In Part 3 (21.03.14) I looked at establishing the best sphere. The next step is to establish the extent and orientation of any astigmatism correction. Using the Jackson cross-cylinder, (or cross-cyl as it is more commonly known and shall be referred to for the rest of this article) or the fan-and-block technique can determine the cylindrical component of the refractive error.
The cross-cylinder
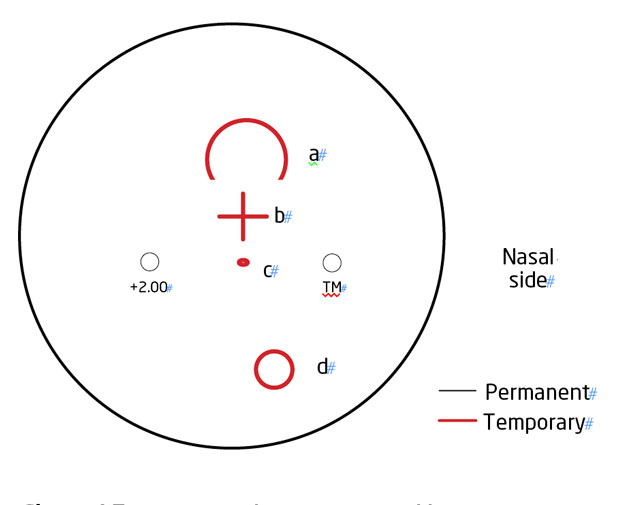
The cross-cyl can be described as ‘a fixed arrangement of a plus and a minus cylinder, axes perpendicular, with a handle placed between the two axes’ (Figure 1).
Various cross-cyl powers are accessible dependent on the patient’s acuity. Coloured markings can be found on the cross-cyl that represent the plus and minus cylinder axes. The lens can be held in various orientations to determine the cylinder power and axis.
For the purpose of this article we will assume that the negative cylinder axis is demarked by a red mark and the positive cylinder axis by a black mark (which is typical though not exclusively the case).
[CaptionComponent="2677"]
Cross-cylinder procedure (with a cylindrical lens in place following retinoscopy)
Check the cylinder axis
? Choose an appropriate target and cross-cyl lens power before conducting the cross-cyl technique. (See the later section on cross-cyl)
? Before commencing, ensure the circle of least confusion (CLC, as explained in Part 3 – 21.03.14) is appropriately positioned
? Checking the cylinder axis: hold the handle of the cross-cylinder parallel to the axis of the cylinder lens in the trial frame resembling that shown in Figure 2 (eg axis of lens is at 180°).
? Ask the patient to look at the distance target selected for cross-cyl; explain to them that you will be showing them two lenses which they will compare (Figures 3a and 3b)
[CaptionComponent="2678"]
? Twirl the cross-cyl handle through 180 degrees and ask the patient if the target looks clearer and sharper with ‘lens one’ or ‘lens two’ or ‘if no difference is seen’. Depending on which lens the patient prefers, rotate the axis of the negative cylinder lens in the trial frame towards the negative axis of the cross-cyl by about 10 degrees (Figure 4)
? Reposition your cross-cyl handle so that it is now in line with the new axis (eg 170°) and repeat the procedure described above, continually changing the axis until no difference is reported between lens 1 and 2
? If the patient reports no difference in target clarity when the two lenses are shown initially, this suggests that the cylinder axis found after retinoscopy was correct and therefore does not need to be altered. Remember that the end point is when the two images appear similar, even if not very sharp. Some patients find this confusing so be prepared to explain.
Check the cylinder power
? Now hold the handle of the cross-cylinder at 45 degrees to the cylinder axis in the trial frame, so that the axis of the cross-cylinder is parallel with the axis of the cylinder in the trial frame (Figure 5)
? Twirl the cross-cylinder through 180 degrees and ask the patient if the target looks clearer and sharper with lens 1 or lens 2 or if no difference is seen
? If the patient reports that the target is clearer with the negative axis of the cross-cylinder superimposed on the axis of the cylinder in the trial frame, increase the negative power of the cylinder. If alternatively the patient reports that the circles are clearer when the positive axis of the cross-cylinder is superimposed on the cylinder axis in the trial frame, then reduce the negative power of the cylinder
? Repeat the procedure described above until no difference is reported between lens 1 and lens 2.
