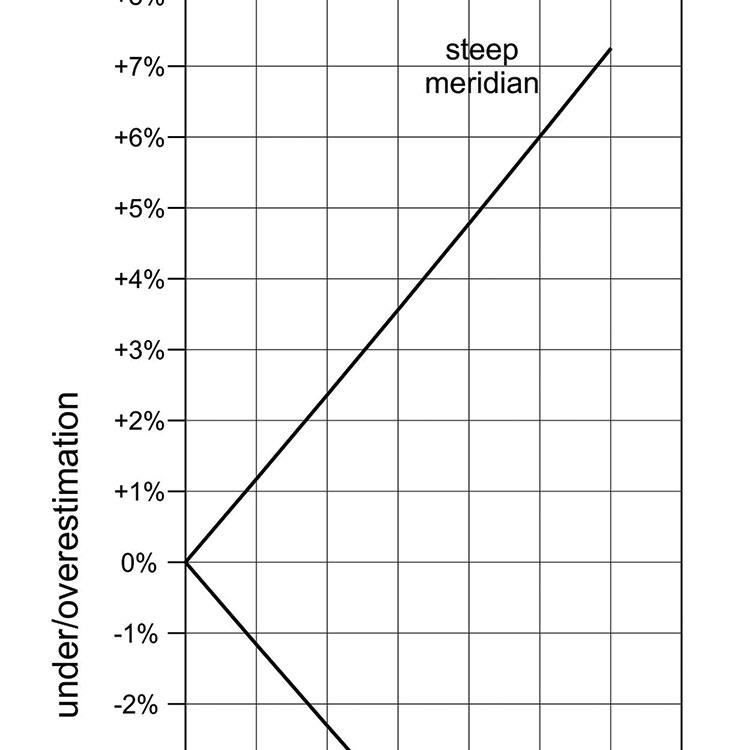
Figure 5: Error induced by measurement along principal meridians on astigmatic corneas
It should be noted the optimum offset angle is not actually a constant 43°, but varies according to the eccentricity (ie the non-circularity) of the applanation patch which, in turn, depends on the degree of corneal astigmatism. For low degrees of astigmatism the optimum angle is close to 45° gradually diminishing for larger amounts of astigmatism until around 12 dioptres when it does eventually equal 43°. Within this range the static 43° offset is responsible for an underestimation of IOP. However, the underestimation never exceeds a negligible 0.25% (Figure 6). Thus, for a very wide range of corneal astigmatism, the 43° offset satisfactorily minimises this source of measurement error.
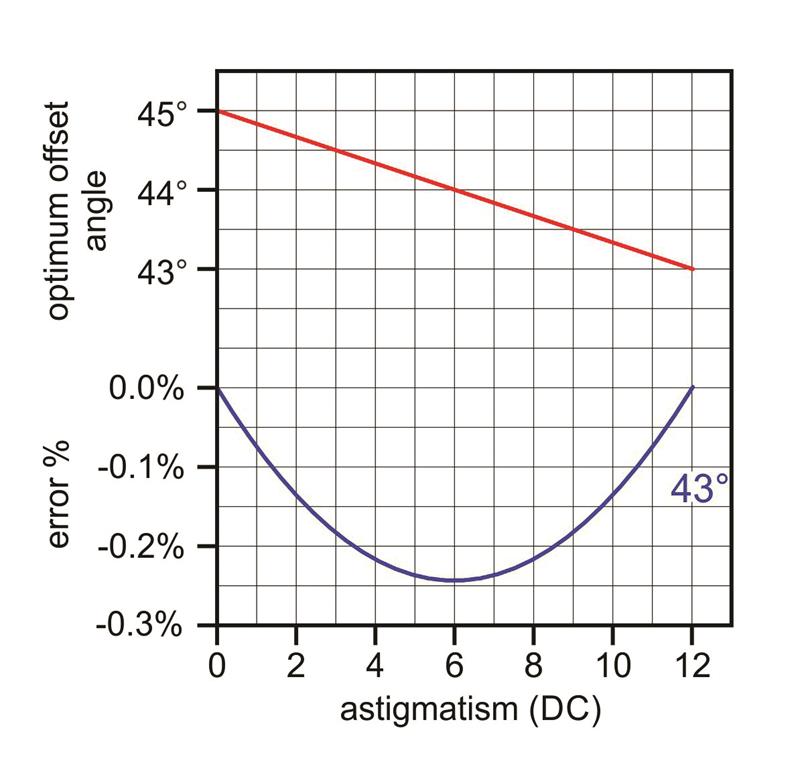
Figure 6: Red line shows the optimum offset angle for zero measurement error on astigmatic corneas. Blue line shows error values for Goldmann probe offset at 43°
How critical is this setting of 43°? A couple of questions arise: What if the offset is set erroneously at 43° from the steepest meridian instead of the flattest (effectively offsetting by 133°)? What if it is set at 45°? (Convenient on the Perkins tonometer which does not have a 43° marker).