Checking the cross-cylinder procedure (without a cylindrical lens in place following retinoscopy)
? Hold the appropriate cross-cyl selected (see notes below on cross-cyl selection) in front of the right eye with its handle at 45° so that the negative axes of the cross-cyl (red marker) is presented along the horizontal (180°) and vertical meridians (90°) in turn
? Ask the patient if the target looks clearer and sharper with ‘lens 1’ (negative axis at 180°) or ‘lens 2’ (negative axis at 90°). If, in this example, when presented with the two lenses the patient prefers the
-ve cyl axis (red marker) at 180°, this suggests that there is some astigmatism present and its axis is closer to 180° than 90°
? Now hold the cross-cylinder handle at 180° so that the negative axes of the cross-cyl (red marker) is presented along the diagonal (45° and 135°) meridians in turn
? Ask the patient if the target looks clearer and sharper with ‘lens 1’ (negative axis at 45°) or ‘lens 2’ (negative axis at 135°). If, in this example, the patient prefers the -ve cyl axis at 45°, this suggests that the axis of the astigmatism is closer to 45° than 135°. Coupled with the previous information, the cylinder axis lies somewhere between 180° and 45°
? Now place a -0.25DC (or higher power -0.50 to -0.75DC depending on the level of visual acuity at this point) anywhere between axis 180° and 45° and repeat the procedure described above in ‘checking the cyl axis and power following ret’ from step 3 to 4.
The fan-and-block
[CaptionComponent="2679"]
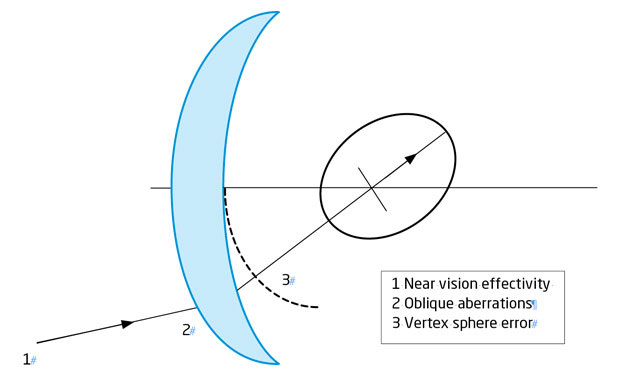
The fan-and-block technique for measuring astigmatism is less utilised in practice nowadays because it is said to be less sensitive at determining small cylinders, it is not reliable for determining astigmatism >2.50D, a person with a head tilt will not give accurate results and some modern projector and computerised charts simply do not have the appropriate fan-and-block target (Figure 6) built in for the assessment of astigmatism. It is, however, useful for detecting irregular astigmatism and an alternative method for checking the presence of astigmatism when poor or unexpected responses are obtained with the cross-cyl test.
Fan-and-block subjective procedure following retinoscopy
? Measure the PD and fit the trial frame on your patient so that it is comfortable
? Perform retinoscopy on both eyes and allow for your working distance if not already done so with a working distance allowance lens. Record your results
? Measure the visual acuity of both eyes after retinoscopy
? Starting with the right eye (left eye occluded), remove the cylinder lens found on retinoscopy from the trial frame
? Determine the best vision sphere (BVS) as described in the simultan technique (see Optician 21.03.14)
– If the acuity is 6/18, use larger dioptric steps so that the patient can appreciate changes in the acuity
–The expected BVS will be half of the cylinder power, for example for -3.00DC expect the BVS to be -1.50DS
? Check duochrome and ensure that both targets are equal
? Direct the patient to the fan-and-block chart. Ask the patient if any of the lines of the fan appear clearer or more distinct
? While looking at the fan, add a fogging lens of spherical power (approximately equal to half of the cylinder power), until the patient reports that all the lines of the fan are now blurred/not clear. Now reduce the spherical fogging lens power by -0.25DS
? To determine the principal meridians, rotate the arrow situated under the fan to the point (or the centre of a group of points) at which the patient reports the lines of the fan appear clearest. Continue fine adjustments of the arrow until both of its limbs are equally clear. This point indicates the negative cylinder axis
? Insert half of the negative cylinder that you found on retinoscopy at the axis found in the previous step and direct the patient to now look at the blocks situated under the arrow
? Ask the patient, which of the blocks appear clearer/blacker. If the block with the lines going in the same direction as the cyl axis appear clearer, increase the cylinder power by -0.25; if, however, the block with the lines going in the opposite direction is the clearest, reduce the cylinder power by +0.25. Continue adding negative or positive cylinders until both blocks are reported to be equally clear. For every 0.50DC change in cylinder power adjust the sphere power by 0.25DS.
? Recheck the cyl axis by asking the patient if all the lines on the fan and both limbs of the arrow are equally clear. If not, it means that the cylinder axis is incorrect and the cylinder axis in the trial frame needs to be adjusted.
The final sphere check may now be carried out.
Final sphere check
Once the astigmatic correction has been checked, the best vision sphere (BVS) should be rechecked to ascertain if any refinement in the spherical component is required following cross-cyl.
Procedure for rechecking the BVS following cross-cyl
? Direct the patient to view the best line of acuity they can read. Add +0.25DS and ask the patient if the letters are clearer, more blurred or the same
? If the patient reports that the letters are better or the same add +0.25DS. Continue to add +0.25DS until the patient sees no improvement in the acuity.
– Offer maximum positive sphere or minimum negative sphere.
? If the visual acuity blurs with the +0.25DS in the first instance, add -0.25DS. Only add negative spheres if an improvement in the line of acuity is seen, ie the patient reads more letters than previously recorded.
+1 blur check
This test is carried out to verify whether the spherical component of the spectacle prescription is correct and the patient has not been over-minused or under-plussed. It is also a precursor to binocular balancing of accommodation (Humphriss immediate contrast or HIC) following a monocular refraction described later in this article.
Traditionally a +0.75DS or +1.00DS lens is used, as it helps to relax accommodation and suppresses the central vision while maintaining peripheral vision. The visual acuity with the +1.00DS blur should reduce to 6/12-6/18, if this does not occur, it suggests that the best vision sphere is not at its end point and needs to be rechecked.
Procedure for checking +1 blur
? Following BVS, cross-cyl and acuity check, inform the patient that you will be placing a lens in front of their right eye that will/may blur the letters on the chart
? While the left eye is still occluded, place a +1.00DS lens in front of the right eye
? Ask the patient what the lowest or clearest line of letters is that they can now read
? The visual acuity should blur back to about 6/12-6/18 (or around three lines worse acuity) and this is the correct end point
? If it does not, remove the +1.00DS lens and recheck the best vision sphere pushing maximum plus and minimum minus
? Replace the +1.00DS blur lens in front of the right eye and ensure appropriate blur as with other eye
? Occlude the right eye and repeat the procedure for the left eye
? Record the visual acuity for both eyes.
Binocular balancing using Humphriss immediate contrast (HIC)
Binocular balancing is essentially the name given to describe the method of balancing the accommodative status of the two eyes while viewing a distance target binocularly.
The HIC method of binocular balancing is usually favoured, as the eyes remain in their normal binocular state with little dissociation and the fogging lens added during the technique helps to relax the accommodation.
Performing binocular balancing is not necessary on patients who are monocular, have little or no accommodation or if a binocular refraction has been performed.
Procedure for binocular balancing
? Perform the +1.00DS blur check in both eyes consecutively as described earlier and ensure that equal blur back has been achieved in both eyes
? Leave the +1.00DS lens in the left eye, ensuring the occluder is removed from both eyes. Inform the patient that you have ‘blurred’ or ‘fogged’ the left eye intentionally but they should keep both eyes open during this test. Where equal blur back has not/is not possible eg due to unequal visual acuities, the +1.00DS lens should be placed in front of the ‘worst eye’ first
? Starting with the right eye, ask the patient to read the lowest line of letters they can see clearly. Add +0.25DS and ask them if the letters appear clearer, more blurred or the same. If the patient reports that the letters are better or the same, add +0.25DS. Continue to present and add +0.25DS until the patient sees no improvement in the acuity or it just blurs
? If the visual acuity blurs with the +0.25DS in the first instance, offer -0.25DS. Only give negative spheres if an improvement in the line of acuity is seen, ie the patient reads more letters than previously recorded
? Remove the +1.00DS lens and now place it in front of the right eye. Repeat the procedure as described above from 3-4 for the left eye.