These questions are answered by figure 7. In the range from zero to six dioptres of corneal astigmatism (a range more likely in normal optometric practice) there is overestimation in both cases but only of a small amount. Indeed, the 45° offset offers even better accuracy than the 43° offset within this range.
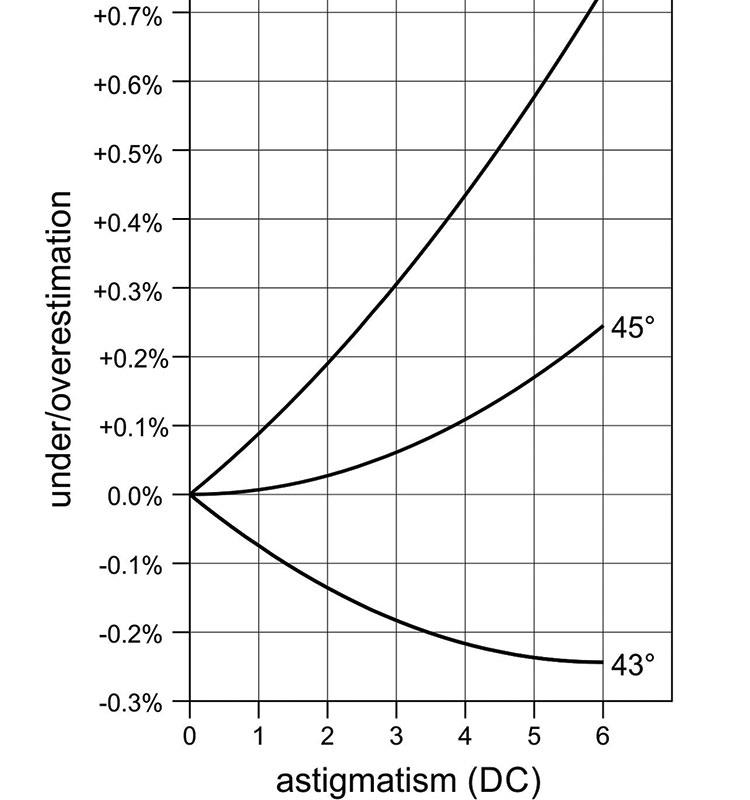
Figure 7: Error values for different Goldmann offset angles (133° is 43° offset from the ‘wrong’ principal meridian)
Finally, situations arise in practice where applanation tonometry is undertaken without prior knowledge of the status of corneal astigmatism. As we have already seen in the worst case scenarios, this can result in small but significant under or over-estimation. However, to minimise this error it has been suggested readings be taken with the probe aligned at 180° and repeated at 90° with the average taken as the IOP measurement.1 This procedure does not completely eliminate the measurement error but nevertheless it does reduce it to the same amount as if using a 45° offset (assuming the IOP does not change between readings).
Caveats
The foregoing was predicated on the assumption that the applanation patch on an astigmatic cornea is a mathematically perfect ellipse. It is certainly oval and unlikely to be very different from a true ellipse in view of its low degree of non-circularity even in high astigmatism.
No account has been taken here of the effect of the tear film meniscus in Goldmann tonometry. It is well known that too much or too little tear fluid significantly affects the accuracy of Goldmann readings. In the situations of under or over-estimation described earlier, the perimeter of the applanation patch differs from the ideal. This will inevitably affect the hydrostatic forces associated with the tear film meniscus. However, it is beyond the scope of this brief article (and its author’s ability) to calculate the influence of this factor.
Conclusions
The biggest potential source of error is misplacement from the centre. The applanation patch should be bisected evenly by the Goldmann probe. The 43° offset is a highly effective means of minimising measurement error on astigmatic corneas. Indeed, there seems to be no good reason to not apply it universally and not just in cases exceeding three dioptres of astigmatism. A 45° offset is also very effective and marginally more accurate when corneal astigmatism is less than six dioptres.
Henry Burek is an optometrist practicing in South Yorkshire and an examiner for the College Of Optometrists.
References
1 Akram, Amjad et al. Pitfalls in Intraocular Pressure Measurement by Goldmann-Type Applanation Tonometers. Pak J Ophthalmol 2009, Vol. 25 No. 4
2 Haag-Streit. Instructions for use: Applanation tonometer AT 900 / 870 .Edition 2014-11
3 Burek, H. Misplacement Errors In Goldmann Tonometry. youtu.be/A6Hbu1gYaPc. 2016