Binocular addition
Binocular addition is the process of checking the maximum plus sphere that can be given to the patient binocularly.
Procedure for binocular addition
? Following +1.00Blur and HIC test, ask the patient to read the lowest line of letters they can see clearly on the chart with both eyes together
? Add +0.25DS in front of both eyes binocularly and ask the patient if the letters are clearer, more blurred or the same
? If the patient reports that the letters are better or the same, add +0.25DS binocularly. Continue to present and add +0.25DS binocularly until the patient sees no improvement in the acuity or it just blurs
? If the visual acuity blurs with the presentation of the initial +0.25DS binocularly do not give it.
Binocular VA
Where applicable, the binocular acuity should always be recorded; it can be particularly indicated in specific situations such as nystagmus where the binocular acuity will be better than the monocular measurement and for occupational and driving standards where recording binocular visual acuity is necessitated.
Procedure for checking binocular vision/visual acuity
? Following monocular acuity testing, ask the patient to read the lowest line of letters they can see clearly on the chart with both eyes open/unoccluded.
Recording results
The end results following subjective refraction should be recorded detailing, at a minimum, the final spherical and cylindrical lens power/axis, the monocular visual acuity and the binocular visual acuity. More detailed record cards may also note the +1blur result, binocular addition and binocular balancing results.
Example of recording final refraction results:
RE: -2.00/-0.50 x180 VA 6/5 +1B 6/12 (Binocular Bal +0.25DS)
LE: -2.50/-0.50 x10 VA 6/5 +1B 6/12 Binoc Add ?
Binoc VA 6/4
Final prescription issued:
RE: -1.75/-0.50 x 180
LE: -2.25/-0.50 x 10.
Conclusion
Figure 7 offers a flow chart summary of the monocular subjective procedure. The goal of a subjective refraction is to measure and improve a patient’s visual function by means of patient and practitioner interaction. It relies heavily on good communication and a well-structured routine to maximise patient response and comfort. A subjective routine should flow effortlessly and have a logical progression. Always ensure you explain the test procedures to the patient and what they may expect to, where possible, experience. Be prepared to modify your routine for patients where communication is limited or responses are not reliable. In the next article I will take a look at binocular techniques and some adaptations to subjective procedure for patients with poor acuity.
? Tina Patel is an optometrist working in hospital and private clinics and is an examiner and assessor for the College of Optometrists
Model answers
(The correct answer is shown in bold text)
1 Which of the following statements about cross-cyl is true?
A It can only be done with a cylinder lens in the trial frame
B It is more sensitive for assessing lower cylinder values than fan-and-block
C It is susceptible to error due to head tilt
D It should not be used in low vision practice
2 How might one adjust the sphere of a 68 year old patient prior to cross-cyl?
A Put in -0.25DS after checking the best vision sphere
B Add sphere to leave on the green
C Put in +0.25
D Use the best vision sphere
3 A patient accepts -1.00DC when checking the power with cross-cyl. This is accepted in -.025DC steps. What change should be made to the sphere?
A None as long as the best vision sphere has been used
B For every -0.50DC step the sphere should be adjusted by +0.25DS
C For every -0.25DC step the sphere should be adjusted by +0.25DS
D For every -0.50DC step the sphere should be adjusted by +0.50DS
4 What is meant by the term bracketing?
A Selecting a midpoint answer between two confirmed responses either side of a result about which there is uncertainty
B Forcing the patient to select a specific answer option
C Using two different cross-cyls of differing powers
D Comparing responses when two different cylinder lenses are superimposed
5 For an end point acuity of 6/4.5, what might the expected acuity be through a +1.00DS lens?
A 6/18
B 6/15
C <6/18
D Three lines worse acuity
6 Which of the following statements about Humphriss immediate contrast method of balancing is true?
A It is suitable for all patients
B It is essential in presbyopes as a way of assessing differences in depth of focus
C It is not required after binocular refraction
D It may still be useful in monocular patients as a check test